Abstract
Ischemic stroke is the major contributor to morbidity and mortality in people with diabetes mellitus. In ischemic stroke patients, neuroinflammation is now understood to be one of the main underlying mechanisms for cerebral damage and recovery delay. It has been well-established that toll-like receptor 4 (TLR4) signaling pathway plays a key role in neuroinflammation. Emerging research over the last decade has revealed that, compared to ischemic stroke without diabetes mellitus, ischemic stroke with diabetes mellitus significantly upregulates TLR4-mediated neuroinflammation, increasing the risk of cerebral and neuronal damage as well as neurofunctional recovery delay. This review aims to discuss how ischemic stroke with diabetes mellitus amplifies TLR4-mediated neuroinflammation and its consequences. Additionally covered in this review is the potential application of TLR4 antagonists in the management of diabetic ischemic stroke.

Similar content being viewed by others
Availability of data and material
Not applicable.
References
Feigin VL, Stark BA, Johnson CO, Roth GA, Bisignano C, Abady GG, Abbasifard M, Abbasi-Kangevari M, Abd-Allah F, Abedi V et al (2021) Global, regional, and national burden of stroke and its risk factors, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Neurol 20(10):795–820. https://doi.org/10.1016/s1474-4422(21)00252-0
Musuka TD, Wilton SB, Traboulsi M, Hill MD (2015) Diagnosis and management of acute ischemic stroke: speed is critical. CMAJ 187(12):887–893. https://doi.org/10.1503/cmaj.140355
Simons LA, McCallum J, Friedlander Y, Simons J (1998) Risk factors for ischemic stroke. Stroke 29(7):1341–1346. https://doi.org/10.1161/01.STR.29.7.1341
Banerjee C, Chimowitz MI (2017) Stroke caused by atherosclerosis of the major intracranial arteries. Circ Res 120(3):502–513. https://doi.org/10.1161/circresaha.116.308441
Mosenzon O, Cheng AYY, Rabinstein AA, Sacco S (2023) Diabetes and stroke: what are the connections? J Stroke 25(1):26–38. https://doi.org/10.5853/jos.2022.02306
Kruyt ND, Nys GM, van der Worp HB, van Zandvoort MJ, Kappelle LJ, Biessels GJ (2008) Hyperglycemia and cognitive outcome after ischemic stroke. J Neurol Sci 270(1–2):141–147. https://doi.org/10.1016/j.jns.2008.02.020
Luitse MJ, Biessels GJ, Rutten GE, Kappelle LJ (2012) Diabetes, hyperglycaemia, and acute ischaemic stroke. Lancet Neurol 11(3):261–271. https://doi.org/10.1016/s1474-4422(12)70005-4
Hacke W, Kaste M, Bluhmki E, Brozman M, Dávalos A, Guidetti D, Larrue V, Lees KR, Medeghri Z, Machnig T et al (2008) Thrombolysis with alteplase 3 to 4.5 hours after acute ischemic stroke. N Engl J Med 359(13):1317–1329. https://doi.org/10.1056/NEJMoa0804656
Huang H, Oo TT, Apaijai N, Chattipakorn N, Chattipakorn SC (2023) An updated review of mitochondrial transplantation as a potential therapeutic strategy against cerebral ischemia and cerebral ischemia/reperfusion injury. Mol Neurobiol 60(4):1865–1883. https://doi.org/10.1007/s12035-022-03200-y
Donnan GA, Fisher M, Macleod M, Davis SM (2008) Stroke. The lancet 371(9624):1612–1623. https://doi.org/10.1016/S0140-6736(08)60694-7
Berlis A, Lutsep H, Barnwell S, Norbash A, Wechsler L, Jungreis CA, Woolfenden A, Redekop G, Hartmann M, Schumacher M (2004) Mechanical thrombolysis in acute ischemic stroke with endovascular photoacoustic recanalization. Stroke 35(5):1112–1116. https://doi.org/10.1161/01.STR.0000124126.17508.d3
Ye X, Chopp M, Liu X, Zacharek A, Cui X, Yan T, Roberts C, Chen J (2011) Niaspan reduces high-mobility group box 1/receptor for advanced glycation endproducts after stroke in type-1 diabetic rats. Neuroscience 190:339–345. https://doi.org/10.1016/j.neuroscience.2011.06.004
Ning R, Chopp M, Zacharek A, Yan T, Zhang C, Roberts C, Lu M, Chen J (2014) Neamine induces neuroprotection after acute ischemic stroke in type one diabetic rats. Neuroscience 257:76–85. https://doi.org/10.1016/j.neuroscience.2013.10.071
Venkat P, Yan T, Chopp M, Zacharek A, Ning R, Van Slyke P, Dumont D, Landschoot-Ward J, Liang L, Chen J (2018) Angiopoietin-1 mimetic peptide promotes neuroprotection after stroke in type 1 diabetic rats. Cell Transplant 27(12):1744–1752. https://doi.org/10.1177/0963689718791568
Kigerl KA, de Rivero Vaccari JP, Dietrich WD, Popovich PG, Keane RW (2014) Pattern recognition receptors and central nervous system repair. Exp Neurol 258:5–16. https://doi.org/10.1016/j.expneurol.2014.01.001
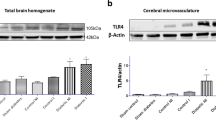
Oo TT, Sumneang N, Ongnok B, Arunsak B, Chunchai T, Kerdphoo S, Apaijai N, Pratchayasakul W, Liang G, Chattipakorn N et al (2022) L6H21 protects against cognitive impairment and brain pathologies via toll-like receptor 4-myeloid differentiation factor 2 signalling in prediabetic rats. Br J Pharmacol 179(6):1220–1236. https://doi.org/10.1111/bph.15741
Huang NQ, Jin H, Zhou SY, Shi JS, Jin F (2017) TLR4 is a link between diabetes and Alzheimer’s disease. Behav Brain Res 316:234–244. https://doi.org/10.1016/j.bbr.2016.08.047
Abdul Y, Abdelsaid M, Li W, Webb RC, Sullivan JC, Dong G, Ergul A (2019) Inhibition of Toll-Like Receptor-4 (TLR-4) Improves neurobehavioral outcomes after acute ischemic stroke in diabetic rats: possible role of vascular endothelial TLR-4. Mol Neurobiol 56(3):1607–1617. https://doi.org/10.1007/s12035-018-1184-8
Li Y, Yao N, Zhang T, Guo F, Niu X, Wu Z, Hou S (2020) Ability of post-treatment glycyrrhizic acid to mitigate cerebral ischemia/reperfusion injury in diabetic mice. Med Sci Monit 26:e926551. https://doi.org/10.12659/MSM.926551
Oo TT, Pratchayasakul W, Chattipakorn N, Chattipakorn SC (2022) Emerging roles of toll-like receptor 4 in chemotherapy-induced neurotoxicity. Neurotoxicology 93:112–127. https://doi.org/10.1016/j.neuro.2022.09.006
Oo TT, Pratchayasakul W, Chattipakorn N, Chattipakorn SC (2020) Potential roles of myeloid differentiation factor 2 on neuroinflammation and its possible interventions. Mol Neurobiol 57(11):4825–4844. https://doi.org/10.1007/s12035-020-02066-2
Lee K-M, Seong S-Y (2009) Partial role of TLR4 as a receptor responding to damage-associated molecular pattern. Immunol Lett 125(1):31–39. https://doi.org/10.1016/j.imlet.2009.05.006
Pandey GN, Rizavi HS, Bhaumik R, Ren X (2019) Innate immunity in the postmortem brain of depressed and suicide subjects: role of toll-like receptors. Brain Behav Immun 75:101–111. https://doi.org/10.1016/j.bbi.2018.09.024
Committee ADAPP (2021) 2. Classification and diagnosis of diabetes: standards of medical care in diabetes—2022. Diabetes Care 45(Supplement_1):S17–S38. https://doi.org/10.2337/dc22-S002
Sinclair A, Saeedi P, Kaundal A, Karuranga S, Malanda B, Williams R (2020) Diabetes and global ageing among 65–99-year-old adults: findings from the International Diabetes Federation Diabetes Atlas, 9(th) edition. Diabetes Res Clin Pract 162:108078. https://doi.org/10.1016/j.diabres.2020.108078
American Diabetes Association (2009) Diagnosis and classification of diabetes mellitus. Diabetes Care 32(Suppl 1):S62–67. https://doi.org/10.2337/dc09-S062
Chen L, Magliano DJ, Zimmet PZ (2011) The worldwide epidemiology of type 2 diabetes mellitus–present and future perspectives. Nat Rev Endocrinol 8(4):228–236. https://doi.org/10.1038/nrendo.2011.183
Patterson CC, Dahlquist GG, Gyürüs E, Green A, Soltész G (2009) Incidence trends for childhood type 1 diabetes in Europe during 1989–2003 and predicted new cases 2005–20: a multicentre prospective registration study. Lancet 373(9680):2027–2033. https://doi.org/10.1016/s0140-6736(09)60568-7
Katsarou A, Gudbjörnsdottir S, Rawshani A, Dabelea D, Bonifacio E, Anderson BJ, Jacobsen LM, Schatz DA, Lernmark Å (2017) Type 1 diabetes mellitus. Nat Rev Dis Primers 3(1):17016. https://doi.org/10.1038/nrdp.2017.16
DeFronzo RA, Ferrannini E, Groop L, Henry RR, Herman WH, Holst JJ, Hu FB, Kahn CR, Raz I, Shulman GI et al (2015) Type 2 diabetes mellitus. Nat Rev Dis Primers 1(1):15019. https://doi.org/10.1038/nrdp.2015.19
Maida CD, Daidone M, Pacinella G, Norrito RL, Pinto A, Tuttolomondo A (2022) Diabetes and Ischemic Stroke: An Old and New Relationship an Overview of the Close Interaction between These Diseases. Int J Mol Sci 23(4):2397. https://doi.org/10.3390/ijms23042397
Sarwar N, Gao P, Seshasai SR, Gobin R, Kaptoge S, Di Angelantonio E, Ingelsson E, Lawlor DA, Selvin E, Stampfer M et al (2010) Diabetes mellitus, fasting blood glucose concentration, and risk of vascular disease: a collaborative meta-analysis of 102 prospective studies. Lancet 375(9733):2215–2222. https://doi.org/10.1016/s0140-6736(10)60484-9
Karapanayiotides T, Piechowski-Jozwiak B, van Melle G, Bogousslavsky J, Devuyst G (2004) Stroke patterns, etiology, and prognosis in patients with diabetes mellitus. Neurology 62(9):1558–1562. https://doi.org/10.1212/01.wnl.0000123252.55688.05
Cui R, Iso H, Yamagishi K, Saito I, Kokubo Y, Inoue M, Tsugane S (2011) Diabetes mellitus and risk of stroke and its subtypes among Japanese: the Japan public health center study. Stroke 42(9):2611–2614. https://doi.org/10.1161/strokeaha.111.614313
Wang L, Wang J, Fang J, Zhou H, Liu X, Su SB (2015) High glucose induces and activates Toll-like receptor 4 in endothelial cells of diabetic retinopathy. Diabetol Metab Syndr 7(1):89. https://doi.org/10.1186/s13098-015-0086-4
Kawamoto EM, Cutler RG, Rothman SM, Mattson MP, Camandola S (2014) TLR4-dependent metabolic changes are associated with cognitive impairment in an animal model of type 1 diabetes. Biochem Biophys Res Commun 443(2):731–737. https://doi.org/10.1016/j.bbrc.2013.12.039
Rohm TV, Meier DT, Olefsky JM, Donath MY (2022) Inflammation in obesity, diabetes, and related disorders. Immunity 55(1):31–55. https://doi.org/10.1016/j.immuni.2021.12.013
Carrillo-Sepulveda MA, Spitler K, Pandey D, Berkowitz DE, Matsumoto T (2015) Inhibition of TLR4 attenuates vascular dysfunction and oxidative stress in diabetic rats. J Mol Med 93(12):1341–1354. https://doi.org/10.1007/s00109-015-1318-7
Forbes JM, Cooper ME (2013) Mechanisms of diabetic complications. Physiol Rev 93(1):137–188. https://doi.org/10.1152/physrev.00045.2011
Feske SK (2021) Ischemic stroke. Am J Med 134(12):1457–1464. https://doi.org/10.1016/j.amjmed.2021.07.027
Lakhan SE, Kirchgessner A, Hofer M (2009) Inflammatory mechanisms in ischemic stroke: therapeutic approaches. J Transl Med 7(1):97. https://doi.org/10.1186/1479-5876-7-97
Ning R, Chopp M, Yan T, Zacharek A, Zhang C, Roberts C, Cui X, Lu M, Chen J (2012) Tissue plasminogen activator treatment of stroke in type-1 diabetes rats. Neuroscience 222:326–332. https://doi.org/10.1016/j.neuroscience.2012.07.018
Kurita N, Yamashiro K, Kuroki T, Tanaka R, Urabe T, Ueno Y, Miyamoto N, Takanashi M, Shimura H, Inaba T et al (2020) Metabolic endotoxemia promotes neuroinflammation after focal cerebral ischemia. J Cereb Blood Flow Metab 40(12):2505–2520. https://doi.org/10.1177/0271678X19899577
Zhang YJ, Guo WJ, Tang ZY, Lin HB, Hong P, Wang JW, Huang XX, Li FX, Xu SY, Zhang HF (2022) Isoflurane attenuates cerebral ischaemia-reperfusion injury via the TLR4-NLRP3 Signalling Pathway in Diabetic Mice. Oxid Med Cell Longev 2022:2650693. https://doi.org/10.1155/2022/2650693
Yang WC, Li TT, Wan Q, Zhang X, Sun LY, Zhang YR, Lai PC, Li WZ (2022) Molecular hydrogen mediates neurorestorative effects after stroke in diabetic rats: the TLR4/NF-kappaB inflammatory pathway. J Neuroimmune Pharmacol. https://doi.org/10.1007/s11481-022-10051-w
Jayaraj RL, Azimullah S, Beiram R, Jalal FY, Rosenberg GA (2019) Neuroinflammation: friend and foe for ischemic stroke. J Neuroinflammation 16(1):142. https://doi.org/10.1186/s12974-019-1516-2
Krishnan A, Lopes RD, Alexander JH, Becker RC, Goldstein LB (2010) Antithrombotic therapy for ischemic stroke: guidelines translated for the clinician. J Thromb Thrombolysis 29(3):368–377. https://doi.org/10.1007/s11239-010-0439-7
Hurford R, Sekhar A, Hughes TAT, Muir KW (2020) Diagnosis and management of acute ischaemic stroke. Pract Neurol 20(4):304–316. https://doi.org/10.1136/practneurol-2020-002557
Eltzschig HK, Eckle T (2011) Ischemia and reperfusion–from mechanism to translation. Nat Med 17(11):1391–1401. https://doi.org/10.1038/nm.2507
Shukla V, Shakya AK, Perez-Pinzon MA, Dave KR (2017) Cerebral ischemic damage in diabetes: an inflammatory perspective. J Neuroinflammation 14(1):21. https://doi.org/10.1186/s12974-016-0774-5
Kim D, Choi I-Y, Jang H, Lee S-H (2013) HMGB1 suppression confers neuroprotection against stroke in diabetic rats. Transl Neurosci 4(4):477–483. https://doi.org/10.2478/s13380-013-0145-y
Kim JM, Lee JE, Cheon SY, Lee JH, Kim SY, Kam EH, Koo BN (2016) The anti-inflammatory effects of agmatine on transient focal cerebral ischemia in diabetic rats. J Neurosurg Anesthesiol 28(3):203–213. https://doi.org/10.1097/ana.0000000000000195
Goldstein RS, Gallowitsch-Puerta M, Yang L, Rosas-Ballina M, Huston JM, Czura CJ, Lee DC, Ward MF, Bruchfeld AN, Wang H et al (2006) Elevated high-mobility group box 1 levels in patients with cerebral and myocardial ischemia. Shock 25(6):571–574. https://doi.org/10.1097/01.shk.0000209540.99176.72
Kim SW, Lee H, Lee HK, Kim ID, Lee JK (2019) Neutrophil extracellular trap induced by HMGB1 exacerbates damages in the ischemic brain. Acta Neuropathol Commun 7(1):94. https://doi.org/10.1186/s40478-019-0747-x
Zhu S, Tang S, Su F (2018) Dioscin inhibits ischemic stroke-induced inflammation through inhibition of the TLR4/MyD88/NF-κB signaling pathway in a rat model. Mol Med Rep 17(1):660–666. https://doi.org/10.3892/mmr.2017.7900
Muriach M, Flores-Bellver M, Romero FJ, Barcia JM (2014) Diabetes and the brain: oxidative stress, inflammation, and autophagy. Oxid Med Cell Longev 2014:102158. https://doi.org/10.1155/2014/102158
Amantea D, Nappi G, Bernardi G, Bagetta G, Corasaniti MT (2009) Post-ischemic brain damage: pathophysiology and role of inflammatory mediators. Febs j 276(1):13–26. https://doi.org/10.1111/j.1742-4658.2008.06766.x
Kriz J (2006) Inflammation in ischemic brain injury: timing is important. Crit Rev Neurobiol 18(1–2):145–157. https://doi.org/10.1615/critrevneurobiol.v18.i1-2.150
Schilling M, Besselmann M, Leonhard C, Mueller M, Ringelstein EB, Kiefer R (2003) Microglial activation precedes and predominates over macrophage infiltration in transient focal cerebral ischemia: a study in green fluorescent protein transgenic bone marrow chimeric mice. Exp Neurol 183(1):25–33. https://doi.org/10.1016/s0014-4886(03)00082-7
Tanaka R, Komine-Kobayashi M, Mochizuki H, Yamada M, Furuya T, Migita M, Shimada T, Mizuno Y, Urabe T (2003) Migration of enhanced green fluorescent protein expressing bone marrow-derived microglia/macrophage into the mouse brain following permanent focal ischemia. Neuroscience 117(3):531–539. https://doi.org/10.1016/s0306-4522(02)00954-5
Price CJ, Menon DK, Peters AM, Ballinger JR, Barber RW, Balan KK, Lynch A, Xuereb JH, Fryer T, Guadagno JV et al (2004) Cerebral neutrophil recruitment, histology, and outcome in acute ischemic stroke: an imaging-based study. Stroke 35(7):1659–1664. https://doi.org/10.1161/01.Str.0000130592.71028.92
Buck BH, Liebeskind DS, Saver JL, Bang OY, Yun SW, Starkman S, Ali LK, Kim D, Villablanca JP, Salamon N et al (2008) Early neutrophilia is associated with volume of ischemic tissue in acute stroke. Stroke 39(2):355–360. https://doi.org/10.1161/strokeaha.107.490128
Yilmaz G, Granger DN (2008) Cell adhesion molecules and ischemic stroke. Neurol Res 30(8):783–793. https://doi.org/10.1179/174313208x341085
Yang Y, Rosenberg GA (2015) Matrix metalloproteinases as therapeutic targets for stroke. Brain Res 1623:30–38. https://doi.org/10.1016/j.brainres.2015.04.024
Li Y, Zhu Z-Y, Huang T-T, Zhou Y-X, Wang X, Yang L-Q, Chen Z-A, Yu W-F, Li P-Y (2018) The peripheral immune response after stroke—a double edge sword for blood-brain barrier integrity. CNS Neurosci Ther 24(12):1115–1128. https://doi.org/10.1111/cns.13081
Lee YB, Park JH, Kim E, Kang CK, Park HM (2014) Arterial stiffness and functional outcome in acute ischemic stroke. J Cerebrovasc Endovasc Neurosurg 16(1):11–19. https://doi.org/10.7461/jcen.2014.16.1.11
Arumugam TV, Okun E, Tang SC, Thundyil J, Taylor SM, Woodruff TM (2009) Toll-like receptors in ischemia-reperfusion injury. Shock 32(1):4–16. https://doi.org/10.1097/SHK.0b013e318193e333
Li M, Liu J, Bi Y, Chen J, Zhao L (2018) Potential medications or compounds acting on toll-like receptors in cerebral ischemia. Curr Neuropharmacol 16(2):160–175. https://doi.org/10.2174/1570159x15666170601125139
Brea D, Blanco M, Ramos-Cabrer P, Moldes O, Arias S, Pérez-Mato M, Leira R, Sobrino T, Castillo J (2011) Toll-like receptors 2 and 4 in ischemic stroke: outcome and therapeutic values. J Cereb Blood Flow Metab 31(6):1424–1431. https://doi.org/10.1038/jcbfm.2010.231
Kilic U, Kilic E, Matter CM, Bassetti CL, Hermann DM (2008) TLR-4 deficiency protects against focal cerebral ischemia and axotomy-induced neurodegeneration. Neurobiol Dis 31(1):33–40. https://doi.org/10.1016/j.nbd.2008.03.002
Hua F, Tang H, Wang J, Prunty MC, Hua X, Sayeed I, Stein DG (2015) TAK-242, an antagonist for Toll-like receptor 4, protects against acute cerebral ischemia/reperfusion injury in mice. J Cereb Blood Flow Metab 35(4):536–542. https://doi.org/10.1038/jcbfm.2014.240
Parada E, Casas AI, Palomino-Antolin A, Gómez-Rangel V, Rubio-Navarro A, Farré-Alins V, Narros-Fernandez P, Guerrero-Hue M, Moreno JA, Rosa JM et al (2019) Early toll-like receptor 4 blockade reduces ROS and inflammation triggered by microglial pro-inflammatory phenotype in rodent and human brain ischaemia models. Br J Pharmacol 176(15):2764–2779. https://doi.org/10.1111/bph.14703
Li C, Che LH, Ji TF, Shi L, Yu JL (2017) Effects of the TLR4 signaling pathway on apoptosis of neuronal cells in diabetes mellitus complicated with cerebral infarction in a rat model. Sci Rep 7:43834. https://doi.org/10.1038/srep43834
Author information
Authors and Affiliations
Contributions
Thura Tun Oo conceptualizes, writes, edits, and finalizes the whole manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Competing interests
The author declares no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Oo, T.T. Ischemic stroke and diabetes: a TLR4-mediated neuroinflammatory perspective. J Mol Med (2024). https://doi.org/10.1007/s00109-024-02441-9
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00109-024-02441-9