Abstract
Background
Gas exchange disturbance may develop during urologic robotic laparoscopic surgery with the patient in a steep Trendelenburg position. This study investigated whether prolonged inspiratory time could mitigate gas exchange disturbances including hypercapnia.
Methods
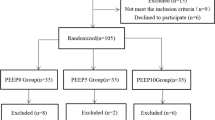
In this randomized cross-over trial, 32 patients scheduled for robot-assisted urologic surgery were randomized to receive an inspiratory to expiratory time ratio (I:E) of 1:1 for the first hour of pneumoperitoneum followed by 1:2 for last period of surgery (group A, n = 17) or I:E of 1:2 followed by 1:1 (group B, n = 15). Arterial blood gas analysis, airway pressure and hemodynamic variables were assessed at four time points (T1: 10 min after induction of general anesthesia, T2: 1 h after the initiation of pneumoperitoneum, T3: 1 h after T2 and T4: at skin closure). The carry over effect of initial I:E was also evaluated over the next hour through arterial blood gas analysis.
Results
There was a significant decrease in partial pressure of oxygen in arterial blood (PaO2) for both groups at T2 and T3 compared to T1 but in group B the PaO2 at T4 was not decreased from the baseline. Partial pressure of carbon dioxide in arterial blood (PaCO2) increased with I:E of 1:2 but did not significantly increase with I:E of 1:1; however, there were no differences in PaO2 and PaCO2 between the groups.
Conclusion
Decreased oxygenation by pneumoperitoneum was improved and PaCO2 did not increase after 1 h of I:E of 1:1; however, the effect of equal ratio ventilation longer than 1 h remains to be determined. There was no carryover effect of the two different I:E ratios.
Zusammenfassung
Hintergrund
Gasaustauschstörungen können bei der urologischen robotergestützten Laparoskopie unter steiler Trendelenburg-Position auftreten. Wir untersuchten, ob eine verlängerte Einatmungszeit Gasaustauschstörungen einschließlich Hyperkapnie mildern könnte.
Methoden
In dieser randomisierten „Cross-over“-Studie wurden 32 Patienten, die für die robotergestützte urologische Chirurgie vorgesehen waren, randomisiert, um ein inspiratorisches zu exspiratorisches Zeitverhältnis (I:E) von 1:1 für die erste Stunde Pneumoperitoneum gefolgt von 1:2 für das letzte Mal der Operation (Gruppe A, n = 17) oder I:E von 1:2, gefolgt von 1:1 (Gruppe B, n = 15), zu erhalten. Arterielle Blutgasanalyse, Atemwegsdruck und hämodynamische Variablen wurden zu 4 Zeitpunkten beurteilt (T1: 10 min nach Induktion der Vollnarkose; T2: 1 h nach Einleitung des Pneumoperitoneums; T3: 1 h nach T2; T4: bei Hautverschluss). Wir evaluierten auch den Verschleppungseffekt des initialen I:E über die nächste Stunde durch arterielle Blutgasanalyse.
Ergebnisse
Es gab eine signifikante Abnahme des Sauerstoffpartialdrucks im arteriellen Blut (paO2) für beide Gruppen bei T2 und T3 im Vergleich zu T1, aber in Gruppe B war der paO2 bei T4 nicht geringer als die Basislinie. Der Kohlendioxidpartialdruck im arteriellen Blut (paCO2) stieg mit I:E von 1:2, aber nicht signifikant mit I:E von 1:1. Allerdings gab es keinen Unterschied in paO2 und PaCO2 zwischen den Gruppen.
Schlussfolgerungen
Die verminderte Sauerstoffversorgung durch das Pneumoperitoneum wurde verbessert, und der paCO2-Wert stieg nach 1h I:E von 1:1 nicht an. Der Effekt einer gleichmäßigen Beatmung, die länger als 1h dauert, muss jedoch noch bestimmt werden. Es gab keinen Übertragungseffekt von 2 verschiedenen I:E-Verhältnissen.


Similar content being viewed by others
References
Lowrance WT, Eastham JA, Savage C et al (2012) Contemporary open and robotic radical prostatectomy practice patterns among urologists in the United States. J Urol 187:2087–2092
Cho A, Lee JE, Kwon GY et al (2011) Post-operative acute kidney injury in patients with renal cell carcinoma is a potent risk factor for new-onset chronic kidney disease after radical nephrectomy. Nephrol Dial Transplant 26:3496–3501
Gainsburg DM (2012) Anesthetic concerns for robotic-assisted laparoscopic radical prostatectomy. Minerva Anestesiol 78:596–604
Lian M, Zhao X, Wang H et al (2016) Respiratory dynamics and dead space to tidal volume ratio of volume-controlled versus pressure-controlled ventilation during prolonged gynecological laparoscopic surgery. Surg Endosc 31:3605–3613
Assad OM, El Sayed AA, Khalil MA (2016) Comparison of volume-controlled ventilation and pressure-controlled ventilation volume guaranteed during laparoscopic surgery in Trendelenburg position. J Clin Anesth 34:55–61
Choi EM, Na S, Choi SH et al (2011) Comparison of volume-controlled and pressure-controlled ventilation in steep Trendelenburg position for robot-assisted laparoscopic radical prostatectomy. J Clin Anesth 23:183–188
Shen JC, Ji MH, Yang C et al (2011) Severe carbon dioxide embolism during laparoscopic kidney resection. Acta Anaesthesiol Scand 55:505
Nguyen NT, Wolfe BM (2005) The physiologic effects of pneumoperitoneum in the morbidly obese. Ann Surg 241:219–226
Tharratt RS, Allen RP, Albertson TE (1988) Pressure controlled inverse ratio ventilation in severe adult respiratory failure. Chest 94:755–762
Chan K, Abraham E (1992) Effects of inverse ratio ventilation on cardiorespiratory parameters in severe respiratory failure. Chest 102:1556–1561
Zavala E, Ferrer M, Polese G et al (1998) Effect of inverse I:E ratio ventilation on pulmonary gas exchange in acute respiratory distress syndrome. Anesthesiology 88:35–42
Abraham E, Yoshihara G (1989) Cardiorespiratory effects of pressure controlled inverse ratio ventilation in severe respiratory failure. Chest 96:1356–1359
Kotani T, Katayama S, Fukuda S et al (2016) Pressure-controlled inverse ratio ventilation as a rescue therapy for severe acute respiratory distress syndrome. Springerplus 5:716
Mercat A, Graini L, Teboul JL et al (1993) Cardiorespiratory effects of pressure-controlled ventilation with and without inverse ratio in the adult respiratory distress syndrome. Chest 104:871–875
Mercat A, Diehl JL, Michard F et al (2001) Extending inspiratory time in acute respiratory distress syndrome. Crit Care Med 29:40–44
Clarke JP, Shuitemaker MN, Sleigh JW (1998) The effect of intraoperative ventilation strategies on perioperative atelectasis. Anaesth Intensive Care 26:262–266
Kim WH, Hahm TS, Kim JA et al (2013) Prolonged inspiratory time produces better gas exchange in patients undergoing laparoscopic surgery: a randomised trial. Acta Anaesthesiol Scand 57:613–622
Lee SM, Kim WH, Ahn HJ et al (2013) The effects of prolonged inspiratory time during one-lung ventilation: a randomised controlled trial. Anaesthesia 68:908–916
Zhang WP, Zhu SM (2016) The effects of inverse ratio ventilation on cardiopulmonary function and inflammatory cytokine of bronchoaveolar lavage in obese patients undergoing gynecological laparoscopy. Acta Anaesthesiol Taiwan 54:1–5
Butterworth J, Mackey D, Wasnick J (2013) Morgan and Mikhail’s clinical anesthesiology. McGraw-Hill, New York
Freeman PR (1989) The performance of the two-stage analysis of two-treatment, two-period crossover trials. Stat Med 8:1421–1432
Marcy TW, Marini JJ (1991) Inverse ratio ventilation in ARDS. Rationale and implementation. Chest 100:494–504
Huang CC, Shih MJ, Tsai YH et al (2001) Effects of inverse ratio ventilation versus positive end-expiratory pressure on gas exchange and gastric intramucosal PCO(2) and pH under constant mean airway pressure in acute respiratory distress syndrome. Anesthesiology 95:1182–1188
Spoerel WE (1980) Low frequency ventilation. Anaesthesia 35:1087–1093
Jo YY, Kim JY, Park CK et al (2016) The effect of ventilation strategy on arterial and cerebral oxygenation during laparoscopic bariatric surgery. Obes Surg 26:339–344
Xu L, Shen J, Yan M (2017) The effect of pressure-controlled inverse ratio ventilation on lung protection in obese patients undergoing gynecological laparoscopic surgery. J Anesth 31:651–656
Jo YY, Kim JY, Chang YJ et al (2016) The effect of equal ratio ventilation on oxygenation, respiratory mechanics, and cerebral perfusion pressure during laparoscopy in the Trendelenburg position. Surg Laparosc Endosc Percutan Tech 26:221–225
Park JH, Lee JS, Lee JH et al (2016) Effect of the prolonged inspiratory to expiratory ratio on oxygenation and respiratory mechanics during surgical procedures. Medicine (Baltimore) 95:e3269
Boros SJ, Matalon SV, Ewald R et al (1977) The effect of independent variations in inspiratory-expiratory ratio and end expiratory pressure during mechanical ventilation in hyaline membrane disease: the significance of mean airway pressure. J Pediatr 91:794–798
Pesenti A, Marcolin R, Prato P et al (1985) Mean airway pressure vs. positive end-expiratory pressure during mechanical ventilation. Crit Care Med 13:34–37
Berman LS, Downs JB, Van Eeden A et al (1981) Inspiration: expiration ratio. Is mean airway pressure the difference? Crit Care Med 9:775–777
Pepe PE, Marini JJ (1982) Occult positive end-expiratory pressure in mechanically ventilated patients with airflow obstruction: the auto-PEEP effect. Am Rev Respir Dis 126:166–170
Jardins TD (2013) Cardiopulmonary anatomy & physiology: essentials of respiratory care. CENGAGE, Boston, p 118
Hess DR (2014) Respiratory mechanics in mechanically ventilated patients. Respir Care 59:1773–1794
Tyagi A, Kumar R, Sethi AK et al (2011) A comparison of pressure-controlled and volume-controlled ventilation for laparoscopic cholecystectomy. Anaesthesia 66:503–508
Ogurlu M, Kucuk M, Bilgin F et al (2010) Pressure-controlled vs volume-controlled ventilation during laparoscopic gynecologic surgery. J Minim Invasive Gynecol 17:295–300
De Baerdemaeker LE, Van Der Herten C, Gillardin JM et al (2008) Comparison of volume-controlled and pressure-controlled ventilation during laparoscopic gastric banding in morbidly obese patients. Obes Surg 18:680–685
Ferrando C, Belda FJ (2015) Inverse ratio ventilation: back to the future? Crit Care Med 43:724–725
Blank RS, Colquhoun DA, Durieux ME et al (2016) Management of one-lung ventilation: impact of tidal volume on complications after thoracic surgery. Anesthesiology 124:1286–1295
Almarakbi WA, Fawzi HM, Alhashemi JA (2009) Effects of four intraoperative ventilatory strategies on respiratory compliance and gas exchange during laparoscopic gastric banding in obese patients. Br J Anaesth 102:862–868
Loring SH, Behazin N, Novero A et al (2014) Respiratory mechanical effects of surgical pneumoperitoneum in humans. J Appl Physiol 117:1074–1079
Reinius H, Jonsson L, Gustafsson S et al (2009) Prevention of atelectasis in morbidly obese patients during general anesthesia and paralysis: a computerized tomography study. Anesthesiology 111:979–987
Levy MM (2004) PEEP in ARDS—how much is enough? N Engl J Med 351:389–391
Hsu RL, Kaye AD, Urman RD (2013) Anesthetic challenges in robotic-assisted urologic surgery. Rev Urol 15:178–184
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
M. Hur, S.-K. Park, D. E. Jung, S. Yoo, J.-Y. Choi, W. H. Kim, J.T. Kim and J.-H. Bahk declare that they have no competing interests.
This study was approved by the Institutional Review Board of Seoul National University Hospital (register number 1609-102-793). All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all participants in the study.
Caption Electronic Supplementary Material
101_2018_486_MOESM2_ESM.docx
ESM2_Table 1. Combined results of arterial blood gas analysis, respiratory mechanics and hemodynamic parameters according to the I:E of 1:1 or 1:2 regardless of the study group
Rights and permissions
About this article
Cite this article
Hur, M., Park, SK., Jung, D.E. et al. Effect of prolonged inspiratory time on gas exchange during robot-assisted laparoscopic urologic surgery. Anaesthesist 67, 859–867 (2018). https://doi.org/10.1007/s00101-018-0486-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00101-018-0486-6