Abstract
Purpose
To compare the outcomes of distal neurotomy (DN) versus proximal neurotomy (PN) for the surgical management of painful neuromas in amputees and non-amputees, whether used in passive or active treatment.
Methods
A retrospective study was conducted on patients who underwent surgery for painful traumatic neuromas between 2019 and 2022. DN with neuroma excision was performed at the level of the injury or amputation. PN was performed using a separate proximal approach without neuroma excision. Outcomes included a Numerical Rating Scale (NRS) score and Patient-Reported Outcomes Measurement Information System (PROMIS) scores, as well as patients’ subjective assessments.
Results
A total of 33 patients were included: 17 amputees and 16 non-amputees. They totalized 43 neuromas treated by DN in 21 cases and PN in 22 cases. At the median follow-up time of 13 months, there were significant decreases in all NRS and PROMIS scores in the whole series. The decrease in limb pain scores was not significantly different between groups, except for the decrease in pain interference and patient satisfaction which were higher in the DN group. Sub-group analyses found the same significant differences in amputees. Targeted muscle reinnervation (TMR) was associated with a higher decrease in PROMIS scores.
Conclusion
DN seemed to give better results in amputees but there were confusing factors related to associated lesions. In other situations, the non-inferiority of PN was demonstrated. PN could be of interest for treating neuromas of superficial sensory nerves, for avoiding direct revision of a well-fitted stump and in conjunction with TMR.




Similar content being viewed by others
Data availability
No datasets were generated or analysed during the current study.
Abbreviations
- NRS:
-
numerical rating scale
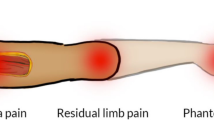
- PLP:
-
phantom limb pain
- PROMIS:
-
patient-reported outcome measurement information system
- TMR:
-
targeted muscle reinnervation
References
Eberlin KR, Ducic I. Surgical algorithm for neuroma management: a changing treatment paradigm. Plast Reconstr Surg Glob Open. 2018;6:e1952.
Domeshek LF, Krauss EM, Snyder-Warwick AK, Laurido-Soto O, Hasak JM, Skolnick GB, et al. Surgical treatment of neuromas improves patient-reported pain, depression and quality of life. Plast Reconstr Surg. 2017;139:407–18.
Nyman E, Dahlin E, Gudinge H, Dahlin LB. Surgically treated neuroma in upper extremity: patients characteristics and factors influencing outcome of surgery. Plast Reconstr Surg Glob Open. 2022;10:e4076.
Dumanian GA, Potter BK, Mioton LM, Ko JH, Cheesborough JE, Souza JM, et al. Targeted muscle reinnervation treats neuroma and phantom pain in major limb amputees. A randomized clinical trial. Ann Surg. 2019;270:238–46.
Souza JM, Cheesborough JE, Ko JH, Cho MS, Kuiken TA, Dumanian GA. Targeted muscle reinnervation: a novel approach to postamputation neuroma pain. Clin Orthop Relat Res. 2014;472:2984–90.
Chiodo CP, Miller SD. Surgical treatment of superficial peroneal neuroma. Foot Ankle Int. 2004;25:689–94.
Lans J, Gamo L, DiGiovanni CW, Chen NC, Eberlin KR. Etiology and treatment outcomes for sural neuroma. Foot Ankle Int. 2019;40:545–52.
Mathieu L, Diner C, Aries P, Thomas M, Truffaut S, de L’escalopier N. Preemptive targeted muscle reinnervation: the single incision approach should be avoided in trans-tibial traumatic amputation. Mil Med Res. 2022;9:60.
Dellon AL, Mackinnon SE. Treatment of the painful neuroma by neuroma resection and muscle implantation. Plast Reconstr Surg. 1986;77:427–38.
Goldstein SA, Sturim HS. Intraosseous nerve transposition for treatment of painful neuromas. J Hand Surg Am. 1985;10:270–4.
Sallaffi F, Stancati A, Silvestri CA, Ciapetti A, Grassi W. Minimal clinically important changes in chronic musculoskeletal pain intensity measured on a numerical rating scale. Eur J Pain. 2004;8:283–91.
Chen W, Revicki D, Amtmann D, Jensen M, Keefe F, Cella D. Development and analysis of PROMIS pain intensity scale. Qual Life Res. 2012;20:18.
Askew RL, Cook KF, Keefe FJ, Nowinski CJ, Cella D, Revicki DA, et al. A PROMIS measure of neuropathic pain quality. Value Health. 2016;19:623–30.
Revicki DA, Chen WH, Harnam N, Cook KF, Amtmann D, Callahan LF, et al. Development and psychometric analysis of the PROMIS pain behavior item bank. Pain. 2009;146:158–69.
Amtmann D, Cook KF, Jensen MP, Chen WH, Choi S, Revicki D, et al. Development of a PROMIS item bank to measure pain interference. Pain. 2010;150:173–82.
Cella D, Riley W, Stone A, Rothrock N, Reeve B, Yount S, et al. The patient-reported outcomes Measurement Information System (PROMIS) developed and testes its first wave of adult self-reported health outcome item banks: 2005–2008. J Clin Epidemiol. 2010;63:1179–94.
Haute Autorité de Santé. Qualité des soins perçue par le patient– Indicateurs PROMs et PREMs Panorama d’expériences étrangères et principaux enseignements. Rapport du 1er juillet 2021. https://www.has-sante.fr/upload/docs/application/pdf/2021-07. Accessed 1 December 2021.
Brakkee EM, Stokvis A, DeVinney E, Ducic I, Coert JH. Surgical treatment strategies for injuries of the unforgiving superficial branch of the radial nerve. Plast Reconstr Surg. 2022;150:8453.
Gart MS, Souza JM, Dumanian GA. Targeted muscle reinnervation in the upper extremity amputee: a technical roadmap. J Hand Surg Am. 2015;40:e1877–88.
Potter BK, Burns TC, Lacap AP, Granville RR, Gajewski DA. Heterotopic ossification following traumatic and combat-related amputations. Prevalence, risk factors, and preliminary results of excision. J Bone Joint Surg Am. 2007;89:476–86.
Mioton LM, Dumanian GA, Shah N, Qiu CS, Ertl WJ, Potter BK, et al. Targeted muscle reinnervation improves residual limb pain, phantom limb pain, and limb function: a prospective study of 33 major limb amputees. Clin Orthop Relat Res. 2020;478:2161–7.
Valerio IL, Dumanian GA, Jordan SW, Mioton LM, Bowen JB, West JM, et al. Preemptive treatment of phantom and residual pain with targeted muscle reinnervation at the time of major limb amputation. J Am Coll Surg. 2019;228:217–26.
Hoyt BW, Gibson JA, Potter BK, Souza JM. Practice patterns and pain outcomes for targeted muscle reinnervation: an informed approach to targeted muscle reinnervation use in the acute amputation setting. J Bone Joint Surg Am. 2021;103:681–7.
Chang BL, Mondshine J, Attinger CE, Kleiber GM. Targeted muscle reinnervation improves Pain and Ambulation outcomes in highly comorbid amputees. Plast Reconstr Surg. 2021;48:376–86.
Chang BL, Harbour P, Mondshine J, Kleiber GM. Targeted muscle reinnervation to expendable motor nerves for the treatment of refractory symptomatic neuromas in nonamputees. Plast Reconstr Surg Glob Open. 2021;9:e3436.
Van Opijnen MP, Hazelbag HM, de Ruiter GCW. Targeted muscle reinnervation for a recurrent traumatic neuroma of the sural nerve: illustrative case. J Neurosurg Case Lessons. 2022;3:CASE2264.
Funding
There is no funding source.
Author information
Authors and Affiliations
Contributions
A.C., J.N.B., L.M. and Z.B. operated the patients. A.L.P., A.M., C.R., and S.A. collected the data. L.M. supervised the study and analyzed the data. A.L.P. and L.M. and wrote the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
This study was approved by our review board (Protocol No 42-2019 HIA-CS).
Consent for publication
Informed consent was obtained from all individual participants included in the study.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lemaire-Petit, A., Milaire, A., Amar, S. et al. Surgical treatment of painful neuroma in amputated and non-amputated patients: does the level of neurotomy affect clinical outcomes?. Eur J Trauma Emerg Surg (2024). https://doi.org/10.1007/s00068-024-02529-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00068-024-02529-4