Abstract
Background
Some studies lack detailed analyses of the differences and characteristics of pediatric injury mechanisms between urban and rural areas.
Objective
We aim to understand the characteristics, trends, and mortality rates of injury mechanisms in children in urban and rural areas in central China.
Results
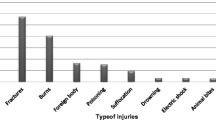
In a study involving 15,807 pediatric trauma patients, it was observed that boys constituted the majority (65.4%) and those aged ≤ 3 years were the most prevalent (28.62%). Falls (39.8%), burns (23.2%), and traffic accidents (21.1%) were identified as the top three injury mechanisms. The head (29.0%) and limbs (35.7%) were found to be the most susceptible to injury. Additionally, children between the ages of 1–3 years exhibited a higher likelihood of sustaining burn injuries compared to other age groups. The main causes of burn injury were hydrothermal burns (90.3%), flame burns (4.9%), chemical burns (3.5%), and electronic burns (1.3%). In urban areas, the major injury mechanisms were falls (40.9%), traffic accidents (22.4%), burns (20.9%), and poison (7.1%), whereas, in rural areas, they were falls (39.5%), burns (23.8%), traffic accidents (20.8%), and penetration (7.0%). Over the past decade, the overall incidences of pediatric trauma have been decreasing. In the past year, the number of injured children was the highest in July, and the overall mortality rate due to trauma was 0.8%.
Conclusion
Our findings revealed that in different age groups, the injury mechanisms are different in urban and rural areas. Burns are the second leading cause of trauma in children. A decrease in pediatric trauma over the past 10 years indicates targeted measures and preventive intervention may effectively prevent pediatric trauma.


Similar content being viewed by others
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Kyu HH, Pinho C, Wagner JA, et al. Global and national burden of diseases and injuries among children and adolescents between 1990 and 2013: Findings from the global burden of disease 2013 Study. JAMA Pediatr. 2016;170:267–87.
Yin X, Dai W, Yukai Du, et al. The injury mechanisms and injury pyramids among children and adolescents in Zhuhai City. China BMC Public Health. 2021;21(436):1–11.
de Vries AP, Kassam-Adams N, Cnaan A, et al. Looking beyond the physical injury: posttraumatic stress disorder in children and parents after pediatric traffic injury. Pediatrics. 1999;104(6):1293–9.
Naumann RB, Dellinger AM, Zaloshnja E, et al. Incidence and total lifetime costs of motor vehicle–related fatal and nonfatal injury by road user type, United States, 2005. Traffic Inj Prev. 2010;11(4):353–60.
Hedström EM, Bergström U, Michno P. Injuries in children and adolescents–analysis of 41,330 injury related visits to an emergency department in northern Sweden. Injury. 2012;43:1403–8.
Keys Joni, Dempster Martin, Jackson Jonathan, et al. The psychosocial impact of losing an eye through traumatic injury and living with prosthetic restoration: A thematic analysis. J ActPsy. 2021; 219.
Wolyncewicz GEL, Palmer CS, Jowett HE, et al. Horse-related injuries in children-unmounted injuries are more severe: A retrospective review. Injury. 2018;49.
Burrows S, Auger N, Lo E. Language and unintentional injury mortality in Quebec. Canada Inj Prev. 2016;22(1):72–5.
Matzopoulos R, Prinsloo M, Pillay-van Wyk V, et al. Injury-related mortality in South Africa: a retrospective descriptive study of postmortem investigations. Bull World Health Organ. 2015;93(5):303–13.
Lin Y, Chen M, Chen G, et al. Application of an autoregressive integrated moving average model for predicting injury mortality in Xiamen, China. BMJ Open. 2015;5(12): e008491.
Makoto Aoki, Toshikazu Abe, Daizoh Saitoh, et al. Epidemiology, patterns of treatment, and mortality of pediatric trauma patients in Japan. Scientific Reports. 2019;9(1).
Jones S , Tyson S , Young M , et al. Patterns of moderate and severe injury in children after the introduction of major trauma networks. Arch Dis Child. 2018;0:1–6.
Sethi D, Aldridge E, Rakovac I, et al. Worsening inequalities in child injury deaths in the WHO European region. Int J Environ Res Public Health. 2017;14(10):1–8.
Garay M, Hess J, Armstrong D, et al. Pediatric ATV Injuries in a Statewide Sample: 2004 to 2014. Pediatrics. 2017;140(2): e20170945.
Esteban E, Bujaldon E, Esparza M, et al. Sex differences in children with severe health conditions: Causes of admission and mortality in a Pediatric Intensive Care Unit. Am J Hum Biol. 2015;27:613–9.
Mitchell RJ, Curtis K, Foster K. A 10-year review of child injury hospitalizations, health outcomes and treatment costs in Australia. Inj Prev. 2017; injuryprev-2017–042451.
Park ES, Yang HJ, Park JB. Pediatric Traumatic Brain Injury : The Epidemiology in Korea. J Korean Neurosurg Soc. 2022;65(3):334–41.
Qiu X, Deng H, Su Q, et al. Epidemiology and management of 10,486 pediatric fractures in Shenzhen: experience and lessons to be learnt. BMC Pediatr. 2022;22(1):161.
Liang W, Zhu K, Dai W, et al. Epidemiological characteristics of injury deaths among 0–14 year old children in Zhuhai from 2006 to 2017. Injury Medicine. 2020;9(2):24–9.
Rivara FP, Thompson DC, Beahler C, et al. Systematic reviews of strategies to prevent motor vehicle injuries. Am J Prev Med. 1999;16(Suppl 1):1–5.
Zhang X, Chen B, Hou B, et al. Analysis on the death of children and adolescents aged 0–14 years in Xi ’an. School Health in China. 2016;37(1):74–7.
Ping M , Hussain N , Abbe M . An examination of traffic-related traumatic injuries among children at a Level-1 pediatric trauma center, 2005–2014. J Trauma Acute Care Surg. 2017; 83(5S Suppl 2):S233.
Trauma Audit Research Network. 2 years of severe injury in children. Manchester, England: Trauma Audit Research Network. 2016.
Anderson P. Assessment and development of executive function (EF) during childhood. Child Neuropsychol. 2002;8:71–82.
Haagsma JA, Graetz N, Bolliger I, et al. The global burden of injury: incidence, mortality, disability-adjusted life years and time trends from the global burden of disease study 2013. Inj Prev. 2016;22(1):3–18.
Mitchell RJ, Chong SL. Comparison of injury-related hospitalized morbidity and mortality in urban and rural areas in Australia. Rural Remote Health. 2010;10(1):1326. 20230166.
Kristiansen T, Rehn M, Gravseth HM, et al. Paediatric trauma mortality in Norway: a population-based study of injury characteristics and urban-rural differences. Injury. 2012;43(11):1865–72.
Staton C, Vissoci J, Gong E, et al. Road traffic injury prevention initiatives: a systematic review and metasummary of effectiveness in low and middle income countries. PLoS ONE. 2016;11(1): e0144971.
McBride DL. Children and outdoor play. J Pediatr Nurs. 2012;27:421–2.
Beck B, Teague W, Cameron P, et al. Causes and characteristics of injury in paediatric major trauma and trends over time. Arch Dis Child. 2019;104:256–61.
Snyder CW, Muensterer OJ, Sacco F, et al. Paediatric trauma on the Last Frontier: an 11-year review of injury mechanisms, high-risk injury patterns and outcomes in Alaskan children. Int J Circumpolar Health. 2014;73:25066.
Macedo JL, Santos JB. Predictive factors of mortality in burn patients. Rev Inst Med Trop Sao Paulo. 2007;49:365–70.
Mashreky SR, Rahman A, Chowdhury SM, et al. Epidemiology of childhood burn: yield of largest community based injury survey in Bangladesh. Burns. 2008;34:856–62.
Mathers C, Fat DM, Boerma JT. The global burden of disease: 2004 update. Geneva: World Health Organization; 2008.
Lang C, Guofu Z, Qian Z, et al. Epidemiological investigation of 1330 hospitalized burn children. Chinese J burn. 2018;34(2):111–3.
Yingxia W, Yang Zuxian Xu, Ling. Investigation on burn prevention awareness and nursing countermeasures of caregivers of burn children in Huizhou. Yunnan medicine. 2020;42(3):284–93.
Elliot AJ, Cross KW, Fleming DM. Acute respiratory infections and winter pressures on hospital admissions in England and Wales 1990–2005. J Public Health. 2008;30:91–8.
Department of Health and Social Care. NHS 7 day services: Information on the government’s plans for the NHS to provide a 7 day service by 2020. 2015, https://www.gov.uk/government/collections/nhs-7-day-services (Accessed December 1 2017).
Acknowledgements
The authors would like to thank all relative hospitals for their support and help in providing the data required for the study. The authors would also like to thank our colleagues for their guidance in data analysis.
Funding
This manuscript is independent research supported by the Science and Technology Planning Project in Wuhu (2021jc2–4).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Yuanying Yao, Lijuan Ma, and Lei Chen declare that they have no conflict of interest.
Patient consent
Not required.
Provenance and peer review
Not commissioned; externally peer reviewed.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yao, Y., Ma, L. & Chen, L. Characteristics of injury mechanisms in children and differences between urban and rural areas in central China. Eur J Trauma Emerg Surg 49, 2459–2466 (2023). https://doi.org/10.1007/s00068-023-02320-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-023-02320-x