Abstract
Purpose
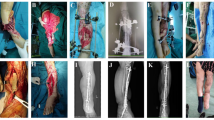
To investigate the clinical efficacy of accelerated rehabilitation surgery for the treatment of Gustilo type IIIA/B open tibiofibular fracture with emergency stage I debridement, internal fracture fixation, bone grafting, coverage of the wound surface with a muscle flap combined with vacuum sealing drainage (VSD), and internal and lateral leg reduction.
Methods
A retrospective analysis was performed on the clinical data of 15 patients with Gustilo type IIIA/B open tibiofibular fracture who were admitted to the Affiliated Zhongshan Hospital of Dalian University from January 2015 to December 2018. There were 12 males and 3 females. The patients ranged in age from 20 to 62 years, with an average of 39.5 years. After admission, the patients underwent stage I emergency debridement (including exploration and repair of nerves and tendons), open reduction and internal fixation of the tibia and fibula, iliac bone grafting, muscle flap and VSD coverage of the bone defect, complete tensioning of the calf inside and outside, tibia-sparing incision before healing, and stage II free skin grafting. Patients were followed up periodically to observe muscle flap survival, fracture healing time, length of hospitalization, wound healing time, delayed union, bone nonunion, osteomyelitis and other complications. At the last follow-up, the Johner–Wruhs criteria were used to evaluate the rate of good functional recovery from tibial shaft fracture, fracture healing quality was evaluated by the Merchant score, and limb function was evaluated by the LEFS.
Results
All 15 cases were followed up for 12–32 months, with an average of 22.8 months. All the fractures healed; the range of healing time was 14–30 weeks (mean 18.5 weeks). The length of hospitalization was 25.1 ± 7.6 days, and wound healing took 12.2 ± 2.0 days. None of the patients had complications such as osteomyelitis infection. When the Johner–Wruhs evaluation criteria for functional recovery from tibial shaft fracture were applied at the last follow-up, the outcomes were as follows: excellent in 13 cases, good in 1 case and fair in 1 case, for an excellent and good rate of 93.3%. When fracture healing was evaluated according to the Merchant scoring standard, the outcomes were as follows: excellent in 12 cases, good in 1 case, fair in 1 case, and poor in 1 case, for an excellent and good rate of 86.7%. The mean LEFS score of the affected limb at the last follow-up was 70 (59–80).
Conclusion
For Gustilo type IIIA/B open tibiofibular fractures, emergency stage I debridement, internal fixation of the fracture, bone grafting, coverage of the wound with a muscle flap, complete tensioning of the calf inside and outside, and application of VSD can improve the repair of leg soft-tissue defects, shorten hospitalization time, promote fracture healing, and effectively reduce infection and complications related to bone exposure. More importantly, this treatment protocol provides effective wound repair, guarantees the recovery of limb function, significantly speeds up recovery, and improve patients’ quality of life.





Similar content being viewed by others
Data availability
The datasets generated or analyzed during this study are available from the corresponding author on reasonable request.
References
Rittstieg P, Wurm M, Miiller M, et al. Current treatment strategies for lower leg fractures in adults. Unfallchirurg. 2020;123(6):479–90. https://doi.org/10.1007/s00113-020-00805-7.
Ljungqvist O, Scott M, Fearon KC. Enhanced recovery after surgery: a review. JAMA Surg. 2017;152(3):292–8.
Johner R, Wruhs O. classification of tibial shaft fractures andcorrelation with resuIts after rigid internal fixation. ClinOrthop. 1983;178:7–25.
Merchant TC, Dietz FR. Long-term follow-up after fractures of the tibial and fibular shafts. J Bone Jt Surg Am. 1989;71(4):599–606.
Javdan M, Tahririan MA, Nouri M. The role of fibular fixation in the treatment of combined distal tibia and fibula fracture: a randomized, control trial. Adv Biomed Res. 2017;6(1):48. https://doi.org/10.4103/2277-9175.205190.
Shafiq B, Hacquebord J, Wright DJ, et al. Modern princi-ples inthe acute surgical management of open distal tibial fractures. J Am Acad Orthop Surg. 2021;29(11):e536–47. https://doi.org/10.5435/JAAOS-D-20-00502.
Bliven EK, Greinwald M, Hackl S, et al. External fixation of the lower extremities: biomechanical perspective and recent innovations. Injury. 2019;50(Suppl 1):S10–7. https://doi.org/10.1016/j.injury.2019.03.041.
Mundi R, Chaudhry H, Niroopan G, et al. Open tibial fractures: updated guidelines for management. JBJS Rev. 2015. https://doi.org/10.2016/JBJS.RVW.N.00051.
Fu Q, Zhu L, Lu JJ, et al. External fixation versus unreamed tibial intramedullary nailing for open tibial fractures: a meta-analysis of randomized controlled trials. Sci Rep. 2018;8(1):1–7.
Riechelmann F, Kaiser P, Arora R. Primary softtissue management in open fracture. Oper Orthop Traumatol. 2018;30(5):294–308. https://doi.org/10.1007/s00064-018-0562-8.
Al-Hourani K, Fowler T, Whitehouse MR, et al. Two-stage combined ortho-plastic management of type IIIB open diaphyseal tibial fractures requiring flap coverage: is the timing of debridement and coverage associated with outcomes? J Orthop Trauma. 2019;33(12):591–7. https://doi.org/10.1097/BOT.0000000000001562.
Yu Bin Wu, Xinbao TP, et al. Chinese Guidelines for the diagnosis and treatment of open fractures (2019 edition). Chin J Trauma Orthoped. 2019;21(11):921–8. https://doi.org/10.3760/cma.j.issn.1671-7600.2019.11.001.
Wang Z, Liu T, Cheng Y, et al. Tibial nail combined with vacuum sealing drainage for Gustilo grade IIIB open tibialfractures:a patient series. J Foot Ankle Surg. 2020;59(2):409–12. https://doi.org/10.1053/j.jfas.201908.016.
Rupp M, Popp D, Alt V. Prevention of infection in open fractures: where are the pendulums now? Injury. 2019. https://doi.org/10.1016/j.injury.2019.10.074.
Al-Hourani K, Pearce O, Kelly M. Standards of open lower limb fracture care in the United Kingdom. Injury. 2021;52(3):378–83. https://doi.org/10.1016/j.injury.2021.01.021.
Kehlet H, Joshi GP. Enhanced recovery after surgery: current controversies and concerns. Anesth Analg. 2017;125(6):2154–5.
Boriani F, UlHaq A, Baldini T, Urso R, Granchi D, Baldini N, Tigani D, Tarar M, Khan U. Orthoplastic surgical collaboration is required to optimise the treatment of severe limb injuries: a multi-centre, prospective cohort study. J Plast Reconstr Aesth Surg. 2017;70(6):715–22.
Kuripla C, Tornetta P, Foote CJ, et al. Timing of flap coverage with respect to definitive fixation in open tibia fractures. J Orthop Trauma. 2021;35(8):430–6. https://doi.org/10.1097/BOT.0000000000002033.
Yazar S, Lin CH. One-stage reconstruction of composite bone and soft-tissue defects in traumatic lower extremities. Plast Reconstr Surg. 2004;114(6):1457–66.
Lack WD, Karunakar MA, Angerame MR, Seymour RB, Sims S, Kellam JF. Bosse MJ Type III open tibia fractures immediate antibiotic prophylaxis minimizes infection. J Orthop Trauma. 2015;29:1–6.
Nambi GI, Salunke AA, Thirumalaisamy SG, Babu VL, Baskaran K, Janarthanan T, Boopathi K, Chen YS. Single stage management of Gustilo type III A/B tibia fractures: fifixed with nail and covered with fascio cutaneous fl flap. Chin J Traumatol. 2017;20(2):99–102.
Gill SP, Raj M, Kumar S, Singh P, Kumar D, Singh J, Deep A. Early conversion of external fifixation to interlocked nailing in open fractures of both bone leg assisted with vacuum closure (VAC)-fifinal outcome. J Clin Diagn Res. 2016;10(2):RC10-4.
Nowotarski PJ, Turen CH, Brumback RJ, Scarboro JM. Conversion of external fifixation to intramedullary nailing for fractures of the shaft of the femur in multiply injured patients. J Bone Jt Surg Am. 2000;82(6):781–8.
Wilmore DW. From Cuthbertson to fast-track surgery: 70 years of progress in reducing stress in surgical patients. Ann Surg. 2002;236:643–8.
Poznanovic MR, Sulen N. Crush syndrome in severe tuaum. Lijec Vjesn. 2007;129(Suppl 5):142–4.
Egol KA, Bazzi J, McLaurin TM, et al. The effect of knee-spanning external fixation on compartment pressures in theleg. J Orthop Trauma. 2008;22(10):680–5.
DeLong WG Jr, Born CT, Wei SY, et al. Aggressive treatment of 119 open fracture wounds. J Trauma. 1999;46:1049–54.
Mathews JA, Ward J, Champman TW, Khan UM. Kelly MBSingle-stage orthoplastic reconstruction of Gustilo-Andersongrade III open tibial fractures greatly reduces infection rates. Injury. 2015;46:2263–6.
Funding
No funding was obtained from any source.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors unanimously declare that there is no conflict of interest.
Ethical approval
All procedures performed in this study involving human participants were in accordance with the ethical standards of the institutional and national research committees and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ma, X., Wang, Z. & Wang, J. Clinical analysis of accelerated rehabilitation surgery for Gustilo type IIIA/B open tibio fibular fracture. Eur J Trauma Emerg Surg 49, 2355–2362 (2023). https://doi.org/10.1007/s00068-022-02164-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-022-02164-x