Abstract
Background
Intense noxious input from the periphery may result in central sensitization and hyperexcitability, thus accentuating subsequent postoperative pain. Parturients who undergo emergency cesarean section (C-sec) after experiencing labor pain often develop labor pain-induced sensitization.
Objective
This retrospective study evaluated whether parturients without epidural labor analgesia (ELA) who underwent emergency C‑sec, experienced more severe postoperative pain and required more rescue analgesics during the postoperative period.
Methods
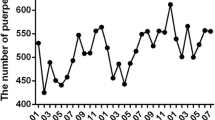
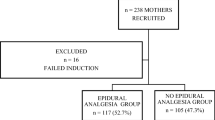
The institution’s medical database was searched for parturients who underwent emergency C‑sec under spinal anesthesia for any reason between January 2013 and December 2016. Those who underwent elective C‑sec under spinal anesthesia were included as the reference arm. Parturients were divided into three groups: ELA, no-ELA and elective. Characteristics of patients and perioperative outcomes were evaluated. As primary outcomes, numerical rating scale (NRS) for postoperative pain (0–10) was recorded up to 96 h postoperatively, and use of rescue analgesics was evaluated at 6, 24, and 48 h postoperatively.
Results
In the ELA, no-ELA, and elective groups, 61, 73, and 88 parturients, respectively, were ultimately enrolled. The NRS for pain were similar among the three groups, except at 6 h postoperatively. Parturients in the no-ELA group demonstrated significantly higher NRS at 6 h postoperatively than those in the ELA group (P = 0.01).More patients in the no-ELA group required rescue analgesics than in the ELA (P = 0.001) and elective groups (P < 0.001) at 6–24 h postoperatively. Moreover, the proportion of patients requiring rescue analgesics ≥2 times was also significantly higher in the no-ELA group (vs. the ELA group, P = 0.004; vs. the elective group, P < 0.001).
Conclusion
Parturients undergoing emergency C‑sec without ELA management during labor experienced greater postoperative pain and a greater use of rescue analgesics during the postoperative period. The findings suggest that administration of ELA before emergency C‑sec may act as pre-emptive analgesia against postoperative pain.
Zusammenfassung
Hintergrund
Intensive periphere Schmerzstimuli können zu einer zentralen Sensibilisierung und Übererregbarkeit führen, wodurch sich die späteren postoperativen Schmerzen verstärken können. Gebärende, die sich unter Wehenschmerzen einem Notfall-Kaiserschnitt unterziehen, entwickeln häufig eine wehenschmerzbedingte Sensibilisierung.
Ziele
In dieser retrospektiven Studie wurde untersucht, ob bei Gebärenden ohne Epiduralanästhesie (EDA), bei denen ein Notfall-Kaiserschnitt durchgeführt wurde, stärkere postoperative Schmerzen auftraten und im postoperativen Zeitraum mehr Zusatzanalgetika erforderlich waren.
Methoden
Die medizinische Datenbank der Einrichtung wurde nach Gebärenden durchsucht, bei denen zwischen Januar 2013 und Dezember 2016 aus irgendeinem Grund ein Notfall-Kaiserschnitt unter Spinalanästhesie durchgeführt wurde. Diejenigen, die einen elektiven Kaiserschnitt unter Spinalanästhesie erhielten, wurden als Vergleichsgruppe gescreent. Die Gebärenden wurden in 3 Gruppen unterteilt: EDA-, Nicht-EDA- und elektive Gruppe. Es wurden Daten zu den Patientencharakteristika sowie zum perioperativen und postoperativen Verlauf erfasst. Als primäre Ergebnisse wurde die numerische Rating-Skala (NRS) für postoperative Schmerzen (0–10) bis 96 h postoperativ aufgezeichnet und die Anwendung von Zusatzanalgetika wurde 6, 24 und 48 h postoperativ bewertet.
Ergebnisse
Bei der EDA-, Nicht-EDA- und elektiven Gruppe wurden letztendlich 61, 73 bzw. 88 Gebärende eingeschlossen. Die NRS-Scores für postoperative Schmerzen waren in den 3 Gruppen ähnlich, mit Ausnahme von 6 h postoperativ. Die Gebärenden in der Nicht-EDA-Gruppe zeigten 6 h postoperativ eine signifikant höhere NRS-Werte als diejenigen in der EDA-Gruppe (p = 0,01). Allerdings benötigten 6–24 h nach der Operation mehr Patienten in der Nicht-EDA-Gruppe Zusatzanalgetika als in der EDA-Gruppe (p = 0,001) und der elektiven Gruppe (p < 0,001). Darüber hinaus war der Anteil der Patienten, die mehr als 2‑mal so viele Zusatzanalgetika benötigten, in der Nicht-EDA-Gruppe signifikant höher als in den beiden anderen Gruppen (gegenüber der EDA-Gruppe, p = 0,004; gegenüber der elektiven Gruppe, p < 0,001).
Schlussfolgerung
Bei Gebärenden, die in der Wehenperiode einen Notfall-Kaiserschnitt ohne EDA erhielten, traten stärkere postoperative Schmerzen auf, denen während der postoperativen Zeit ein verstärkter Einsatz von Zusatzanalgetika folgte. Die Ergebnisse legen nahe, dass die Verabreichung von EDA vor einem Notfall-Kaiserschnitt als präventive Analgesie gegen postoperative Schmerzen wirken kann.


Similar content being viewed by others
References
Jones L, Othman M, Dowswell T et al (2012) Pain management for women in labour: an overview of systematic reviews. Cochrane Database Syst Rev 3:CD9234
Declercq ER, Sakala C, Corry MP, Applebaum S (2007) Listening to Mothers II: Report of the Second National U.S. Survey of Women’s Childbearing Experiences: Conducted January-February 2006 for Childbirth Connection by Harris Interactive(R) in partnership with Lamaze International. J Perinat Educ 16:9–14
Declercq ER, Sakala C, Corry MP, Applebaum S (2007) Listening to Mothers II: Report of the Second National U.S. Survey of Women’s Childbearing Experiences: Conducted January-February 2006 for Childbirth Connection by Harris Interactive(R) in partnership with Lamaze International. J Perinat Educ 16:15–17
Ueland K, Hansen JM (1969) Maternal cardiovascular dynamics. 3. Labor and delivery under local and caudal analgesia. Am J Obstet Gynecol 103:8–18
Anim-Somuah M, Smyth RM, Cyna AM, Cuthbert A (2018) Epidural versus non-epidural or no analgesia for pain management in labour. Cochrane Database Syst Rev 5:CD331
Lieberman E, O’Donoghue C (2002) Unintended effects of epidural analgesia during labor: a systematic review. Am J Obstet Gynecol 186:S31–68
Cervero F (1995) Visceral pain: mechanisms of peripheral and central sensitization. Ann Med 27:235–239
Kissin I (2000) Preemptive analgesia. Anesthesiology 93:1138–1143
Katz J, Clarke H, Seltzer Z (2011) Review article: Preventive analgesia: quo vadimus? Anesth Analg 113:1242–1253
Ong CK, Lirk P, Seymour RA, Jenkins BJ (2005) The efficacy of preemptive analgesia for acute postoperative pain management: a meta-analysis. Anesth Analg 100:757–773
Ip HY, Abrishami A, Peng PW, Wong J, Chung F (2009) Predictors of postoperative pain and analgesic consumption: a qualitative systematic review. Anesthesiology 111:657–677
Caumo W, Schmidt AP, Schneider CN et al (2002) Preoperative predictors of moderate to intense acute postoperative pain in patients undergoing abdominal surgery. Acta Anaesthesiol Scand 46:1265–1271
Borly L, Anderson IB, Bardram L et al (1999) Preoperative prediction model of outcome after cholecystectomy for symptomatic gallstones. Scand J Gastroenterol 34:1144–1152
Kalkman CJ, Visser K, Moen J, Bonsel GJ, Grobbee DE, Moons KG (2003) Preoperative prediction of severe postoperative pain. Pain 105:415–423
Latremoliere A, Woolf CJ (2009) Central sensitization: a generator of pain hypersensitivity by central neural plasticity. J Pain 10:895–926
Thomas T, Robinson C, Champion D, McKell M, Pell M (1998) Prediction and assessment of the severity of post-operative pain and of satisfaction with management. Pain 75:177–185
Committee on Practice Bulletins—Obstetrics (2017) Practice Bulletin No. 177: Obstetric Analgesia and Anesthesia. Obstet Gynecol 129:e73–e89
Vincent RD Jr., Chestnut DH (1998) Epidural analgesia during labor. Am Fam Physician 58:1785–1792
Vermelis JM, Wassen MM, Fiddelers AA, Nijhuis JG, Marcus MA (2010) Prevalence and predictors of chronic pain after labor and delivery. Curr Opin Anaesthesiol 23:295–299
Eisenach JC, Pan PH, Smiley R, Lavand’homme P, Landau R, Houle TT (2008) Severity of acute pain after childbirth, but not type of delivery, predicts persistent pain and postpartum depression. Pain 140:87–94
Kainu JP, Sarvela J, Tiippana E, Halmesmaki E, Korttila KT (2010) Persistent pain after caesarean section and vaginal birth: a cohort study. Int J Obstet Anesth 19:4–9
Kain ZN, Sevarino F, Alexander GM, Pincus S, Mayes LC (2000) Preoperative anxiety and postoperative pain in women undergoing hysterectomy. A repeated-measures design. J Psychosom Res 49:417–422
Sjoling M, Nordahl G, Olofsson N, Asplund K (2003) The impact of preoperative information on state anxiety, postoperative pain and satisfaction with pain management. Patient Educ Couns 51:169–176
Bansal T, Joon A (2017) A comparative study to assess preoperative anxiety in obstetric patients undergoing elective or emergency cesarean section. Anesth Pain Intensive Care 21:25–30
Tzeng YL, Yang YL, Kuo PC, Lin YC, Chen SL (2017) Pain, anxiety, and fatigue during labor: a prospective, repeated measures study. J Nurs Res 25:59–67
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
H.-Y. Park, Y.-W. Park, J.-W. Hwang, S.-H. Do and H.-S. Na declare that they have no competing interests. This research did not receive any specific grant from funding agencies in the public, commercial, or no-for-profit sectors.
All procedures performed in studies involving human participants or on human tissue were in accordance with the ethical standards of the institutional and/or national research committee (Institutional Review Board of Seoul National University Bundang Hospital (B-1709/418-105)) and with the 1975 Helsinki declaration and its later amendments or comparable ethical standards. The requirement for informed consent was waived.
Rights and permissions
About this article
Cite this article
Park, HY., Park, YW., Hwang, JW. et al. The influence of preoperative epidural labor analgesia on postoperative pain in parturients undergoing emergency cesarean section. Anaesthesist 69, 352–358 (2020). https://doi.org/10.1007/s00101-020-00753-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00101-020-00753-2