Abstract
Purpose
Emergency surgery carries an increased risk of death and complications. Scoring systems can help identify patients at higher risk of mortality and complications. Scoring systems can also help benchmark acute care services. This study aims to compare different scoring systems in predicting outcomes among acute care surgery patients.
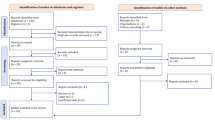
Methods
Our study is a retrospective cohort study that included all adult emergency surgery admissions between 2017 and 2019. Data were obtained from patients' electronic health records. Same admission mortality and postoperative complications were collected. Data were recorded to calculate the American Society of Anesthesiologists Physical Status classification system (ASA-PS), Shock Index Score (SI), Age Shock Index Score (AgeSI), and the Emergency Surgery Score (ESS). The probability of death and complications was correlated with each scoring system and was assessed by calculating the c-statistic.
Results
During the study period, 1606 patients fulfilled inclusion criteria. The mortality rate was 2.2%, complication rate was 18.7%. ESS predicted mortality with a c-statistic of 0.87 better than ASA-PS, AgeSI, and SI with a calculated c-statistic of 0.81, 0.74, and 0.57, respectively. ESS also predicted the occurrence of complications with a c-statistic of 0.83 better than ASA-PS, AgeSI, and SI with a calculated c-statistic of 0.72, 0.71, and 0.63, respectively.
Conclusion
ESS demonstrated a better prognostic accuracy for hospital mortality and postoperative complications than other prognostic scoring systems. Our findings suggest that a scoring system designed for the acute care surgical population may provide enhanced prognostic performance over other surgical prognostic scoring systems.


Similar content being viewed by others
Data availability
The datasets analyzed during the current work are available from the corresponding author upon reasonable request.
References
Gale SC, Shafi S, Dombrovskiy VY, et al. The public health burden of emergency general surgery in the United States: a 10-year analysis of the Nationwide Inpatient Sample—2001 to 2010. J Trauma Acute Care Surg. 2014;77(2):202–8.
Wohlgemut JM, Ramsay G, Boyers D, Jansen JO. Current and projected financial burden of emergency general surgery for adults in Scotland’s Single Payer Healthcare System: a cost analysis of hospital admissions. Ann Surg. 2021;274(6):e522–8.
Mullen MG, Michaels AD, Mehaffey JH, et al. Risk associated with complications and mortality after urgent surgery vs elective and emergency surgery: implications for defining “Quality” and reporting outcomes for urgent surgery. JAMA Surg. 2017;152(8):768–74.
Havens JM, Peetz AB, Do WS, et al. The excess morbidity and mortality of emergency general surgery. J Trauma Acute Care Surg. 2015;78(2):306–11.
Neary WD, Prytherch D, Foy C, et al. Comparison of different methods of risk stratification in urgent and emergency surgery. Br J Surg. 2007;94(10):1300–5.
Havens JM, Columbus AB, Seshadri AJ, et al. Risk stratification tools in emergency general surgery. Trauma Surg Acute Care Open. 2018;3(1):e000160.
Mayhew D, Mendonca V, Murthy BVS. A review of ASA physical status—historical perspectives and modern developments. Anaesthesia. 2019;74(3):373–9.
Mutschler M, Nienaber U, Munzberg M, et al. The Shock Index revisited—a fast guide to transfusion requirement? A retrospective analysis on 21,853 patients derived from the TraumaRegister DGU. Crit Care. 2013;17(4):R172.
Owens WD, Felts JA, Spitznagel EL Jr. ASA physical status classifications: a study of consistency of ratings. Anesthesiology. 1978;49(4):239–43.
Wolters U, Wolf T, Stutzer H, Schroder T. ASA classification and perioperative variables as predictors of postoperative outcome. Br J Anaesth. 1996;77(2):217–22.
Allgower M, Burri C. Shock index. Dtsch Med Wochenschr. 1967;92(43):1947–50.
DeMuro JP, Simmons S, Jax J, Gianelli SM. Application of the Shock Index to the prediction of need for hemostasis intervention. Am J Emerg Med. 2013;31(8):1260–3.
Cannon CM, Braxton CC, Kling-Smith M, et al. Utility of the shock index in predicting mortality in traumatically injured patients. J Trauma. 2009;67(6):1426–30.
Montoya KF, Charry JD, Calle-Toro JS, et al. Shock index as a mortality predictor in patients with acute polytrauma. J Acute Dis. 2015;4(3):202–4.
Zarzaur BL, Croce MA, Fischer PE, et al. New vitals after injury: shock index for the young and age x shock index for the old. J Surg Res. 2008;147(2):229–36.
Kim SY, Hong KJ, Shin SD, et al. Validation of the Shock Index, modified Shock Index, and age Shock Index for predicting mortality of geriatric trauma patients in Emergency Departments. J Korean Med Sci. 2016;31(12):2026–32.
Sangji NF, Bohnen JD, Ramly EP, et al. Derivation and validation of a novel Physiological Emergency Surgery Acuity Score (PESAS). World J Surg. 2017;41(7):1782–9.
Nandan AR, Bohnen JD, Sangji NF, et al. The Emergency Surgery Score (ESS) accurately predicts the occurrence of postoperative complications in emergency surgery patients. J Trauma Acute Care Surg. 2017;83(1):84–9.
Peponis T, Bohnen JD, Sangji NF, et al. Does the Emergency Surgery Score accurately predict outcomes in emergent laparotomies? Surgery. 2017;162(2):445–52.
Hackett NJ, De Oliveira GS, Jain UK, Kim JY. ASA class is a reliable independent predictor of medical complications and mortality following surgery. Int J Surg. 2015;18:184–90.
Al Jalbout N, Balhara KS, Hamade B, et al. Shock Index as a predictor of hospital admission and inpatient mortality in a US National Database of Emergency Departments. Emerg Med J. 2019;36(5):293–7.
Reinstadler SJ, Fuernau G, Eitel C, et al. Shock Index as a predictor of myocardial damage and clinical outcome in ST-elevation myocardial infarction. Circ J. 2016;80(4):924–30.
Altamimi A, Hassanain M, Nouh T, et al. Predictors of morbidity and mortality post emergency abdominal surgery: a national study. Saudi J Gastroenterol. 2018;24(5):282–8.
Funding
This research did not receive any specific Grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Thamer Nouh, Norah Alkadi, Lamis Alsuwailem, Albatoul Alshanaifi, Rahaf Alshunaiber, and Ahmed Alburakan have no conflict of interest to disclose.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Nouh, T., Alkadi, N., Alsuwailem, L. et al. Comparison of different scoring systems in predicting mortality and postoperative complications in acute care surgery patients at a Saudi Academic Centre. Eur J Trauma Emerg Surg 49, 1321–1327 (2023). https://doi.org/10.1007/s00068-023-02218-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-023-02218-8