Abstract
Purpose
The objective of this systematic review was to perform epidemiological as well as clinical, radiological and patient-reported outcome analysis of surgically treated perilunate dislocations and fracture dislocations (PLDs and PLFDs) based on the so far largest pooled patient population to date.
Material and methods
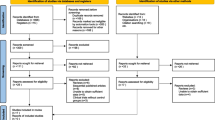
This systematic review was written according to the updated guideline for reporting systematic reviews by the Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) statement. A comprehensive literature search of Pubmed, Embase, CENTRAL, and CINAHL databases was performed. All studies reporting on complications, radiological, functional and/or patient-reported outcomes of surgically treated acute PLDs and PLFDs with a minimum follow-up of 12 months were included.
Results
Twenty-six studies encompassing 550 patients with 553 operatively treated acute perilunate injuries (106 PLDs and 447 PLFDs) were included. The overall postoperative complication rate was 15.0% with secondary reduction loss representing the main contributing factor (10.1%). The overall reoperation rate was 10.4% and the incidence of salvage procedures was 2.8%. The risk for secondary reduction loss was higher for PLD than for PLFD injuries (24.2% vs. 7.0%, relative risk [RR] 3.5, 95% confidence interval [CI] 1.6–7.5). There was a higher overall complication rate for the combined dorsopalmar approach when compared to the isolated dorsal approach (17.4% vs. 8.4%, RR 0.5, 95% CI 0.2–1.0, number needed to treat [NNT] 11.2) and for open surgery versus arthroscopic surgery (17.4% vs. 4.8%, RR 0.3, 95% CI 0.1–0.9, NNT 8.0). A significant correlation was found between radiological osteoarthritis (rOA) and follow-up duration of the individual studies, while functional and patient-rated outcomes were comparable.
Conclusions
Regardless of surgical technique, PLFDs appear to be less susceptible to secondary reduction loss than PLDs. Whenever possible, less invasive (e.g. arthroscopic) surgery should be performed to minimize postoperative complications. The rate of rOA is high and increases significantly with follow-up duration. Interestingly, rOA does not seem to correlate with reduced wrist function nor patient dissatisfaction and the need for salvage surgery is surprisingly rare.
Level of evidence: Systematic review of level IV studies.



Similar content being viewed by others
Data availability
The raw and metadata of this systematic literature review are on file with the corresponding author and can be made available upon request.
References
Najarian R, Nourbakhsh A, Capo J, Tan V. Perilunate injuries. Hand (N Y). 2011;6:1–7. https://doi.org/10.1007/S11552-010-9293-5.
Apergis E, Maris J, Theodoratos G, Pavlakis D, Antoniou N. Perilunate dislocations and fracture-dislocations. Closed and early open reduction compared in 28 cases. Acta Orthop Scand. 1997;275:55–9.
Krief E, Appy-Fedida B, Rotari V, David E, Mertl P, Maes-Clavier C. Results of perilunate dislocations and perilunate fracture dislocations with a minimum 15-year follow-up. J Hand Surg Am. 2015;40:2191–7. https://doi.org/10.1016/J.JHSA.2015.07.016.
Herzberg G, Comtet J, Linscheid R, Amadio P, Cooney W, Stalder J. Perilunate dislocations and fracture-dislocations: a multicenter study. J Hand Surg (Am Vol Surg). 1993;18:768–79. https://doi.org/10.1016/0363-5023(93)90041-Z.
Zhang X, Wei Q, Ji F, Tong DK, Tang H, Zhang H, et al. Manipulative reduction and plaster external fixation for the treatment of the scaphoid fracture and perilunate dislocation. China J Orthop Traumatol. 2018;31:441–5. https://doi.org/10.3969/J.ISSN.1003-0034.2018.05.009.
Scalcione L, Gimber L, Ho A, Johnston S, Sheppard J, Taljanovic M. Spectrum of carpal dislocations and fracture-dislocations: imaging and management. Am J Roentgenol. 2014;203:541–50. https://doi.org/10.2214/AJR.13.11680.
Garg B, Goyal T, Kotwal P. Staged reduction of neglected transscaphoid perilunate fracture dislocation: a report of 16 cases. J Orthop Surg Res. 2012;7:19. https://doi.org/10.1186/1749-799X-7-19.
Garg B, Batra S. Chronic trans-scaphoid perilunate dislocation: current management protocol. J Clin Orthop Trauma. 2020;11:523–8. https://doi.org/10.1016/J.JCOT.2020.05.006.
van der Oest MJW, Duraku LS, Artan M, Hundepool CA, Power DM, Rajaratnam V, et al. Perilunate injury timing and treatment options: a systematic review. J Wrist Surg. 2021;11:164–76. https://doi.org/10.1055/S-0041-1735841.
Charalambous C, Mills S, Hayton M. Gradual distraction using an external fixator followed by open reduction in the treatment of chronic lunate dislocation. Hand Surg. 2010;15:27–9. https://doi.org/10.1142/S0218810410004436.
Gupta R, Kamboj K. Functional outcome after surgical treatment of perilunate injuries: a series of 12 cases. J Clin Orthop Trauma. 2016;7:7–11. https://doi.org/10.1016/J.JCOT.2015.09.005.
Muller T, Hidalgo Diaz JJ, Pire E, Prunières G, Facca S, Liverneaux P. Treatment of acute perilunate dislocations: ORIF versus proximal row carpectomy. Orthop Traumatol Surg Res. 2017;103:95–9. https://doi.org/10.1016/J.OTSR.2016.10.014.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. https://doi.org/10.1136/BMJ.N71.
Higgins JPT, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. https://doi.org/10.1136/BMJ.D5928.
Agoritsas T, Merglen A, Courvoisier DS, Combescure C, Garin N, Perrier A, et al. Sensitivity and predictive value of 15 PubMed search strategies to answer clinical questions rated against full systematic reviews. J Med Internet Res. 2012;14: e85. https://doi.org/10.2196/jmir.2021.
Ferguson DO, Shanbhag V, Hedley H, Reichert I, Lipscombe S, Davis TRC. Scaphoid fracture non-union: a systematic review of surgical treatment using bone graft. J Hand Surg Eur. 2016;41:492–500. https://doi.org/10.1177/1753193415604778.
Harden NR, Bruehl S, Perez RSGM, Birklein F, Marinus J, Maihofner C, et al. Validation of proposed diagnostic criteria (the “Budapest Criteria”) for complex regional pain syndrome. Pain. 2010;150:268–74. https://doi.org/10.1016/j.pain.2010.04.030.
Berriós-Torres SI, Umscheid CA, Bratzler DW, Leas B, Stone EC, Kelz RR, et al. Centers for disease control and prevention guideline for the prevention of surgical site infection, 2017. JAMA Surg. 2017;152:784–91. https://doi.org/10.1001/jamasurg.2017.0904.
Study Quality Assessment Tools | NHLBI, NIH n.d. https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools. Accessed 18 Jan 2022.
Risk of bias tools—ROBINS-I detailed guidance (2016) n.d. https://sites.google.com/site/riskofbiastool/welcome/home/current-version-of-robins-i/robins-i-detailed-guidance-2016. Accessed 12 Aug 2022.
Guyatt G, Oxman AD, Akl EA, Kunz R, Vist G, Brozek J, et al. GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. J Clin Epidemiol. 2011;64:383–94. https://doi.org/10.1016/J.JCLINEPI.2010.04.026.
Kim J, Lee J, Park M. Arthroscopic reduction and percutaneous fixation of perilunate dislocations and fracture-dislocations. Arthroscopy. 2012;28:196–203. https://doi.org/10.1016/J.ARTHRO.2011.08.299.
Kim J, Lee J, Park M. Arthroscopic treatment of perilunate dislocations and fracture dislocations. J Wrist Surg. 2015;4:81–7. https://doi.org/10.1055/S-0035-1550160.
Savvidou O, Beltsios M, Sakellariou V, Mavrogenis A, Christodoulou M, Papagelopoulos P. Use of external fixation for perilunate dislocations and fracture dislocations. Strateg Trauma Limb Reconstr. 2014;9:141–8. https://doi.org/10.1007/S11751-014-0201-3.
Savvidou O, Beltsios M, Sakellariou V, Papagelopoulos P. Perilunate dislocations treated with external fixation and percutaneous pinning. J Wrist Surg. 2015;4:076–80. https://doi.org/10.1055/S-0035-1550159.
Lebot G, Amouyel T, Hardy A, Chantelot C, Saab M. Perilunate fracture-dislocations: clinical and functional outcomes at a mean follow-up of 33 years. Orthop Traumatol Surg Res. 2021;107:102973. https://doi.org/10.1016/J.OTSR.2021.102973. (Epub 2021 May 27).
Wong T, Ip F. Minimally invasive management of trans-scaphoid perilunate fracture-dislocations. Hand Surg. 2008;13:159–65. https://doi.org/10.1142/S0218810408004018.
Knoll V, Allan C, Trumble T. Trans-scaphoid perilunate fracture dislocations: results of screw fixation of the scaphoid and lunotriquetral repair with a dorsal approach. J Hand Surg (Am Vol). 2005;30:1145–1145. https://doi.org/10.1016/J.JHSA.2005.07.007.
Herzberg G, Forissier D. Acute dorsal trans-scaphoid perilunate fracture-dislocations: medium-term results. J Hand Surg Am. 2002;27:498–502. https://doi.org/10.1054/JHSB.2002.0774.
Sotereanos D, Mitsionis G, Giannakopoulos P, Tomaino M, Herndon J. Perilunate dislocation and fracture dislocation: a critical analysis of the volar-dorsal approach. J Hand Surg Am. 1997;22:49–56. https://doi.org/10.1016/S0363-5023(05)80179-0.
Gabl M, Lutz M, Pechlaner S, Fink C. Perilunate dislocation and dislocation fractures—results of surgical management. Unfallchirurg. 1996;99:650–5. https://doi.org/10.1007/S001130050038.
Çolak I, Bulut G, Bekler H, Çeçen G, Gülabi D. Mid-term clinical and radiographic outcomes of perilunate injuries treated with open reduction and internal fixation. Acta Orthop Traumatol Turc. 2021;55:57–61. https://doi.org/10.5152/J.AOTT.2021.19246.
Hee HT, Wong HP, Med M, Low YP. Transscaphoid perilunate fracture/dislocations—results of surgical treatment. Ann Acad Med Singapore. 1999;28:791–4.
Meszaros T, Vögelin E, Mathys L, Leclère F. Perilunate fracture-dislocations: clinical and radiological results of 21 cases. Arch Orthop Trauma Surg. 2018;138:287–97. https://doi.org/10.1007/S00402-017-2861-1.
George J, Kumar K, Vijayakumar G, Ravishankar M. Functional outcome of surgically managed perilunate injuries. Indian J Orthop. 2020;54:270–6. https://doi.org/10.1007/S43465-020-00225-0.
Lameijer C, Niezen C, El Moumni M, van der Sluis C. Pain, impaired functioning, poor satisfaction and diminished health status eight years following perilunate (fracture) dislocations. Disabil Rehabil. 2020;42:849–56. https://doi.org/10.1080/09638288.2018.1512165.
Özyürekoğlu T, Acar M. Treatment of acute perilunate dislocation or fracture dislocation using dorsal approach and diamond-shaped Kirschner-wire fixation. Jt Dis Relat Surg. 2021;32:42–50. https://doi.org/10.5606/EHC.2021.74838.
Liu B, Chen S, Zhu J, Tian G. Arthroscopic management of perilunate injuries. Hand Clin. 2017;33:709–15. https://doi.org/10.1016/J.HCL.2017.06.002.
Griffin M, Roushdi I, Osagie L, Cerovac S, Umarji S. Patient-reported outcomes following surgically managed perilunate dislocation: outcomes after perilunate dislocation. Hand (N Y). 2016;11:22–8. https://doi.org/10.1177/1558944715617222.
Kremer T, Wendt M, Riedel K, Sauerbier M, Germann G, Bickert B. Open reduction for perilunate injuries—clinical outcome and patient satisfaction. J Hand Surg Am. 2010;35:1599–606. https://doi.org/10.1016/J.JHSA.2010.06.021.
Martinage A, Balaguer T, Chignon-Sicard B, Monteil M, Dréant N, Lebreton E. Perilunate dislocations and fracture-dislocations of the wrist, a review of 14 cases. Chir Main. 2008;27:31–9. https://doi.org/10.1016/J.MAIN.2007.10.006.
Hildebrand K, Ross D, Patterson S, Roth J, MacDermid J, King G. Dorsal perilunate dislocations and fracture-dislocations: questionnaire, clinical, and radiographic evaluation. J Hand Surg (Am Vol). 2000;25:1069–79. https://doi.org/10.1053/JHSU.2000.17868.
Savvidou OD, Beltsios M, Sakellariou VI, Papagelopoulos PJ. Perilunate dislocations treated with external fixation and percutaneous pinning. J Wrist Surg. 2015;4:76–80. https://doi.org/10.1055/S-0035-1550159.
Kural C, Tanriverdi B, Erçin E, Baca E, Yilmaz M. The surgical outcomes of trans-scaphoid perilunate fracture-dislocations. Turkish J Med Sci. 2020;50:25–30. https://doi.org/10.3906/SAG-1710-163.
Dunn J, Koehler L, Kusnezov N, Polfer E, Orr J, Pirela-Cruz M, et al. Perilunate dislocations and perilunate fracture dislocations in the U.S. Military. J Wrist Surg. 2018;7:57–65. https://doi.org/10.1055/S-0037-1603932.
Oh W, Choi Y, Kang H, Koh I, Lim K. Comparative outcome analysis of arthroscopic-assisted versus open reduction and fixation of trans-scaphoid perilunate fracture dislocations. Arthroscopy. 2017;33:92–100. https://doi.org/10.1016/J.ARTHRO.2016.07.018.
Kara A, Celik H, Seker A, Kilinc E, Camur S, Uzun M. Surgical treatment of dorsal perilunate fracture-dislocations and prognostic factors. Int J Surg. 2015;24:57–63. https://doi.org/10.1016/J.IJSU.2015.10.037.
Chou Y, Hsu Y, Cheng C, Wu C. Percutaneous screw and axial Kirschner wire fixation for acute transscaphoid perilunate fracture dislocation. J Hand Surg (Am Vol) 2012;37:715–720. https://doi.org/10.1016/J.JHSA.2012.01.019
Malović M, Pavić R, Milosević M. Treatment of trans-scaphoid perilunate dislocations using a volar approach with scaphoid osteosynthesis and temporary Kirschner wire fixation. Mil Med. 2011;176:1077–82. https://doi.org/10.7205/MILMED-D-10-00419.
Lutz M, Arora R, Kammerlander C, Gabl M, Pechlaner S. Stabilization of perilunate and transscaphoid perilunate fracture-dislocations via a combined palmar and dorsal approach. Oper Orthop Traumatol. 2009;21:442–58. https://doi.org/10.1007/S00064-009-1906-1.
Mühldorfer-Fodor M, Hohendorff B, Saalabian A, Hahne M, van Schoonhoven J, Prommersberger K. Median nerve neuropathy after perilunate dislocation injuries. Handchir Mikrochir Plast Chir. 2014;46:163–8. https://doi.org/10.1055/S-0034-1370959.
Schaller P, Grünert J. Late outcome after surgical treatment of perilunar dislocation and dislocation fractures. Handchir Mikrochir Plast Chir. 1998;30:298–302.
Forli A, Courvoisier A, Wimsey S, Corcella D, Moutet F. Perilunate dislocations and transscaphoid perilunate fracture-dislocations: a retrospective study with minimum ten-year follow-up. J Hand Surg (Am Vol) 2010;35:62–8. https://doi.org/10.1016/J.JHSA.2009.09.003
Gummesson C, Ward MM, Atroshi I. The shortened disabilities of the arm, shoulder and hand questionnaire (QuickDASH): validity and reliability based on responses within the full-length DASH. BMC Musculoskelet Disord. 2006;7:1–7. https://doi.org/10.1186/1471-2474-7-44/FIGURES/1.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
All listed authors have made substantial contributions to this article. The design and conception of the work, analysis, and interpretation of data was carried out by RL, DNM and SH. RL wrote the first draft of the manuscript. Critical revision for important intellectual content as well as final approval of the version to be published was done by AOG, BJMVDW and EV. All authors agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval
Not applicable.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Liechti, R., Merky, D.N., Grobbelaar, A.O. et al. Outcomes of acute perilunate injuries—a systematic review. Eur J Trauma Emerg Surg 49, 2071–2084 (2023). https://doi.org/10.1007/s00068-023-02222-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-023-02222-y