Abstract
Purpose
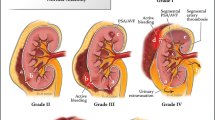
Pseudoaneurysms (PSA) can occur following high-grade solid organ injury. PSA natural history is unclear but risk for spontaneous rupture and exsanguination exist. The yield of delayed CT Angiography (dCTA) for PSA diagnosis is not well delineated and optimal timing is undefined. The study objective was definition of dCTA utility in diagnosing and triggering intervention for PSA after high-grade blunt solid organ injury.
Methods
All blunt trauma patients arriving to our ACS-verified Level 1 trauma center with AAST grade ≥ III liver, spleen, and/or kidney injury were included in this retrospective observational study (01/2017–10/2021). Exclusions were age < 18 year, transfers in, death < 48 h, and immediate nephrectomy/splenectomy. dCTA performance was not protocolized and pursued at attending surgeon discretion. Demographics, clinical/injury data, and outcomes were collected. Primary outcome was dCTA-triggered intervention. Statistical testing with ANOVA/Chi squared compared outcomes by type of solid organ.
Results
349 blunt trauma patients with 395 high-grade solid organ injuries met study criteria. Median AAST grade of solid organ injury was 3 [3–4]. dCTA for PSA screening was pursued in 175 patients (44%), typically on hospital day 4 [3–7]. dCTA identified vascular lesions in 16 spleen, 10 liver, and 6 kidney injuries. dCTA triggered intervention in 24% of spleen, 13% of kidney, and 9% of liver injured patients who were screened, for an overall yield of 14%. Intervention was typically AE (n = 23, 92%), although two splenic PSA necessitated splenectomy.
Conclusion
Delayed CTA for PSA screening after high-grade blunt solid organ injury was performed in half of eligible patients. dCTA identified numerous vascular lesions requiring endovascular or surgical intervention, with highest yield for splenic injuries. We recommend consideration of universal screening of high-grade blunt solid organ injuries with delayed abdominal CTA to avoid missing PSA.

Similar content being viewed by others
Data availability
In line with institutional policies, data, material, and/or code will not be made available.
References
Bukur M, Inaba K, Barmparas G, Paquet C, Best C, Lam L, Plurad D, Demetriades D. Routine follow-up imaging of kidney injuries may not be justified. J Trauma. 2011;70(5):1229–33.
Zarzaur BL, Kozar RA, Fabian TC, Coimbra R. A survey of American Association for the Surgery of Trauma member practices in the management of blunt splenic injury. J Trauma. 2011;70(5):1026–31.
Wallen TE, Clark K, Baucom MR, Pabst R, Lemmink J, Pritts TA, Makley AT, Goodman MD. Delayed splenic pseudoaneurysm identification with surveillance imaging. J Trauma Acute Care Surg. 2022;93(1):113–7.
Morrison CA, Gross BW, Kauffman M, Rittenhouse KJ, Rogers FB. Overview of nonoperative blunt splenic injury management with associated splenic artery pseudoaneurysm. Am Surg. 2017;83(6):554–8.
Leeper WR, Leeper TJ, Ouellette D, Moffat B, Sivakumaran T, Charyk-Stewart T, Kribs S, Parry NG, Gray DK. Delayed hemorrhagic complications in the nonoperative management of blunt splenic trauma: early screening leads to a decrease in failure rate. J Trauma Acute Care Surg. 2014;76(6):1349–53.
Østerballe L, Helgstrand F, Axelsen T, Hillingsø J, Svendsen LB. Hepatic pseudoaneurysm after traumatic liver injury; is CT follow-up warranted? J Trauma Manag Outcomes. 2014;8:18.
Muroya T, Ogura H, Shimizu K, Tasaki O, Kuwagata Y, Fuse T, Nakamori Y, Ito Y, Hino H, Shimazu T. Delayed formation of splenic pseudoaneurysm following nonoperative management in blunt splenic injury: multi-institutional study in Osaka. Japan. J Trauma Acute Care Surg. 2013;75(3):417–20.
Zarzaur BL, Dunn JA, Leininger B, Lauerman M, Shanmuganathan K, Kaups K, Zamary K, Hartwell JL, Bhakta A, Myers J, et al. Natural history of splenic vascular abnormalities after blunt injury: a Western Trauma Association multicenter trial. J Trauma Acute Care Surg. 2017;83(6):999–1005.
Kumari M, Parwez M, Jain A, Pandya B. Management of a delayed, post-traumatic rupture of splenic artery pseudoaneurysm in a patient with life threatening co-morbidities: a treatment challenge. Int J Surg Case Rep. 2020;75:479–82.
Sugg SL, Gerndt SJ, Hamilton BJ, Francis IR, Taheri PA, Rodriguez JL. Pseudoaneurysms of the intraparenchymal splenic artery after blunt abdominal trauma: a complication of nonoperative therapy and its management. J Trauma. 1995;39(3):593–5.
Davis KA, Fabian TC, Croce MA, Gavant ML, Flick PA, Minard G, Kudsk KA, Pritchard FE. Improved success in nonoperative management of blunt splenic injuries: embolization of splenic artery pseudoaneurysms. J Trauma. 1998;44(6):1008–15.
Inoue Y, Ikegawa H, Ukai I, Yoshiya K, Sumi Y, Ogura H, Kuwagata Y, Tanaka H, Shimazu T, Sugimoto H. Spontaneous occlusion of splenic and renal pseudoaneurysm after blunt abdominal trauma: a case report and literature review. J Emerg Med. 2010;38(3):e17-22.
Kagoura M, Monden K, Sadamori H, Hioki M, Ohno S, Takakura N. Outcomes and management of delayed complication after severe blunt liver injury. BMC Surg. 2022;22(1):241.
Funding
No funding was received for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Authors Schellenberg, Owattanapanich, Emigh, Nichols, Dilday, Ugarte, Onogawa, Matsushima, Martin, and Inaba declare that they have no conflict of interest.
Ethical approval
All procedures performed in this retrospective observational study involving human participants were in accordance with the ethical standards of the Institutional Review Board of the University of California (HS-22- 00050) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
This study received a waiver for informed consent by the Institutional Review Board of the University of Southern California (HS-22-00050).
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Schellenberg, M., Owattanapanich, N., Emigh, B. et al. Pseudoaneurysms after high-grade blunt solid organ injury and the utility of delayed computed tomography angiography. Eur J Trauma Emerg Surg 49, 1315–1320 (2023). https://doi.org/10.1007/s00068-022-02197-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-022-02197-2