Abstract
Purpose
Early administration and protocolization of massive hemorrhage protocols (MHP) has been associated with decreases in mortality, multiorgan system failure, and number of blood products used. Various prediction tools have been developed for the initiation of MHP, but no single tool has demonstrated strong prediction with early clinical data. We sought to develop a massive transfusion prediction model using machine learning and early clinical data.
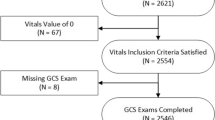
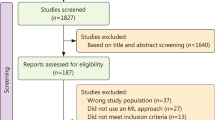
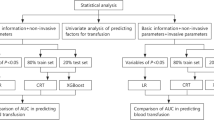
Methods
Using the National Trauma Data Bank from 2013 to 2018, we included severely injured trauma patients and extracted clinical features available from the pre-hospital and emergency department. We subsequently balanced our dataset and used the Boruta algorithm to determine feature selection. Massive transfusion was defined as five units at 4 h and ten units at 24 h. Six machine learning models were trained on the balanced dataset and tested on the original.
Results
A total of 326,758 patients met our inclusion with 18,871 (5.8%) requiring massive transfusion. Emergency department models demonstrated strong performance characteristics with mean areas under the receiver-operating characteristic curve of 0.83. Extreme gradient boost modeling slightly outperformed and demonstrated adequate predictive performance with pre-hospital data only, as well as 4-h transfusion thresholds.
Conclusions
We demonstrate the use of machine learning in developing an accurate prediction model for massive transfusion in trauma patients using early clinical data. This research demonstrates the potential utility of artificial intelligence as a clinical decision support tool.


Similar content being viewed by others
Data availability
The anonymized data collected for this study is available via the National Trauma Data Bank participant use file online data repository: https://www.facs.org/quality-programs/trauma/quality/national-trauma-data-bank/datasets/
References
Mathers CD, Boerma T, Ma Fat D. Global and regional causes of death. Br Med Bull. 2009;92:7–32.
Mathes T, Mosch C, Eikermann M. Economic aspects of trauma care. The poly-traumatized patient with fractures. Springer Berlin Heidelberg; 2016. p. 9–14.
Cotton BA, Au BK, Nunez TC, Gunter OL, Robertson AM, Young PP. Predefined massive transfusion protocols are associated with a reduction in organ failure and postinjury complications. J Trauma Inj Infect Crit Care. 2009;66:41–8.
Meyer DE, Vincent LE, Fox EE, O’Keeffe T, Inaba K, Bulger E, et al. Every minute counts: time to delivery of initial massive transfusion cooler and its impact on mortality. J Trauma Acute Care Surg. 2017;83:19–24.
Shih AW, Al Khan S, Wang AYH, Dawe P, Young PY, Greene A, et al. Systematic reviews of scores and predictors to trigger activation of massive transfusion protocols. J Trauma Acute Care Surg. 2019;87:717–29.
Ogura T, Lefor AK, Masuda M, Kushimoto S. Modified traumatic bleeding severity score: early determination of the need for massive transfusion. Am J Emerg Med. 2016;34:1097–101.
Nunez TC, Voskresensky IV, Dossett LA, Shinall R, Dutton WD, Cotton BA. Early prediction of massive transfusion in trauma: simple as ABC (Assessment of Blood Consumption)? J Trauma Inj Infect Crit Care. 2009;66:346–52.
Yin G, Radulovic N, O’Neill M, Lightfoot D, Nolan B. Predictors of transfusion in trauma and their utility in the prehospital environment: a scoping review. Prehospital Emerg Care. 2022;27:575.
Deo RC. Machine learning in medicine. Circulation. 2015;132:1920–30.
Hanson CW, Marshall BE. Artificial intelligence applications in the intensive care unit. Crit Care Med. 2001;29:427–35.
Rosenberg AL. Recent innovations in intensive care unit risk-prediction models. Curr Opin Crit Care. 2002;8:321–30.
Liu NT, Salinas J. Machine learning for predicting outcomes in trauma. Shock. 2017;48:504–10.
Gorczyca MT, Toscano NC, Cheng JD. The trauma severity model: an ensemble machine learning approach to risk prediction. Comput Biol Med. 2019;108:9–19.
Mitterecker A, Hofmann A, Trentino KM, Lloyd A, Leahy MF, Schwarzbauer K, et al. Machine learning–based prediction of transfusion. Transfusion (Paris). 2020;60:1977–86.
Lammers D, Marenco C, Morte K, Conner J, Williams J, Bax T, et al. Machine learning for military trauma: novel massive transfusion predictive models in combat zones. J Surg Res. 2022;270:369–75.
Seheult JN, Anto VP, Farhat N, Stram MN, Spinella PC, Alarcon L, et al. Application of a recursive partitioning decision tree algorithm for the prediction of massive transfusion in civilian trauma: the MTPitt prediction tool. Transfusion (Paris). 2019;59:953–64.
Nederpelt CJ, Mokhtari AK, Alser O, Tsiligkaridis T, Roberts J, Cha M, et al. Development of a field artificial intelligence triage tool: Confidence in the prediction of shock, transfusion, and definitive surgical therapy in patients with truncal gunshot wounds. J Trauma Acute Care Surg. 2021;90:1054–60.
Peng HT, Siddiqui MM, Rhind SG, Zhang J, Teodoro da Luz L, Beckett A. Artificial intelligence and machine learning for hemorrhagic trauma care. Mil Med Res. 2023;10:1–20. https://doi.org/10.1186/s40779-023-00444-0.
Nolan B, Hicks C, Petrosoniak A, Jung J, Grantcharov T. Pushing boundaries of video review in trauma: using comprehensive data to improve the safety of trauma care. Trauma Surg Acute Care Open. 2020;5: e000510.
Collins GS, Reitsma JB, Altman DG, Moons KGM. Transparent reporting of a multivariable prediction model for individual prognosis or diagnosis (TRIPOD): the TRIPOD Statement. BMC Med. 2015;13:1–10.
Cone JT, Benjamin ER, Alfson DB, Demetriades D. Isolated severe blunt traumatic brain injury: effect of obesity on outcomes. J Neurosurg. 2020;1:1–8.
Gomez D, Haas B, Hemmila M, Pasquale M, Goble S, Neal M, et al. Hips can lie: impact of excluding isolated hip fractures on external benchmarking of trauma center performance. J Trauma Inj Infect Crit Care. 2010;69:1037–41.
Zatta AJ, Mcquilten ZK, Mitra B, Roxby DJ, Sinha R, Whitehead S, et al. Elucidating the clinical characteristics of patients captured using different definitions of massive transfusion. Vox Sang. 2014;107:60–70.
McQuilten ZK, Crighton G, Brunskill S, Morison JK, Richter TH, Waters N, et al. Optimal dose, timing and ratio of blood products in massive transfusion: results from a systematic review. Transfus Med Rev. 2018; 6–15.
Oshiro TM, Perez PS, Baranauskas JA. How many trees in a random forest? Lecture Notes in Computer Science (including subseries Lecture Notes in Artificial Intelligence and Lecture Notes in Bioinformatics). 2012;7376 LNAI:154–68. https://doi.org/10.1007/978-3-642-31537-4_13.
Fischer JE, Bachmann LM, Jaeschke R. A readers’ guide to the interpretation of diagnostic test properties: clinical example of sepsis. Intensive Care Med. 2003;29:1043–51.
Ogura T, Nakamura Y, Nakano M, Izawa Y, Nakamura M, Fujizuka K, et al. Predicting the need for massive transfusion in trauma patients: the Traumatic Bleeding Severity Score. J Trauma Acute Care Surg. 2014;76:1243–50.
Kalkwarf KJ, Goodman MD, Press GM, Wade CE, Cotton BA. Prehospital ABC score accurately forecasts patients who will require immediate resource utilization. South Med J. 2021;114:193–8.
Yeates EO, Grigorian A, Inaba K, Dolich M, Schubl SD, Lekawa M, et al. Blunt trauma massive transfusion (B-MaT) score: a novel scoring tool. J Surg Res. 2022;270:321–6.
Strickland M, Nguyen A, Wu S, Suen SC, Mu Y, Del Rio Cuervo J, et al. Assessment of machine learning methods to predict massive blood transfusion in trauma. World J Surg. 2023;47:2340–6. https://doi.org/10.1007/s00268-023-07098-y.
Chow JH, Richards JE, Galvagno SM, Coleman PJ, Lankford AS, Hendrix C, et al. The algorithm examining the risk of massive transfusion (ALERT) score accurately predicts massive transfusion at the scene of injury and on arrival to the trauma bay: a retrospective analysis. Shock. 2021;56:529–36. Available from: https://journals.lww.com/shockjournal/fulltext/2021/10000/the_algorithm_examining_the_risk_of_massive.7.aspx
Lucas B, Hempel D, Otto R, Brenner F, Stier M, Marzi I, et al. Prehospital FAST reduces time to admission and operative treatment: a prospective, randomized, multicenter trial. Eur J Trauma Emerg Surg. 2022;48:2701–8. https://doi.org/10.1007/s00068-021-01806-w.
Zhang T, Nikouline A, Lightfoot D, Nolan B. Machine learning in the prediction of trauma outcomes: a systematic review. Ann Emerg Med. 2022;80:440–55.
Nauta M, Walsh R, Dubowski A, Seifert C. Uncovering and correcting shortcut learning in machine learning models for skin cancer diagnosis. Diagnostics. 2022;12:40.
Zielinski MD, Stubbs JR, Berns KS, Glassberg E, Murdock AD, Shinar E, et al. Prehospital blood transfusion programs: capabilities and lessons learned. J Trauma Acute Care Surg. 2017;82:S70–8.
Lee SM, Lee G, Kim TK, Le T, Hao J, Jung YM, et al. Development and validation of a prediction model for need for massive transfusion during surgery using intraoperative hemodynamic monitoring data. JAMA Netw Open. 2022;5:e2246637–e2246637.
Park C, Loza-Avalos SE, Harvey J, Hirschkorn C, Dultz LA, Dumas RP, et al. A real-time automated machine learning algorithm for predicting mortality in trauma patients: survey says it’s ready for prime-time. Am Surg. 2023. https://doi.org/10.1177/00031348231207299.
Starr AJ, Julka M, Nethi A, Watkins JD, Fairchild RW, Rinehart D, et al. Parkland trauma index of mortality: real-time predictive model for trauma patients. J Orthop Trauma. 2022;36:280–6.
Park C, Loza-Avalos S, Harvey J, Sadlowski M, Crigger M, Dumas R, et al. Implementation of an automated, real-time machine learning algorithm predicting mortality in trauma patients: survey says ready for prime time. J Am Coll Surg. 2022;235:S284–S284.
Roudsari B, Field C, Caetano R. Clustered and missing data in the US National Trauma Data Bank: Implications for analysis. Inj Prev. 2008;14:96–100.
Glance LG, Osler TM, Mukamel DB, Meredith W, Dick AW. Impact of statistical approaches for handling missing data on trauma center quality. Ann Surg. 2009;249:143–8.
Kostick-Quenet KM, Cohen IG, Gerke S, Lo B, Antaki J, Movahedi F, et al. Mitigating racial bias in machine learning. J Law Med Ethics. 2022;50:92–100.
Haider AH, Chang DC, Efron DT, Haut ER, Crandall M, Cornwell EE. Race and insurance status as risk factors for trauma mortality. Arch Surg. 2008;143:945–9.
Acknowledgements
We would like to acknowledge Dr. David Gomez for his expertise in the NTDB and assisting in our methods, the Li Ka Shing Institute for providing the computers necessary to run our models, and Physician Services Incorporated and the St. Michael’s Hospital Association Alternate Funds Plan for their financial support for this study.
Funding
BN was supported by Physician Services Incorporated and the St. Michael’s Hospital Association Alternate Funds Plan. The funders did not have a role in study design, data analysis, interpretation of the results, writing the manuscript, or submitting the article for publication.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr Nathens works for the American College of Surgeons as the director of the Trauma Quality Improvement Program and has oversight of the database used for this analysis. No other authors have any disclosures to report.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Nikouline, A., Feng, J., Rudzicz, F. et al. Machine learning in the prediction of massive transfusion in trauma: a retrospective analysis as a proof-of-concept. Eur J Trauma Emerg Surg (2024). https://doi.org/10.1007/s00068-023-02423-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00068-023-02423-5