Abstract
Aims/hypothesis
We have recently proposed that fulminant type-1 diabetes is a novel subtype of type-1 diabetes with abrupt onset of insulin-deficient hyperglycaemia without islet-related autoantibodies. The pathogenesis is still unknown, but flu-like symptoms are frequently observed before the onset of disease of this subtype. Enterovirus infection is a candidate environmental factor causing type-1 diabetes. The aim of this study was to determine whether enterovirus infection contributes to the development of fulminant type-1 diabetes.
Methods
We investigated 19 patients with recent-onset fulminant type-1 diabetes, 18 patients with recent-onset typical type-1A diabetes, and 19 healthy controls. IgM, IgG, and IgA subclasses of antibodies to enterovirus were determined by ELISA.
Results
IgA antibody titres to enterovirus were significantly higher in fulminant type-1 diabetes than in typical type-1A diabetes (p=0.033) and controls (p=0.0003). IgM antibodies to enterovirus were not detected in any subject. IgG titres were lower in autoimmune diabetes than fulminant type and controls (p=0.014 and 0.019, respectively).
Conclusions/interpretation
High titres of enterovirus IgA antibodies in serum suggest recurrent enterovirus infection in fulminant type-1 diabetic patients, indicating higher susceptibility to enteroviral infections among them. Such infections might have pathogenetic importance in the triggering of fulminant type-1 diabetes.
Similar content being viewed by others
Introduction
Type 1 (insulin-dependent) diabetes mellitus is characterized by insulin deficiency as a result of the destruction of pancreatic beta cells. It is divided into two subtypes, i.e. autoimmune type-1 (type-1A) diabetes and idiopathic (type-1B) diabetes [1]. Several lines of evidence suggest that pancreatic beta cells are damaged by infiltrating T cells in type-1A diabetes, and several types of autoantibody to pancreatic islet cells have been recognized as markers of type-1A diabetes. These islet-related autoantibodies include islet cell antibodies (ICA), anti-GAD antibodies (GADAb), insulin autoantibodies (IAA), and anti-insulinoma-associated antigen 2 antibodies (IA-2Ab) [1]. Patients with type-1 diabetes who do not have islet autoantibodies at the time of diagnosis are classified as having idiopathic or type-1B diabetes.
A major environmental risk factor disclosed by epidemiological studies is infection by different members of the enterovirus family, mainly coxsackie B viruses in the development of type-1 diabetes [2], but other enteroviruses, for example coxsackie A viruses and several Echoviruses, have also been associated with the development of type-1 diabetes [3]. Case studies have shown that enteroviruses can, indeed, cause acute-onset diabetes [4]. In mouse models of type-1 diabetes encephalomyocarditis (EMC) virus promotes beta cell destruction and insulin-deficient diabetes [5].
We have recently proposed that fulminant type-1 diabetes is a subtype within type-1B diabetes [6–8]. The clinical characteristics of this subtype are quite different from typical type-1A diabetes—remarkably abrupt onset of the disease, negative status of islet-related autoantibodies, virtually no C-peptide secretion (less than 10 μg day−1 in urine), and elevated serum pancreatic enzyme levels [6–8]. Susceptible and resistant class II HLA was also different between fulminant and type-1A diabetes [9]. A nationwide survey of fulminant type-1 diabetes in Japan revealed that this disease is not rare, because more than 20% of ketosis-onset type-1 diabetic patients in Japan have the features of this subtype [7]. The precise aetiology of fulminant type-1 diabetes has not yet been clarified, however.
The involvement of a viral infection has been suggested, because of the markedly acute onset [6–8]. In addition, a nationwide survey also revealed that flu-like symptoms were observed in 71.7% of fulminant type-1 diabetic patients [7], also suggesting that viral infection is critical in the development of fulminant type-1 diabetes.
In this study we investigated enterovirus antibodies in patients with recent-onset type-1 diabetes by using a group-reacting enterovirus-specific ELISA to determine whether enterovirus infection can contribute to the development of fulminant type-1 diabetes. Our assay was shown to react with several different serotypes of enterovirus, for example coxsackie A, coxsackie B, and Echoviruses [10].
Subjects and methods
Patients
We investigated 19 patients with fulminant type-1 diabetes, 18 patients with typical type-1A diabetes, and 19 healthy controls. All the patients developed type-1 diabetes post adolescence. Patients’ sera were obtained in our hospitals. We examined consecutive patients from 1988 to 2002 whose sera were available within 2 months of the onset of overt diabetes. Detailed patient characteristics are shown in Table 1. Inclusion criteria for fulminant type-1 diabetes in this study were:
-
1
ketosis or ketoacidosis at onset of diabetes;
-
2
duration of hyperglycemic symptoms were within a week;
-
3
insulin-dependent both at onset and 6 months after onset;
-
4
the absence of GADAb, ICA, IAA, or IA-2 Ab;
-
5
HbA1c<8.5% on first visit; and
-
6
urinary C-peptide excretion <10 μg day−1.
These criteria were determined on the basis of data for the first 11 patients with fulminant diabetes reported by Imagawa et al. and a nationwide survey in Japan [6–8]. GADAb, IAA and IA-2Ab were measured by radioimmunoassay and ICA were determined by immunohistochemical methods as described previously [6–8]. Patients with typical autoimmune type-1 diabetes were ketosis-prone with GADAb or ICA. The duration of hyperglycemic symptoms before the start of insulin therapy was less than 3 months in these patients. Patients with slowly progressive IDDM or latent-onset diabetes of adult (LADA) were excluded from this study. Age-matched and sex-matched healthy controls were also recruited.
This study was carried out in accordance with the Declaration of Helsinki as revised in 2000, and informed consent was obtained from all subjects.
Enterovirus antibody analyses
Sera of patients and control subjects were collected in our hospitals and kept frozen at −20°C. IgM, IgG, and IgA subclasses of antibodies to enterovirus were determined by ELISA as published previously with some minor modifications. Our system for detecting enterovirus antibodies was shown to react with several different serotypes of enterovirus, for example coxsackie A, coxsackie B, and Echoviruses [10]. Briefly, a local broad-reacting strain of coxsackie B5 virus was used as antigen. ELISA plates were sensitized overnight at room temperature with viral antigen and control antigen in parallel columns. Sera were analysed at a final dilution of 1/440 and were incubated for 2 h at 37°C. Samples subject to IgM and IgA determination were pretreated with sheep-antihuman IgG with the purpose of eliminating the influence of possible rheumatoid factor and competing specific IgG. Appropriate conjugates were incubated for 1 h at 37°C followed by incubation of the substrate. Antibody activity was expressed as arbitrary units (AU), i.e. [(net absorbance of the sample)/(net absorbance of the positive reference)]×100. The method is accredited at the Swedish Board for Accreditation and Conformity Assessment.
Statistical analysis
Statistical analysis was performed using the Mann–Whitney rank sum test. A value of p<0.05 was considered to indicate statistical significance.
Results
IgM antibodies to enterovirus were not detected in any subject.
IgG antibody titres to enterovirus were 90.0 (53.5, 115.3) AU in fulminant type-1 diabetic patients, 54.0 (24.0, 79.0) AU in typical type-1A diabetic patients and 91.0 (56.5, 106.0) AU in healthy controls [median (25 percentile, 75 percentile)]. The titre of IgG antibodies was significantly lower in autoimmune diabetes than in fulminant type-1 diabetes and healthy controls (p=0.014 and p=0.019, respectively).
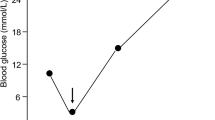
IgA antibody titres to enterovirus were 33.0 (21.3, 87.6) AU in fulminant type-1 diabetic patients, 20.5 (11.0, 35.0) AU in typical type-1A diabetic patients and 10.0 (0, 22.3) AU in healthy controls [median (25 percentile, 75 percentile)]. The titres were significantly higher in fulminant type diabetes than in autoimmune diabetes (p=0.033) and healthy controls (p=0.0003), as shown in Fig. 1.
IgA antibodies to enterovirus in type-1 diabetic patients and healthy controls. The titer of IgA antibodies was significantly higher in fulminant type-1 diabetic patients than in typical type-1 diabetic patients and controls. AU arbitrary units, * p=0.033, ** p=0.0003. The ends of the boxes are the 25th and 75th quartiles, and the line across the middle identifies the median value. The ends of the whiskers are the outermost data points from their respective quartiles that fall within the distance computed as 1.5×(interquartile range)
Discussion
The first 11 patients with fulminant type-1 diabetes were reported in 2000 and 161 patients with this subtype of type-1 diabetes were investigated in a nationwide survey reported in 2003 [6–8]. Patients with fulminant type-1 diabetes fulfil the WHO/ADA criteria of type-1 diabetes but, because of the absence of both islet-related serum autoantibodies and signs of insulitis in pancreas, the pathogenesis of this subtype is largely unknown [6–8]. Viral infection might contribute to the pathogenesis, because of markedly acute destruction of pancreatic beta cells and the presence of pre-existing flu-like symptoms. The pre-existing flu-like symptoms were observed in 71.7% of fulminant type-1 diabetes but in only 26.9% of typical type-1A diabetes [7]. Comparison of enterovirus titres might therefore be of interest. Our present study demonstrated that titres of IgA antibodies to enterovirus were significantly higher in fulminant diabetic patients than in typical autoimmune (type 1A) diabetes and controls.
High titres of IgA antibodies suggest recurrent enterovirus infection in fulminant type-1 diabetic patients. Our system for detecting enterovirus antibodies was shown to react with several different serotypes of enterovirus, for example coxsackie A, coxsackie B, and Echoviruses [10]. Therefore, titres of IgG and IgA antibodies would be increased if different serotypes of enteroviruses repeatedly infected the same patient. Our results therefore suggest that fulminant type-1 diabetic patients are more susceptible to enterovirus infection than autoimmune diabetic patients and controls.
IgM antibodies to enteroviruses were not, on the other hand, detected in any patient or healthy control in this study. This is not unexpected, because all patients and controls were adults. Because primary enterovirus infection usually occurs in childhood, it is expected that IgM antibodies to enteroviruses will rarely be detected in adults even if reinfection has occurred.
In conclusion, high titres of IgA antibodies to enterovirus were found in patients with fulminant type-1 diabetes, indicating that recurrent enterovirus infection precedes this type of diabetes. Our results suggest that fulminant type-1 diabetic patients are especially susceptible to enterovirus infection.
Abbreviations
- AU:
-
arbitrary units
- GADAb:
-
anti-glutamic acid decarboxylase antibodies
- IAA:
-
insulin autoantibodies
- IA-2Ab:
-
anti-insulinoma-associated antigen-2 antibodies
- ICA:
-
islet cell antibodies
References
Alberti KG, Zimmet PZ (1998) Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1: diagnosis and classification of diabetes mellitus provisional report of a WHO consultation. Diabet Med 15:539–553
Graves PM, Norris JM, Pallansch MA, Gerling IC, Rewers M (1997) The role of enteroviral infections in the development of IDDM: limitations of current approaches. Diabetes 46:161–168
Vreugdenhil GR, Schloot NC, Hoorens A et al (2000) Acute onset of type I diabetes mellitus after severe echovirus 9 infection: putative pathogenic pathways. Clin Infect Dis 31:1025–1031
Yoon JW, Austin M, Onodera T, Notkins AL (1979) Virus-induced diabetes mellitus. N Engl J Med 300:1173–1179
Jun HS, Yoon JW (2001) The role of viruses in type I diabetes: two distinct cellular and molecular pathogenic mechanisms of virus-induced diabetes in animals. Diabetologia 44:271–285
Imagawa A, Hanafusa T, Miyagawa J, Matsuzawa Y for the Osaka IDDM Study Group (2000) A novel subtype of type-1 diabetes mellitus characterized by a rapid onset and an absence of diabetes-related antibodies. N Engl J Med 342:301–307
Imagawa A, Hanafusa T, Uchigata Y et al (2003) Fulminant type-1 diabetes—a nationwide survey in Japan. Diabetes Care 26:2345–2352
Shimizu I, Makino H, Osawa H, Kounoue E, Imagawa A, Hanafusa T, Kawasaki E, Fujii Y (2003) Association of fulminant type-1 diabetes with pregnancy. Diabetes Res Clin Pract 62:33–38
Imagawa A, Hanafusa T, Uchigata Y et al. (2003) Different contribution of class II HLA in fulminant and typical autoimmune Type 1 (Type 1A) diabetes. Diabetologia 46(Suppl 2):A108 (Abstract)
Boman J, Nilsson B, Juto P (1992) Serum IgA, IgG, and IgM responses to different enteroviruses as measured by a coxsackie B5-based indirect ELISA. J Med Virol 38:32–35
Acknowledgements
This study was supported by a grants-in-aid from the Japanese Ministry of Health, Labour, and Welfare, the Japan Medical Association and the Japan Diabetes Society. We thank laboratory technicians in the Serology Section of the Department of Clinical Virology for skilful technical assistance.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Imagawa, A., Hanafusa, T., Makino, H. et al. High titres of IgA antibodies to enterovirus in fulminant type-1 diabetes. Diabetologia 48, 290–293 (2005). https://doi.org/10.1007/s00125-004-1624-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-004-1624-z