Abstract
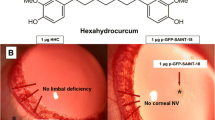
Corneal neovascularization is a leading cause for compromised vision. Therapeutic prevention of corneal neovascularization is a major clinical challenge, and there is a compelling need to seek effective and safe therapy for this pathology. This study is aimed to evaluate curcumin nanoparticle for prevention of corneal neovascularization. MePEG-PCL nanoparticles were successfully prepared and characterized. The nanoparticle of curcumin has shown increased efficiency in preventing angiogenic sprouting in vitro. Topical delivery of curcumin nanoparticle in the eye showed enhanced retention of curcumin in the cornea, and significant improvement in prevention of corneal neovascularization over free curcumin as graded clinically and by histopathology; suppression in the expression of VEGF, inflammatory cytokines, and MMP was evidenced in the treated cornea. Curcumin inhibited NFκB in LPS-induced corneal cells. Histopathology and scanning electron microscopy showed absence of any adverse change in the corneal structure following application of curcumin nanoparticle. Therefore, we conclude that curcumin nanoparticle can be a potential candidate for prevention of corneal neovascularization.
Key message
-
Curcumin nanoparticles show enhanced retention of curcumin in the cornea.
-
Curcumin NPs suppress the expression of VEGF, inflammatory cytokines, and MMP.
-
Curcumin NPs prevent corneal neovascularization by suppressing the NFκB pathway.
-
Curcumin NPs may be a promising candidate for prevention of corneal neovascularization.








Similar content being viewed by others
References
Ambati BK, Nozaki M, Singh N, Takeda A, Jani PD, Suthar T, Albuquerque RJ, Richter E, Sakurai E, Newcomb MT et al (2006) Corneal avascularity is due to soluble VEGF receptor-1. Nature 443:993–997
Cursiefen C, Chen L, Saint-Geniez M, Hamrah P, Jin Y, Rashid S, Pytowski B, Persaud K, Wu Y, Streilein JW et al (2006) Proc Natl Acad Sci U S A 103:11405–11410
Amano S, Rohan R, Kuroki M, Tolentino M, Adamis AP (1998) Requirement for vascular endothelial growth factor in wound- and inflammation-related corneal neovascularization. Invest Ophthalmol Vis Sci 39:18–22
Cursiefen C, Chen L, Borges LP, Jackson D, Cao J, Radziejewski C, D’Amore PA, Dana MR, Wiegand SJ, Streilein JW (2004) VEGF-A stimulates lymphangiogenesis and hemangiogenesis in inflammatory neovascularization via macrophage recruitment. J Clin Invest 113:1040–1050
Gong Y, Koh DR (2010) Neutrophils promote inflammatory angiogenesis via release of preformed VEGF in an in vivo corneal model. Cell Tissue Res 339:437–448
Philipp W, Speicher L, Humpel C (2000) Expression of vascular endothelial growth factor and its receptors in inflamed and vascularized human corneas. Invest Ophthalmol Vis Sci 41:2514–2522
Gan L, Fagerholm P, Palmblad J (2004) Vascular endothelial growth factor (VEGF) and its receptor VEGFR-2 in the regulation of corneal neovascularization and wound healing. Acta Ophthalmol Scand 82:557–563
Benelli U, Ross JR, Nardi M, Klintworth GK (1997) Corneal neovascularization induced by xenografts or chemical cautery: inhibition by cyclosporin A. Invest Ophthalmol Vis Sci 38:274–282
Hayashi A, Popovich KS, Kim HC, de Juan E (1997) Role of protein tyrosine phosphorylation in rat corneal neovascularization. Graefes Arch Clin Exp Ophthalmol 235:460–467
Lee P, Wang CC, Adamis AP (1998) Ocular neovascularization: an epidemiologic review. Surv Ophthalmol 43:245–269
Gonzalez L, Loza RJ, Han KY, Sunoqrot S, Cunningham C, Purta P, Drake J, Jain S, Hong S, Chang JH (2013) Nanotechnology in corneal neovascularization therapy—a review. J Ocul Pharmacol Ther 29:124–134
Sarchahi AA, Maimandi A, Tafti AK, Amani M (2008) Effects of acetylcysteine and dexamethasone on experimental corneal wounds in rabbits. Ophthalmic Res 40:41–48
Guidera AC, Luchs JI, Udell IJ (2001) Keratitis, ulceration, and perforation associated with topical nonsteroidal anti-inflammatory drugs. Ophthalmology 108:936–944
Shakiba Y, Mansouri K, Rezaei N, Arshadi D (2009) Corneal neovascularization: molecular events and therapeutic options. Recent Patents Inflamm Allergy Drug Discov 3:221–231
Koenig Y, Bock F, Kruse FE, Stock K, Cursiefen C (2012) Angioregressive pretreatment of mature corneal blood vessels before keratoplasty: fine-needle vessel coagulation combined with anti-VEGFs. Cornea 31:887–892
Kim SW, Ha BJ, Kim EK, Tchah H, Kim TI (2008) The effect of topical bevacizumab on corneal neovascularization. Ophthalmology 115:33–38
Oh JY, Kim MK, Wee WR (2009) Subconjunctival and intracorneal bevacizumab injection for corneal neovascularization in lipid keratopathy. Cornea 28:1070–1073
Ambati BK, Anand A, Joussen AM, Kuziel WA, Adamis AP, Ambati J (2003) Sustained inhibition of corneal neovascularization by genetic ablation of CCR5. Invest Ophthalmol Vis Sci 44:590–593
Ambati BK, Joussen AM, Anand A, Adamis AP, Ambati J (2003) Inhibition of corneal neovascularization by genetic ablation of CCR2. Cornea 22:465–467
Lu P, Li L, Liu G, van Rooijen N, Mukaida N, Zhang X (2009) Opposite roles of CCR2 and CX3CR1 macrophages in alkali-induced corneal neovascularization. Cornea 28:562–569
Lan W, Petznick A, Heryati S, Rifada M, Tong L (2012) Nuclear factor-kB: central regulator in ocular surface inflammation and diseases. Ocul Surf 10:137–148
Zhao F, Gong Y, Hu Y, Lu M, Wang J, Dong J, Chen D, Chen L, Fu F, Qiu F (2015) Curcumin and its major metabolites inhibit the inflammatory response induced by lipopolysaccharide: translocation of nuclear factor-κB as potential target. Mol Med Rep 11:3087–3093
Gaudana R, Jwala J, Boddu SH (2009) Recent perspectives in ocular drug delivery. Pharm Res 26:1197–1216
Chang JH, Gabison EE, Kato T (2001) Corneal neovascularization. Curr Opin Ophthalmol 12:242–249
Rawas-Qalaji M, Williams CA (2012) Advances in ocular drug delivery. Curr Eye Res 37:345–356
Guha R, Chowdhury S, Palui H, Mishra A, Basak S, Mandal TK, Hazra S, Konar A (2013) Doxorubicin-loaded MePEG-PCL nanoparticles for prevention of posterior capsular opacification. Nanomedicine (Lond) 8:1415–1428
Qazi Y, Stagg B, Singh N, Singh S, Zhang X, Luo L, Simonis J, Kompella UB, Ambati BK (2012) Nanoparticle-mediated delivery of shRNA. VEGF-A plasmids regresses corneal neovascularization. Invest Ophthalmol Vis Sci 53:2837–2844
Al-Abd AM, Kim NH, Song SC, Lee SJ, Kuh HJ (2009) A simple HPLC method for doxorubicin in plasma and tissues of nude mice. Arch Pharm Res 32:605–611
Bian F, Zhang MC, Zhu Y (2008) Inhibitory effect of curcumin on corneal neovascularization in vitro and in vivo. Ophthalmologica 222:178–186
Klein R, Lobes LA Jr (1976) Ocular alkali burns in a large urban area. Ann Ophthalmol 8:1185–1189
Morgan SJ (1987) Chemical burns of the eye: causes and management. Br J Ophthalmol 71:854
Huang FC, Chan WK, Moriarty KJ (1998) Novel cytokine release inhibitors. Part I: triterpenes. Bioorg Med Chem Lett 8:1883–1886
Kim JS, Choi JS, Chung SK (2010) The effect of curcumin on corneal neovascularization in rabbit eyes. Curr Eye Res 35:274–280
Sivak JM, Ostriker AC, Woolfenden A, Demirs J, Cepeda R, Long D, Anderson K, Jaffee B (2011) Pharmacologic uncoupling of angiogenesis and inflammation during initiation of pathological corneal neovascularization. J Biol Chem 286:44965–44975
Ma DH, Chen JK, Kim WS, Hao YX, Wu HC, Tsai RJ, Hwang DG, Zhang F (2001) Expression of matrix metalloproteinases 2 and 9 and tissue inhibitors of metalloproteinase 1 and 2 in inflammation-induced corneal neovascularisation. Ophthalmic Res 33:353–362
Arbiser JL, Klauber N, Rohan R, van Leeuwen R, Huang MT, Fisher C, Flynn E, Byers HR (1998) Curcumin is an in vivo inhibitor of angiogenesis. Mol Med 4:376–383
Gao C, Ding Z, Liang B, Chen N, Cheng D (2003) Study on the effects of curcumin on angiogenesis. Zhong Yao Cai 26:499–502
Gupta SK, Kumar B, Nag TC (2011) Curcumin prevents experimental diabetic retinopathy in rats through its hypoglycemic, antioxidant, and anti-inflammatory mechanisms. J Ocul Pharmacol Ther 27:123–130
Anand P, Kunnumakkara AB, New-man RA, Aggarwal BB (2007) Bioavailability of curcumin: problems and promises. Mol Pharm 4:807–818
Acknowledgments
We acknowledge the Department of Biotechnology (Grant No. BT/PR13434/NNT/28/469/2009), Government of India, for funding and West Bengal University of Animal & Fishery Sciences and CSIR-IICB for the support.
Conflict of interest
The authors declare no conflict of interests related to this study.
Author information
Authors and Affiliations
Corresponding authors
Additional information
Nirparaj Pradhan and Rajdeep Guha contributed equally to this work.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Suppl. Fig. 1
(PDF 67 kb)
Rights and permissions
About this article
Cite this article
Pradhan, N., Guha, R., Chowdhury, S. et al. Curcumin nanoparticles inhibit corneal neovascularization. J Mol Med 93, 1095–1106 (2015). https://doi.org/10.1007/s00109-015-1277-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00109-015-1277-z