Abstract
Purpose
Trauma during pregnancy is the leading indirect obstetric cause of death, and its management is challenging owing to its characteristics. We aimed to describe the epidemiology of pregnant trauma patients and explore their characteristics by comparing them with those of non-pregnant patients.
Methods
Using the Japan Trauma Data Bank data collected between January 2004 and May 2019, we identified pregnant and non-pregnant female trauma patients between the ages of 15–45 years. We described patient characteristics, prehospital information, in-hospital management, and clinical outcomes. We also investigated the differences in the information between pregnant and non-pregnant patients.
Results
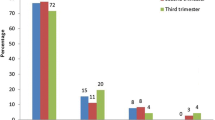
In total, 165 pregnant trauma patients were identified (0.7%). Motor vehicle collisions were the most frequent mechanism of injury (64.6%) in pregnant patients. The time from call to the arrival of emergency medical services at the hospital was similar for both pregnant and non-pregnant patients. The use of abdominal computed tomography (CT) scans was lower and injury to the abdomen was more frequent in pregnant than non-pregnant patients. In-hospital mortality was 7.2% in pregnant patients and 10.9% in non-pregnant patients. No significant differences in mortality after adjustment for confounding factors were found (adjusted odds ratio: 0.78, 95% confidential interval: 0.35–1.75, p = 0.548).
Conclusion
Transport time and mortality were similar between pregnant and non-pregnant trauma patients. Abdominal trauma and surgery were more common in pregnant relative to non-pregnant patients, while the number of CT scans was less. Further research is required to investigate the effects of trauma on the course of pregnancy and the fetus.

Similar content being viewed by others
Data Availability
The data that support the findings of this study are available from the JTDB, but the availability of these data is restricted.
References
WHO U, UNFPA, World Bank Group and the United Nations Population Division. World Health Organization. Maternal mortality: Levels and trends 2000–2017. https://www.who.int/reproductivehealth/publications/maternal-mortality-2000-2017/en/. Accessed 24 Aug 2021.
Say L, Chou D, Gemmill A, et al. Global causes of maternal death: a WHO systematic analysis. Lancet Glob Health. 2014;2:e323–33. https://doi.org/10.1016/s2214-109x(14)70227-x.
Fildes J, Reed L, Jones N, Martin M, Barrett J. Trauma: the leading cause of maternal death. J Trauma. 1992;32:643–5.
Petrone P, Talving P, Browder T, et al. Abdominal injuries in pregnancy: a 155-month study at two level 1 trauma centers. Injury. 2011;42:47–9. https://doi.org/10.1016/j.injury.2010.06.026.
El-Kady D, Gilbert WM, Anderson J, Danielsen B, Towner D, Smith LH. Trauma during pregnancy: an analysis of maternal and fetal outcomes in a large population. Am J Obstet Gynecol. 2004;190:1661–8. https://doi.org/10.1016/j.ajog.2004.02.051.
Sperry JL, Casey BM, McIntire DD, Minei JP, Gentilello LM, Shafi S. Long-term fetal outcomes in pregnant trauma patients. Am J Surg. 2006;192:715–21. https://doi.org/10.1016/j.amjsurg.2006.08.032.
Hill CC, Pickinpaugh J. Trauma and surgical emergencies in the obstetric patient. Surg Clin North Am. 2008;88:421–40. https://doi.org/10.1016/j.suc.2007.12.006.
Kuo C, Jamieson DJ, McPheeters ML, Meikle SF, Posner SF. Injury hospitalizations of pregnant women in the US, 2002. Am J Obstet Gynecol. 2007;196(161):e1-6. https://doi.org/10.1016/j.ajog.2006.09.015.
Battaloglu E, McDonnell D, Chu J, Lecky F, Porter K. Epidemiology and outcomes of pregnancy and obstetric complications in trauma in the United Kingdom. Injury. 2016;47:184–7. https://doi.org/10.1016/j.injury.2015.08.026.
Hitosugi M, Motozawa Y, Kido M, et al. Traffic injuries of the pregnant women and fetal or neonatal outcomes. Forensic Sci Int. 2006;159:51–4. https://doi.org/10.1016/j.forsciint.2005.06.006.
Research. JTCa. The Japan Trauma Data Bank. https://www.jtcr-jatec.org/traumabank/index.htm. Accessed 25 Aug 2021.
Research JTCa. Japan Trauma Data Bank Report 2020 (2019.1-2019.12). https://www.jtcr-jatec.org/traumabank/dataroom/data/JTDB2020e.pdf. Accessed 25 Aug 2021.
Harmsen AM, Giannakopoulos GF, Moerbeek PR, Jansma EP, Bonjer HJ, Bloemers FW. The influence of prehospital time on trauma patients outcome: a systematic review. Injury. 2015;46:602–9. https://doi.org/10.1016/j.injury.2015.01.008.
Ruffolo DC. Trauma care and managing the injured pregnant patient. J Obstet Gynecol Neonatal Nurs. 2009;38:704–14. https://doi.org/10.1111/j.1552-6909.2009.01072.x.
Jain V, Chari R, Maslovitz S, et al. Guidelines for the management of a pregnant trauma patient. J Obstet Gynaecol Can. 2015;37:553–74. https://doi.org/10.1016/s1701-2163(15)30232-2.
Maxwell BG, Greenlaw A, Smith WJ, Barbosa RR, Ropp KM, Lundeberg MR. Pregnant trauma patients may be at increased risk of mortality compared to nonpregnant women of reproductive age: trends and outcomes over 10 years at a level I trauma center. Womens Health (Lond). 2020;16:1745506520933021. https://doi.org/10.1177/1745506520933021.
Oba T, Hasegawa J, Sekizawa A. Postpartum ultrasound: postpartum assessment using ultrasonography. J Matern Fetal Neonatal Med. 2017;30:1726–9. https://doi.org/10.1080/14767058.2016.1223034.
Prick BW, Jansen AJ, Steegers EA, et al. Transfusion policy after severe postpartum haemorrhage: a randomised non-inferiority trial. BJOG. 2014;121:1005–14. https://doi.org/10.1111/1471-0528.12531.
Deshpande NA, Kucirka LM, Smith RN, Oxford CM. Pregnant trauma victims experience nearly 2-fold higher mortality compared to their nonpregnant counterparts. Am J Obstet Gynecol. 2017;217(590):e1-9. https://doi.org/10.1016/j.ajog.2017.08.004.
John PR, Shiozawa A, Haut ER, et al. An assessment of the impact of pregnancy on trauma mortality. Surgery. 2011;149(1):94–8. https://doi.org/10.1016/j.surg.2010.04.019.
Acknowledgements
We thank JTDB and all personnel at the participating institutions for their contributions. Furthermore, we would like to thank Editage (www.editage.com) for English language editing.
Funding
No funding was received for conducting this study.
Author information
Authors and Affiliations
Contributions
YM contributed to the conception and design of this study, data analysis, interpretation of results, and writing of the manuscript draft. TK contributed to the conception and design of this study, the interpretation of results, and the drafting of the manuscript. HK and SI supervised the study and interpreted the data. All authors agree to be accountable for all aspects of this research, ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Conflict of interest
All authors have no relevant financial or non-financial interests to declare.
Ethical approval
All procedures performed in this study follow the ethical standards of the participating institutes and the Japanese Association for the Surgery of Trauma and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Consent to participate
Not applicable.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Makino, Y., Kiguchi, T., Kato, H. et al. Epidemiology and outcomes of pregnant trauma patients in Japan: a nationwide descriptive study. Eur J Trauma Emerg Surg 49, 1287–1293 (2023). https://doi.org/10.1007/s00068-022-02165-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-022-02165-w