Abstract
Purpose
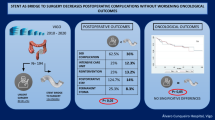
To analyze if perioperative and oncologic outcomes with stenting as a bridge to surgery (SEMS-BS) and interval colectomy performed by acute care surgeons for left-sided occlusive colonic neoplasms (LSCON) are non-inferior to those obtained by colorectal surgeons for non-occlusive tumors of the same location in the full-elective context.
Methods
From January 2011 to January 2021, patients with LSCON at University Regional Hospital in Málaga (Spain) were directed to a SEMS-BS strategy with an interval colectomy performed by acute care surgeons and included in the study group (SEMS-BS). The control group was formed with patients from the Colorectal Division elective surgical activity dataset, matching by ASA, stage, location and year of surgery on a ratio 1:2. Stages IV or palliative stenting were excluded. Software SPSS 23.0 was used to analyze perioperative and oncologic (defined by overall -OS- and disease free -DFS-survival) outcomes.
Results
SEMS-BS and control group included 56 and 98 patients, respectively. In SEMS-BS group, rates of technical/clinical failure and perforation were 5.35% (3/56), 3.57% (2/56) and 3.57% (2/56). Surgery was performed with a median interval time of 11 days (9–16). No differences between groups were observed in perioperative outcomes (laparoscopic approach, primary anastomosis rate, morbidity or mortality). As well, no statistically significant differences were observed in OS and DFS between groups, both compared globally (OS:p < 0.94; DFS:p < 0.67, respectively) or by stages I–II (OS:p < 0.78; DFS:p < 0.17) and III (OS:p < 0.86; DFS:p < 0.70).
Conclusion
Perioperative and oncologic outcomes of a strategy with SEMS-BS for LSCON are non-inferior to those obtained in the elective setting for non-occlusive neoplasms in the same location. Technical and oncologic safety of interval colectomy performed on a semi-scheduled situation by acute care surgeons is absolutely warranted.


Similar content being viewed by others
Abbreviations
- CRC:
-
Colorectal cancer
- LSCON:
-
Left-sided colonic occlusive neoplasms
- SEMS:
-
Self-expandable metallic stent
- ES:
-
Emergency surgery
- RCT:
-
Randomized controlled trials
- MA:
-
Meta-analysis
- ACS:
-
Acute care surgery
- CT:
-
Computed tomography
- SEMS-BS:
-
Self-expandable metallic stent as a bridge to surgery
- CRS:
-
Colorectal surgical activity database
- OS:
-
Overall survival
- DFS:
-
Disease-free survival
References
2017 WSES guidelines on colon and rectal cancer emergencies: obstruction and perforation. Pisano M, Zorcolo L, Merli C, Cimbanassi S, Poiasina E, Ceresoli M, et al. World J Em Surg. 2018. p. 36.
Arezzo A, Balague C, Targarona E, Borgui F, Giraudo G, Ghezzo L, et al. Colonic stenting as a bridge to surgery versus emergency surgery for malignant colonic obstruction: results of a multicenter randomized controlled trial (ESCO trial). Surg Endos. 2017;31(8):3297–305.
Alcántara M, Serra Aracil X, Falcó J, Mora L, Bombardó J, Navarro S. Prospective, controlled, randomized study in intraoperative colonic lavage versus stent placement in obstructive left-sided colonic cancer. World J Surg. 2011;35:1904–10.
Ghazal AHA, ElShazly WG, Bessa SS, ElRiwini MT, Hussein AM. Colonic endolumenal stenting devices and elective surgery versus emergency subtotal/total colectomy in the management of malignant obstructed left colon carcinoma. J Gastrointest Surg. 2013;17(6):1123–9.
Maruthachalam K, Lash GE, Shenton BK, et al. Tumour cell dissemination following endoscopic stent insertion. Br J Surg. 2007;94:1151–4.
Elwan TH, Zaher NA. Endoscopic stenting as a bridge to elective surgery versus emergency laparotomy for patients with acute malignant large bowel obstruction. Egypt J Surg. 2020;39:529–35.
Arezzo A, Forcignanò E, Bonino MA, Balagué C, Targarona E, Borgui F, Giraudo G, et al. Long-term oncologic results after stenting as a bridge to surgery versus emergency surgery for malignant left-sided colonic obstruction: a multicenter randomized controlled trial (ESCO trial). Ann Surg. 2020;272:703–8.
Cirocchi R, Arezzo A, Sapienza P, Crocetti D, Cavaliere D, Solaini L, et al. Current status of the self-expandable metal stent as a bridge to surgery versus emergency surgery in colorectal cancer: results from an updated systematic review and meta-analysis of the literature. Medicina. 2021;57:268.
van Hooft JE, Veld JV, Arnold D, Beets-Tan RGH, Everett S, Götz M, et al. Self-expandable metal stents for obstructing colonic and extracolonic cancer: European Society of Gastrointestinal Endoscopy (ESGE) Guideline-Update 2020. Endoscopy. 2020;52:389–407.
Kim SJ, Hur H, Min BS, Sohn SK, Cho CH, Kim NK. Oncologic outcomes of self-expanding metallic stent insertion as a bridge to surgery in the management of left-sided colon cancer obstruction: comparison with nonobstructing elective surgery. World J Surg. 2009;33:1281–6.
Knight AL, Trompetas V, Saunders MP, Anderson HJ. Does stenting of left-sided colorectal cancer as a bridge to surgery adversely affect oncological outcomes? A comparison with non-obstructing elective left-sided colonic resections. Int J Colorectal Dis. 2012;27(11):1509–14.
Tamini N, Ceresoli M, Aldè S, Carissimi F, Ripamonti L, Nespoli L, et al. Quasi-elective left colectomy after endoscopic colon stenting for obstructive cancer yields comparable oncologic outcome to full-elective operation. Int J Colorectal Dis. 2020;35:633–40.
Hallam S, Bickley M, Phelan L, Dilworth M, Bowley DM. Does declared surgeon specialist interest influence the outcome of emergency laparotomy? Ann R Coll Surg Engl. 2020;102(6):437–41.
Schuster KM, McGillicuddy EA, Maung AA, Kaplan LJ, Davis KA. Can acute care surgeons perform emergency colorectal procedures with good outcomes? J Trauma. 2011;71:94–101.
Gibbons GG, Jin-Tan C, Bartolo DCC, Filgate R, Makin G, Barwood N, Wallace M. Emergency left colonic resections on an acute surgical unit: does subspecialization improve outcomes? ANZ J Surg. 2015;85:739–43.
Kulaylat AS, Pappou E, Philip MM, Kuritzkes BA, Ortenzi G, Hollenbeak CS, Choi C, Messaris E. Emergent colon resections: does surgeon specialization influence outcomes? Dis Colon Rectum. 2019;62:79–87.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336patients and results of a survey. Ann Surg. 2004;240(2):205–13.
Di Saverio S, Birindelli A, Segalini E, Novello M, Larocca A, Ferrara F, Binda GA, Bassi M. “To stent or not to stent?”: immediate emergency surgery with laparoscopic radical colectomy with CME and primary anastomosis is feasible for obstructing left colon carcinoma. Surg Endosc. 2018;32(4):2151–5. https://doi.org/10.1007/s00464-017-5763-y (Epub 2017 Aug 8).
Tejero E, Mainar A, Fernández L, Tobio R, De Gregorio MA. New procedure for the treatment of colorectal neoplastic obstructions. Dis Colon Rectum. 1994;37(11):1158–9.
Yamashita S, Tanemura M, Sawada G, Moon J, Shimizu Y, Yamaguchi T, Kuwai T, Urata Y, Kuraoka K, Hatanaka N, Yamashita Y, Taniyama K. Impact of endoscopic stent insertion on detection of viable circulating tumor cells from obstructive colorectal cancer. Oncol Lett. 2018;15(1):400–6. https://doi.org/10.3892/ol.2017.7339 (Epub 2017 Nov 2).
Hill J, Clive K, Morton D, Magill L, Handley K, Gray RG. CREST: randomized phase III study of stenting as a bridge to surgery in obstructing colorectal cancer: results of the UK ColoRectal Endoscopic Stenting Trial (CREST). J Clin Oncol. 2016;34(15):3507.
Arezzo A, Passera R, Lo Secco G, Verra M, Bonino MA, Targarona E, Morino M. Stent as bridge to surgery for left-sided malignant colonic obstruction reduces adverse events and stoma rate compared with emergency surgery: results of a systematic review and meta-analysis of randomized controlled trials. Gastrointest Endosc. 2017;86:416–26.
Matsuda A, Miyashira M, Matsumoto S, Matsutani T, Sakurazawa N, Takahashi G, Kishi T, Uchida E. Comparison of long-term outcomes of colonic stent as bridge to surgery and emergency surgery for malignant large bowel obstruction: a meta-analysis. Ann Surg Oncol. 2015;22(2):497–504.
Huang X, Lu B, Zhang S, Meng L. Preoperative colonic stents versus emergency surgery for acute left-sided malignant colonic obstruction: a meta-analysis. J Gastrointest Surg. 2014;18(3):584–91.
Neo VSQ, Jain SR, Yeo JW, Ng CH, Gan TRX, Tan E, Chong CS. Controversies of colonic stenting in obstructive left colorectal cáncer: a critical analysis with meta-analysis and meta-regression. Int J Colorectal Dis. 2021;36(4):689–700.
Jain SR, Yaow CYL, Ng CH, Neo VSQ, Lim F, Foo FJ, Wong NW, Chong CS. Comparison of colonic stents, stomas and resection for obstructive left colon cancer: a meta-analysis. Tech Coloproctol. 2020;24(11):1121–36. https://doi.org/10.1007/s10151-020-02296-5 (Epub 2020 Jul 17).
Arezzo A, Passera R, Lo Secco G, Verra M, Bonino MA, Targarona E, Morino M. Stent as bridge to surgery for left-sided malignant colonic obstruction reduces adverse events and stoma rate compared with emergency surgery: results of a systematic review and meta-analysis of randomized controlled trials. Gastrointest Endosc. 2017;86(3):416–26. https://doi.org/10.1016/j.gie.2017.03.1542 (Epub 2017 Apr 6).
Amelung FJ, Burghgraef TA, Tanis PJ, van Hooft JE, Ter Borg F, Siersema PD, Bemelman WA, Consten ECJ. Critical appraisal of oncological safety of stent as bridge to surgery in left-sided obstructing colon cancer; a systematic review and meta-analysis. Crit Rev Oncol Hematol. 2018;131:66–75. https://doi.org/10.1016/j.critrevonc.2018.08.003 (Epub 2018 Sep 4).
Benson AB, Venook AP, Al-Hawary MM, Arain MA, Chen YJ, Ciombor KK, et al. NCCN clinical practice guidelines in oncology (NCCN Guidelines). Colon cancer. Version 2.2021. 3025 Chemical Road, Suite 100, Plymouth Meeting, PA 19462: NCCN; c2021. https://www.nccn.org/professionals/physician_gls/pdf/colon.pdf. Accessed 18 May 2021.
Van Hooft JE, van Halsema EE, Vanbiervliet G, Beets-Tan RGH, DeWitt JM, Donnellan F, et al. Self-expandable metal stents for obstructing colonic and extracolonic cancer: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline. Endoscopy. 2014;46(11):990–1053.
Sloothaak DAM, van Berg MW, Dijkgraaf MGW, Fockens P, Tanis PJ, van Hooft JE, Bemelman WA. Collaborative Dutch Stent-In study group oncological outcome of malignant colonic obstruction in the Dutch Stent-In 2 trial. Br J Surg. 2014;101(13):1751–7.
Committee on Acute Care Surgery American Association for the Surgery of Trauma. The acute care surgery curriculum. J Trauma. 200;62(3):553–6. https://doi.org/10.1097/TA.0b013e3180327c18
Ingraham A, Nathens A, Peitzman A, Bode A, Dorlac G, Dorlac W, Miller P, Sadeghi M, Wasserman DD, Bilimoria K. American association for the surgery of trauma emergency general surgery quality indicator development expert panel assessment of emergency general surgery care based on formally developed quality indicators. Surgery. 2017. https://doi.org/10.1016/j.surg.2017.03.025 (Epub 2017 Jun 21).
Aranda Narváez JM, Tallón Aguilar L, López Ruiz JA, Pareja Ciuró F, Jover Navalón JM, Turégano Fuentes F, Navarro Soto S, Ceballos Esparragón J, Pérez Díaz L. The acute care surgery model in the world, and the need for and implementation of trauma and emergency surgery units in Spain. Cir Esp. 2019;97(1):3–10. https://doi.org/10.1016/j.ciresp.2018.09.015.
National Accreditation Program for Trauma and Emergency Surgery Units. Calle O´Donnell, 16. 1º izq., 28009 Madrid, Spain: Spanish Association of Surgeons; c2021. https://www.aecirujanos.es/Trauma-y-Cirugia-de-Urgencias_es_80_0_0_384_386.html. Accessed 18 May 2021.
Archampong D, Borowski D, Wille-Jørgensen P, Iversen LH. Workload and surgeon’s specialty for outcome after colorectal cancer surgery. Cochrane Database Syst Rev. 2012. https://doi.org/10.1002/14651858.CD005391.pub3.
De la Portilla F, Builes S, García-Novoa A, Espín E, Kreisler E, Enríquez-Navascues JM, Biondo S, Codina A. Analysis of quality indicators for colorectal cáncer surgery in units accredited by the Spanish Association of Coloproctology. Cir Esp. 2018;96(4):226–33.
Acknowledgements
To Dr. Di Saverio S. for previous exam of the paper, and so appreciable help with structure and language.
Funding
No funding was obtained to develop the present study.
Author information
Authors and Affiliations
Contributions
AJM and GJ played the same role in designing the study, collecting/analyzing data and writing the manuscript. AJM, GAJ, TA, CI and RL performed colectomies in the study group and gave significant support to the final version of the manuscript. GI and MS operated patients of the control group and formulated adequate suggestions to analysis and writing. VL performed the endoscopic stent placement in most of the patients of study group and contributed with data regarding the procedure. SJ gave institutional support and key suggestions to the study and the manuscript. All authors have examined and approved the final version of this paper.
Corresponding author
Ethics declarations
Conflict of interests
The authors declare that they have no competing interests.
Ethics approval and consent to participate
The current study has received the approval of the Ethics for Investigation Committee of the province of Málaga, Spain (graphic confirmation available). No specific informed consent was considered necessary, though all patients signed the necessary consent for surgery.
Consent for publication
Not applicable.
Rights and permissions
About this article
Cite this article
Aranda-Narváez, J., González-Cano, J., González-Sánchez, A. et al. Perioperative and oncologic outcomes of interval colectomy performed by acute care surgeons after stenting as a bridge to surgery for left-sided malignant colonic obstruction are non-inferior to the outcomes of colorectal surgeons in the elective setting: single center experience. Eur J Trauma Emerg Surg 48, 4651–4660 (2022). https://doi.org/10.1007/s00068-022-02015-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-022-02015-9