Abstract
Aims/hypothesis
Mice that are deficient for complement factor 3 (C3) have shown resistance to weight gain, despite increased food intake. Cross-sectional studies of humans have reported correlations between C3 and obesity. This longitudinal study explored whether C3 predicts a large weight gain in middle-aged men.
Methods
Plasma concentrations of C3 and complement factor 4 (C4) were measured in 2,706 non-diabetic healthy men aged between 38 and 50 years, who were re-examined after a mean period of 6.1 years.
Results
After adjustments for initial weight, age, height and follow-up time, the odds of incurring large weight gain (75th percentile, ≥3.8 kg) were 1.00 (reference), 0.96 (95% CI:0.7–1.2), 1.1 (CI:0.9–1.5) and 1.4 (CI:1.1–1.8), respectively, among men with C3 levels in the first, second, third and fourth quartiles (p for trend=0.01) respectively. This relationship remained significant after further adjustments for lifestyle factors (physical inactivity, alcohol, smoking), metabolic factors (glucose or homeostasis model assessment values, cholesterol, triglycerides), inflammatory markers (fibrinogen, haptoglobin, ceruloplasmin, orosomucoid, α1-antitrypsin) and for C4. C4 was associated with weight gain after adjustments for initial weight, height, follow-up time and lifestyle factors, but not after adjustments for C3.
Conclusions/interpretation
C3 is a risk factor for incurring large weight gain in middle-aged men.
Similar content being viewed by others
Introduction
Complementary factors 3 and 4 (C3, C4) are the major plasma proteins of the complement pathway of the immune system. The synthesis of these proteins increases in response to inflammation and infection, with a slower increase than the traditional acute-phase proteins [1–3]. Although hepatic production is the main source of these proteins, C3 and C4 are also expressed and secreted by other cells, for example, in adipose tissue [4, 5].
Individuals who are overweight or obese generally have raised concentrations of C3 and C4 [4–10], and it has been reported that C3 levels decrease after weight loss [6, 7]. The proteolytic fragment of C3, acylation-stimulating protein (ASP), is a paracrine metabolic factor that stimulates the uptake of glucose and fat storage in human adipose tissue [11–14]. Knock-out mice that are deficient for C3 and ASP show resistance to weight gain on a high-fat diet, despite increased food intake [11, 14]. However, no prospective study has investigated the relationship between C3 and weight gain in humans.
Previous studies from the present cohort have shown that raised concentrations of fibrinogen, haptoglobin, ceruloplasmin, orosomucoid and α1-antitrypsin are associated with weight gain [15]. However, the correlations between levels of C3 and levels of these inflammatory markers are small and we recently reported that C3 is associated with incidence of diabetes independently of these proteins [16]. Based on the findings from animal models, we explored the hypothesis that C3 could be associated with future weight increase independently of other inflammatory markers.
Subjects, materials and methods
Subject recruitment and study protocol
Between 1974 and 1984, 22,444 men participated in a screening programme for the detection of those at high risk for cardiovascular diseases. Complete birth cohorts from the city of Malmö were invited [17] and the participation rate was 71%. Plasma protein determination was part of the programme for 6,193 men who were selected at random from cohorts examined between 1974 and 1982. After the exclusion of men with diabetes or a history of myocardial infarction, stroke or cancer (according to questionnaire), 5,729 men remained.
A follow-up examination was performed after a mean follow-up of 6.1±0.93 years (range 3.0–9.0). Of the screened birth cohorts, men born between 1926 and 1931 and in 1938 (aged 38–50 years at baseline) were invited to the follow-up. A total of 2,822 participated, representing 81% of those who were alive in 1982 when the re-examinations started. Measurements of C3 and C4 were available for 2,706 and 2,704 of these men, respectively. The sample in the present study thus consists of 2,706 healthy men, aged 38–50 years at baseline, who were re-examined after a mean period of 6.1 years.
The health service authority of Malmö approved and funded the screening programme and all participants gave their informed consent.
Baseline examinations
Diabetes was defined as fasting whole blood glucose ≥6.1 mmol/l, 2-h glucose ≥10.0 mmol/l (glucose load: 30 g/m2 body surface area), or self-reported diabetes.
Information about fasting insulin was available in a subgroup of 1,907 men. Insulin (mIU/l) was measured with a non-specific radioimmunoassay [18]. The homeostasis model assessment (HOMA) formula according to Matthews et al. [19], i.e. (fasting insulin×fasting glucose)/22.5, was used to calculate a score for insulin resistance.
Subjects were placed in two categories: smokers and non-smokers. Physical inactivity was assessed in a questionnaire at baseline and at follow-up. Men who reported that they were mostly sedentary in their spare time were categorised as physically inactive. Some items of the questionnaire were changed before the end of the follow-up period. At the follow-up examination, physical inactivity was therefore defined either as those who were mostly sedentary in their spare time or those who reported that they did not perform physical activity in their spare time (e.g. walking, cycling) regularly every week. Alcohol consumption was assessed using the modified shortened version of the Michigan Alcoholism Screening Test [20]. Men with more than two (of nine) affirmative answers were considered to be high-consumers of alcohol.
Weight was measured in the morning with the subject wearing light indoor clothing and no shoes. Weight increase (in kg) was calculated as weight at baseline subtracted from the follow-up value. A large weight gain was defined as one on or above the 75th percentile (>3.8 kg) [15].
Plasma proteins
Electroimmunoassay was used to assess the concentrations of plasma proteins [21]. The coefficient of variation was <5% [21]. The analyses were performed consecutively at the study entry. C3 and C4 were originally expressed as the percentage of the mean values from a reference population of blood donors. The reference values for C3 were 70–130%, which corresponds to 0.67–1.29 g/l, and the reference values for C4 were 65–170% (0.13–0.32 g/l). To facilitate the interpretation of the C3 and C4 values, the percentages have been converted into g/l (C3:100%=0.98 g/l, C4:100%=0.20 g/l). The distributions of the other plasma proteins (fibrinogen, haptoglobin, ceruloplasmin, orosomucoid, α1-antitrypsin) have been presented elsewhere [22]. The correlation between C3 and C4 was r=0.47 and the correlations between C3 and the other proteins were all below 0.3 in this cohort [16].
Statistics
One-way analysis of variance and the Mantel–Haenzel χ 2 test were used to compare the risk factors by quartiles of C3. Pearson’s correlation was used for two continuous variables. A general linear model was used to compare weight at follow-up in quartiles of C3, with adjustments for confounding factors. Logistic regression was used to study the proportion of men with large weight gain in relation to plasma protein levels. The relationships between C3 and weight gain were adjusted for initial weight in all calculations. Two-tailed p values <0.05 were considered statistically significant.
Results
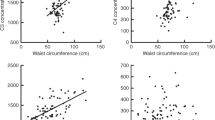
The baseline and follow-up characteristics by quartiles of C3 are presented in Table 1. BMI and weight were substantially higher in men with high C3. The proportion of smokers was somewhat lower in men with high C3 (Table 1). However, C3 showed no association with smoking after adjustments for BMI (data not shown).
Weight at baseline was inversely correlated with weight increase during the follow-up (r=−0.17, p<0.0001). The proportion with a large weight gain (>3.8 kg) was 24.1% in men with low concentrations of C3 (1st quartile), and 25.9% in men with high concentrations of C3 (4th quartile). However, when weight at baseline, age, height and follow-up time were taken into account, a large weight gain was significantly associated with C3 at baseline (Table 2). This relationship remained significant after further adjustments for lifestyle factors (Model 2: +smoking, physical activity, alcohol consumption), metabolic factors (Model 3: +glucose, cholesterol, triglycerides), and inflammation-sensitive proteins (ISPs) (Model 4: +fibrinogen, ceruloplasmin, α1-antitrypsin, orosomucoid, haptoglobin). The results also remained significant after adjustments for C4. The relationships were similar when C3 was used as a continuous variable (per SD) (Table 2).
Weight at follow-up showed similar associations with C3 after adjustments for initial weight (Table 2). C3 was significantly associated with weight at follow-up after adjustments for inflammatory markers (Model 4). After further adjustments for C4, this association was of borderline significance (p=0.06).
Weight loss >1.2 kg (lowest quartile of weight gain) was not associated with C3 after adjustment for initial weight (Table 2).
The results were identical if weight increase (initial weight subtracted from weight at follow-up) was used instead of weight at follow-up. The results were also identical if BMI was used to assess weight and weight increase (not shown). The results were essentially unchanged after exclusion of 117 subjects who developed diabetes during the follow-up period (not shown).
The relationships between C3 and weight gain were largely consistent over the quartiles of BMI. The relationships were somewhat weaker in smokers than in non-smokers or in smokers who gave up smoking during the follow-up period (Table 3).
Subgroup with HOMA-values
Information about HOMA was available for a subgroup of 1,907 men. The relationship with large weight gain was studied in this subgroup, with and without adjustments for HOMA (log-transformed). After adjustments for initial weight, age, height, follow-up time, lifestyle, and metabolic factors (Model 3), the odds ratios for a large weight gain were 1.00, 1.1 (0.8–1.6), 1.2 (0.9–1.7) and 1.56 (1.1–2.2) respectively for C3 levels in the first, second, third and fourth quartiles (p for trend=0.008). Odds ratio (OR) per 1 SD increase in C3 was 1.17 (1.04–1.32, p=0.007). When HOMA was added to the model, the ORs were 1.00, 1.1 (0.8–1.6), 1.2 (0.9–1.7), and 1.54 (1.1–2.1), respectively (p for trend: 0.009). OR per 1 SD was 1.17 (1.04–1.31, p=0.01). These relationships remained significant after further adjustments for ISPs (Model 4).
The relationship between C3 and weight at follow-up was significant after adjustments for lifestyle, metabolic factors (Model 3) and HOMA (adjusted mean+standard error, 78.1+0.20, 78.3+0.22, 78.3+0.20 and 78.8+0.21 kg, respectively, for the quartiles of C3 concentration, p for trend <0.05). After further adjustments for inflammatory proteins, this association did not reach significance in this subgroup (p for trend=0.11).
ISPs and C4
Table 4 presents the relationships between a large weight gain and the number of ISPs in the top quartile. The risk of a large weight gain was significantly associated with the number of elevated ISPs, and this relationship remained significant after adjustments for C3 and C4.
Table 5 presents the relationship between C4 and a large weight gain. C4 was associated with weight gain after adjustments for initial weight, follow-up time and lifestyle factors. However, there was no association between C4 and weight gain after adjustments for C3. This relationship was similar when C4 was used as a continuous variable (not shown).
Discussion
Cross-sectional studies have shown that obesity is associated with elevated plasma levels of C3 [4, 6–10], but the causal and temporal relations of this association have been unclear. The present study showed that C3 was strongly associated both with weight at baseline and weight at follow-up. When adjusting for initial weight, C3 was significantly associated with an increased risk of developing a large weight gain. To our knowledge, this is the first study linking C3 to future weight gain in humans.
Although the causes of obesity are multifactorial, increasing evidence links inflammation and infections to obesity or weight gain [23–28]. Seropositivity for Chlamydia pneumoniae has been associated with high BMI in humans [28] and in mice virus infections have been associated with weight gain [27]. Elevated levels of fibrinogen, white blood cells, von Willebrand factor or factor VIII, i.e. four putative markers of inflammation, have been associated with large weight gain in a large cohort study [26]. A study from this cohort showed that high levels of fibrinogen, ceruloplasmin, α1-antitrypsin, orosomucoid and haptoglobin were associated with weight gain [15]. However, C3 shows only modest correlations with these inflammatory markers (all r<0.3) [16]. The relationship between C3 and weight gain was essentially unchanged after adjustment for inflammatory proteins and, conversely, the number of elevated ISPs was associated with weight gain even after adjustments for C3. Hence, the relationship between C3 and weight gain cannot be explained by inflammation as measured by these acute-phase proteins. Thus C3 and the ISPs could represent different pathways of weight gain.
Another question is whether the relationships are specific for C3 or whether other complement components are also associated with weight gain. Data on C4 were available in this study and the correlation between C3 and C4 was approximately r=0.5. The relationship between C3 and weight gain was slightly reduced after adjustments for C4. In contrast, the relationship between C4 and weight gain became clearly non-significant after adjustment for C3. Hence, the association between C4 and weight gain seems to be explained by its relationship with C3.
ASP is a possible link between C3 and weight gain. This hormone has autocrine or paracrine effects and is produced in the adipose tissue by conversion from C3 [11]. It has been shown that ASP stimulates the storage of fat in human adipocytes, inhibits intracellular lipolysis and increases plasma clearance of triglycerides [11–13]. ASP also stimulates the disposal of glucose by increasing the release of insulin [29]. Mice with C3 and ASP deficiencies show resistance to weight gain despite increased food intake [14]. These animals also have increased energy expenditure [30]. However, it is unclear to what extent circulating C3 reflects the concentrations in the adipose tissue. As local effects in the adipose tissue are probably most important, circulating levels of C3 could be a crude proxy for the local effects.
The hepatic synthesis of C3 is stimulated by various cytokines, e.g. IL-1 and TNF-α [31]. These cytokines are also involved in the regulation of metabolism and food intake. For example, TNF-α and IL1-β decrease the production and expression of leptin, an anorexigenic hormone formed in the adipose tissue [32]. Polymorphisms of the genes encoding TNF-α receptor have been associated with leptin-resistance and obesity [33, 34]. In studies of rodents, injection of TNF-α and IL-1 initially reduces food intake. However, tolerance soon develops after repetitive administration of TNF-α [35]. The relation between plasma C3 and weight gain could hypothetically reflect the effects of these cytokines.
We had no information on diet in this cohort. It is unclear whether the relations between weight and C3 could reflect dietary factors that increase C3. It has been reported that intake of lipids and proteins could induce oxidative stress [36], which hypothetically could increase inflammation. On the other hand, studies of C3 levels before and after food intake have not shown any consistent differences. Two studies reported no postprandial changes [37, 38], while another study showed a small increase [39]. Since the plasma samples were drawn after an overnight fast, this probably reduced the effects of food intake.
The participant rates were high and the procedures were identical at both examinations. As smoking cessation is associated with weight gain, smoking is a potential confounder. However, smoking was not associated with C3 after body weight had been taken into account and the relation between C3 and weight gain persisted after adjustments for current and former smoking and smoking cessation during follow-up. Physical activity is another factor that could affect weight gain. The results were adjusted for physical inactivity both at baseline and at follow-up. However, only two categories of physical activity were used and it is possible that the variables did not pick-up all effects of physical activity.
Another limitation is that only men were included in the study. Apart from cytokine stimulation of C3 synthesis, C3 concentrations are determined by immune-complex deposition, genetic factors and female sex hormones [40]. It is not known whether the relation between C3 and weight gain is similar in women.
High levels of C3 are a risk factor for incurring large weight gain. The reasons for this association remain to be explored.
Abbreviations
- ASP:
-
acylation-stimulating protein
- C3:
-
complement factor 3
- C4:
-
complement factor 4
- HOMA:
-
homeostasis model assessment
- ISPs:
-
inflammation-sensitive plasma proteins
- OR:
-
odds ratio
- Q:
-
quartile
- SE:
-
standard error
References
Ritchie RF, Palomaki GE, Neveux LM, Navolotskaia O, Ledue TB, Craig WY (2004) Reference distributions for complement proteins C3 and C4: a practical, simple and clinically relevant approach in a large cohort. J Clin Lab Anal 18:1–8
Moshage H (1997) Cytokines and the hepatic acute phase response. J Pathol 181:257–266
Walport MJ (2001) Complement. First of two parts. N Engl J Med 355:1058–1066
Gabrielsson BG, Johansson JM, Lönn M et al (2003) High expression of complement components in omental adipose tissue in obese men. Obes Res 11:699–708
Xia Z, Cianflone K (2003) Acylation-stimulating protein precursor proteins in adipose tissue in human obesity. Metabolism 52:1360–1366
Pomeroy C, Mitchell J, Eckert E, Raymond N, Crosby R, Dalmasso AP (1997) Effect of body weight and caloric restriction on serum complement proteins, including factor D/adipsin: studies in anorexia nervosa and obesity. Clin Exp Immunol 108:507–515
Hanusch-Enserer U, Cauza E, Spak M et al (2003) Acute-phase response and immunological markers in morbid obese patients and patients following adjustable gastric banding. Int J Obesity 27:355–361
Weyer C, Tataranni PA, Pratley RE (2000) Insulin action and insulinemia are closely related to the fasting complement C3, but not acylation stimulating protein concentration. Diabetes Care 23:779–785
Muscari A, Bozzoli C, Puddu GM et al (1995) Association of serum C3 levels with the risk of myocardial infarction. Am J Med 98:357–364
Peake PW, Kriketos AD, Campbell LV, Charlesworth JA (2005) Response of the alternative complement pathway to an oral fat load in first-degree relatives of subjects with type II diabetes. Int J Obes Relat Metab Disord 29:429–435
Cianflone K, Xia Z, Chen LY (2003) Critical review of acylation-stimulating protein physiology in humans and rodents. Biochim Biophys Acta 1609:127–143
Maslowska M, Sniderman AD, Germinario R, Cianflone K (1997) ASP stimulates glucose transport in cultured human adipocytes. Int J Obes Relat Metab Disord 21:261–266
Van Harmelen V, Reynisdottir S, Cianflone K et al (1999) Mechanisms involved in the regulation of free fatty acid release from isolated human fat cells by acylation-stimulating protein and insulin. J Biol Chem 274:18243–18251
Xia Z, Sniderman AD, Cianflone K (2002) Acylation-stimulating protein (ASP) deficiency induces obesity resistance and increased energy expenditure in ob/ob mice. J Biol Chem 277:45874–45879
Engström G, Hedblad B, Stavenow L, Lind P, Janzon L, Lindgärde F (2003) Inflammation-sensitive plasma proteins are associated with future weight gain. Diabetes 52:2097–2101
Engström G, Hedblad B, Eriksson KF, Janzon L, Lindgärde F (2005) Complement C3 is a risk factor for the development of diabetes. A population-based cohort study. Diabetes 54:570–575
Berglund G, Eriksson KF, Israelsson B et al (1996) Cardiovascular risk groups and mortality in an urban Swedish male population: the Malmö preventive project. J Intern Med 239:489–497
Thorell JI, Larson SM (1978) Radioimmunoassay and related techniques. CV Mosby Company, St Louis, pp:205–211
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC (1985) Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 28:412–419
Kristenson H, Trell E (1982) Indicators of alcohol consumption: comparisons between a questionnaire (Mm-MAST), interviews and serum gamma-glutamyl transferase (GGT) in a health survey of middle-aged males. Br J Addict 77:297–304
Laurell CB (1972) Electroimmunoassay. Scand J Clin Lab Invest Suppl 124:21–37
Engström G, Lind P, Hedblad B, Stavenow L, Janzon L, Lindgärde F (2002) Effects of cholesterol and inflammation-sensitive plasma proteins on incidence of myocardial infarction and stroke in men. Circulation 105:2632–2637
Engström G, Hedblad B, Stavenow L et al (2004) Incidence of obesity-associated cardiovascular disease is related to inflammation-sensitive plasma proteins: a population-based cohort study. Arterioscler Thromb Vasc Biol 24:1498–1502
Wlodek D, Gonzales M (2003) Decreased energy levels can cause and sustain obesity. J Theor Biol 225:33–44
Das UN (2001) Is obesity an inflammatory condition? Nutrition 17:953–966
Duncan BB, Schmidt MI, Chambless LE, Folsom AR, Carpenter M, Heiss G (2000) Fibrinogen, other putative markers of inflammation, and weight gain in middle-aged adults-the ARIC study. Obes Res 8:279–286
Dhurandhar NV (2001) Infectobesity: obesity of infectious origin. J Nutr 131:2794S–2797S
Dart AM, Martin JL, Kay S (2002) Association between past infection with Chlamydia pneumoniae and body mass index, low-density lipoprotein particle size and fasting insulin. Int J Obes Relat Metab Disord 26:464–468
Ahren B, Havel PJ, Pacini G, Cianflone K (2003) Acylation stimulating protein stimulates insulin secretion. Int J Obes Relat Metab Disord 27:1037–1043
Xia Z, Stanhope KL, Digitale E et al (2004) Acylation-stimulating protein (ASP)/complement C3adesArg deficiency results in increased energy expenditure in mice. J Biol Chem 279:4051–4057
Andrews E, Feldhoff P, Feldhoff R, Lassiter H (2003) Comparative effects of cytokines and cytokine combinations on complement component C3 secretion by HepG2 cells. Cytokine 23:164–169
Bruun JM, Pedersen SB, Kristensen K, Richelsen B (2002) Effects of pro-inflammatory cytokines and chemokines on leptin production in human adipose tissue in vitro. Mol Cell Endocrinol 190:91–99
Pausova Z, Deslauriers B, Gaudet D et al (2000) Role of tumor necrosis factor-α gene locus in obesity and obesity-associated hypertension in French Canadians. Hypertension 36:14–19
Fernandez-Real JM, Vendrell J, Ricart W et al (2000) Polymorphism of the TNF-α receptor 2 gene is associated with obesity, leptin levels, and insulin resistance in young subjects and diet-treated type 2 diabetic patients. Diabetes Care 23:831–837
Argiles JM, Busquets S, Lopez-Soriano FJ (2003) Cytokines in the pathogenesis of cancer cachexia. Curr Opin Clin Nutr Metab Care 6:401–406
Dandona P, Mohanty P, Ghanim H et al (2001) The suppressive effect of dietary restriction and weight loss in the obese on the generation of reactive oxygen species by leukocytes, lipid peroxidation, and protein carbonylation. J Clin Endocrinol Metab 86:355–362
Charlesworth JA, Peake PW, Campbell LV, Pussell BA, O’Grady S, Tzilopoulos T (1998) The influence of oral lipid loads on acylation stimulating protein (ASP) in healthy volunteers. Int J Obes Relat Metab Disord 22:1096–1102
Koistinen HA, Vidal H, Karonen SL et al (2001) Plasma acylation stimulating protein concentration and subcutaneous adipose tissue C3 mRNA expression in nondiabetic and type 2 diabetic men. Arterioscler Thromb Vasc Biol 21:1034–1039
Halkes CJ, van Dijk H, de Jaegere PP et al (2001) Postprandial increase of complement component 3 in normolipidemic patients with coronary artery disease: effects of expanded-dose simvastatin. Arterioscler Thromb Vasc Biol 21:1526–1530
Yilmazer M, Fenkci V, Fenkci S, Aktepe O, Sonmezer M, Kurtay G (2003) Association of serum complement (C3, C4) and immunoglobulin (IgG, IgM) levels with hormone replacement therapy in healthy post-menopausal women. Hum Reprod 18:1531–1535
Acknowledgements
This study was supported by grants from the Swedish Heart and Lung Foundation, the Swedish Research Council, and Syskonen Svenssons Foundation.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Engström, G., Hedblad, B., Janzon, L. et al. Weight gain in relation to plasma levels of complement factor 3: results from a population-based cohort study. Diabetologia 48, 2525–2531 (2005). https://doi.org/10.1007/s00125-005-0021-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-005-0021-6