Abstract
Purpose
Severe sepsis and septic shock may impair microcirculatory perfusion and cause organ dysfunction. The aim of this pilot study was to assess a new microcirculation-guided resuscitation strategy in patients with septic shock undergoing emergency abdominal surgery.
Methods
A microcirculation-guided treatment algorithm was developed and applied intraoperatively following restoration of systemic hemodynamics. Sublingual microcirculation was monitored with Sidestream DarkField (SDF +) imaging technique. The primary objective was to investigate the change in De Backer score, Consensus Proportion of Perfused Vessels (Consensus PPV), and Consensus PPV (small) and its association with venous-to-arterial carbon dioxide difference (v-aPCO2).
Results
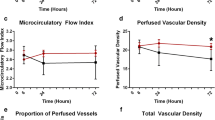
Thirteen consecutive patients were included in the study. Microcirculation-guided resuscitation resulted in an increase of 0.49 mm−1 in the De Backer score (p < 0.001), an increase of 2.28% in the Consensus PPV (p < 0.001), and an increase of 2.26% in the Consensus PPV (small) (p < 0.001) for every 30 min of additional intraoperative time. All microcirculation variables were negatively correlated with v-aPCO2 (rho = − 0.656, adj-p < 0.001; rho = − 0.623; adj-p < 0.001; rho = − 0.597, adj-p < 0.001, respectively) at each intraoperative time point. Lactate levels were negatively correlated with Consensus PPV (rho = − 0.464; adj-p = 0.002) and Consensus PPV (small) (rho = − 0.391, adj-p < 0.001). Survival at 30 days, 90 days, and 1 year were 76.9%, 76.9%, and 61.5%, respectively.
Conclusions
The intraoperative use of microcirculation-guided resuscitation strategy may improve tissue perfusion and hemodynamic coherence in patients with septic shock.




Similar content being viewed by others
Data availability
Data can be made available upon request after publication through a collaborative process. Researchers should provide a methodically sound proposal with specific objectives in an approval proposal. Please contact the corresponding author for additional information.
References
Wolsted H, Møller AM, Tolstrup MB, Vester-Andersen M. A description of deaths following emergency abdominal surgery. World J Surg. 2017;41:3105–10.
Ince C. Hemodynamic coherence and the rationale for monitoring the microcirculation. Crit Care. 2015;19(Suppl 3):S8.
Dubin A, Kanoore Edul VS, Caminos Eguillor JF, Ferrara G. Monitoring microcirculation: utility and barriers—a point-of-view review. Vasc Health Risk Manag. 2020;16:577–89.
Chalkias A, Laou E, Kolonia K, Ragias D, Angelopoulou Z, Mitsiouli E, Kallemose T, Smith-Hansen L, Eugen-Olsen J, Arnaoutoglou E. Elevated preoperative suPAR is a strong and independent risk marker for postoperative complications in patients undergoing major noncardiac surgery (SPARSE). Surgery. 2021. https://doi.org/10.1016/j.surg.2021.10.012.
De Backer D, Hollenberg S, Boerma C, Goedhart P, Büchele G, Ospina-Tascon G, Dobbe I, Ince C. How to evaluate the microcirculation: report of a round table conference. Crit Care. 2007;11:R101.
Massey MJ, Shapiro NI. A guide to human in vivo microcirculatory flow image analysis. Crit Care. 2016;20:35.
Rhodes A, Evans LE, Alhazzani W, Levy MM, Antonelli M, Ferrer R, Kumar A, Sevransky JE, Sprung CL, Nunnally ME, Rochwerg B, Rubenfeld GD, Angus DC, Annane D, Beale RJ, Bellinghan GJ, Bernard GR, Chiche JD, Coopersmith C, De Backer DP, French CJ, Fujishima S, Gerlach H, Hidalgo JL, Hollenberg SM, Jones AE, Karnad DR, Kleinpell RM, Koh Y, Lisboa TC, Machado FR, Marini JJ, Marshall JC, Mazuski JE, McIntyre LA, McLean AS, Mehta S, Moreno RP, Myburgh J, Navalesi P, Nishida O, Osborn TM, Perner A, Plunkett CM, Ranieri M, Schorr CA, Seckel MA, Seymour CW, Shieh L, Shukri KA, Simpson SQ, Singer M, Thompson BT, Townsend SR, Van der Poll T, Vincent JL, Wiersinga WJ, Zimmerman JL, Dellinger RP. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock: 2016. Intensive Care Med. 2017;43:304–77.
Özarslan NG, Ayhan B, Kanbak M, Çelebioğlu B, Demircin M, Ince C, Aypar Ü. Comparison of the effects of sevoflurane, isoflurane, and desflurane on microcirculation in coronary artery bypass graft surgery. J Cardiothorac Vasc Anesth. 2012;26:791–8.
Meijs LPB, van Houte J, Conjaerts BCM, Bindels AJGH, Bouwman A, Houterman S, Bakker J. Clinical validation of a computerized algorithm to determine mean systemic filling pressure. J Clin Monit Comput. 2022;36:191–8.
Wijnberge M, Sindhunata DP, Pinsky MR, Vlaar AP, Ouweneel E, Jansen JR, Veelo DP, Geerts BF. Estimating mean circulatory filling pressure in clinical practice: a systematic review comparing three bedside methods in the critically ill. Ann Intensive Care. 2018;8:73.
Massey MJ, Larochelle E, Najarro G, Karmacharla A, Arnold R, Trzeciak S, Angus DC, Shapiro NI. The microcirculation image quality score: development and preliminary evaluation of a proposed approach to grading quality of image acquisition for bedside videomicroscopy. J Crit Care. 2013;28:913–7.
Chalkias A, Spyropoulos V, Koutsovasilis A, Papalois A, Kouskouni E, Xanthos T. Cardiopulmonary arrest and resuscitation in severe sepsis and septic shock: a research model. Shock. 2015;43:285–91.
Chalkias A, Xanthos T, Papageorgiou E, Anania A, Beloukas A, Pavlopoulos F. Intraoperative initiation of a modified ARDSNet protocol increases survival of septic patients with severe acute respiratory distress syndrome. Heart Lung. 2018;47:616–21.
Bezemer R, Bartels SA, Bakker J, Ince C. Clinical review: Clinical imaging of the sublingual microcirculation in the critically ill–where do we stand? Crit Care. 2012;16:224.
Valeanu L, Bubenek-Turconi SI, Ginghina C, Balan C. Hemodynamic monitoring in sepsis-a conceptual framework of macro- and microcirculatory alterations. Diagnostics (Basel). 2021;11:1559.
Dilken O, Ergin B, Ince C. Assessment of sublingual microcirculation in critically ill patients: consensus and debate. Ann Transl Med. 2020;8:793.
Pan P, Su L, Liu D, Wang X. Microcirculation-guided protection strategy in hemodynamic therapy. Clin Hemorheol Microcirc. 2020;75:243–53.
Kanoore Edul VS, Ince C, Dubin A. What is microcirculatory shock? Curr Opin Crit Care. 2015;21:245–52.
Ospina-Tascón GA, Umaña M, Bermúdez WF, Bautista-Rincón DF, Valencia JD, Madriñán HJ, Hernandez G, Bruhn A, Arango-Dávila C, De Backer D. Can venous-to-arterial carbon dioxide differences reflect microcirculatory alterations in patients with septic shock? Intensive Care Med. 2016;42:211–21.
Luhr R, Cao Y, Söderquist B, Cajander S. Trends in sepsis mortality over time in randomised sepsis trials: a systematic literature review and meta-analysis of mortality in the control arm, 2002–2016. Crit Care. 2019;23:241.
Shankar-Hari M, Harrison DA, Rubenfeld GD, Rowan K. Epidemiology of sepsis and septic shock in critical care units: comparison between sepsis-2 and sepsis-3 populations using a national critical care database. Br J Anaesth. 2017;119:626–36.
Shankar-Hari M, Phillips GS, Levy ML, Seymour CW, Liu VX, Deutschman CS, Angus DC, Rubenfeld GD, Singer M, Sepsis Definitions Task Force. Developing a new definition and assessing new clinical criteria for septic shock: for the third international consensus definitions for sepsis and septic shock (sepsis-3). JAMA. 2016;315:775–87.
Bauer M, Gerlach H, Vogelmann T, Preissing F, Stiefel J, Adam D. Mortality in sepsis and septic shock in Europe, North America and Australia between 2009 and 2019- results from a systematic review and meta-analysis. Crit Care. 2020;24:239.
Bouattour K, Teboul JL, Varin L, Vicaut E, Duranteau J. Preload dependence is associated with reduced sublingual microcirculation during major abdominal surgery. Anesthesiology. 2019;130:541–9.
Booth G, Stalker TJ, Lefer AM, Scalia R. Elevated ambient glucose induces acute inflammatory events in the microvasculature: effects of insulin. Am J Physiol Endocrinol Metab. 2001;280:E848–56.
Efrati S, Berman S, Hamad RA, Siman-Tov Y, Chanimov M, Weissgarten J. Hyperglycaemia emerging during general anaesthesia induces rat acute kidney injury via impaired microcirculation, augmented apoptosis and inhibited cell proliferation. Nephrology (Carlton). 2012;17:111–22.
Gomes MB, Affonso FS, Cailleaux S, Almeida AL, Pinto LF, Tibiriçá E. Glucose levels observed in daily clinical practice induce endothelial dysfunction in the rabbit macro- and microcirculation. Fundam Clin Pharmacol. 2004;18:339–46.
See KC. Glycemic targets in critically ill adults: a mini-review. World J Diabetes. 2021;12:1719–30.
De Backer D. Is microcirculatory assessment ready for regular use in clinical practice? Curr Opin Crit Care. 2019;25:280–4.
Turek Z, Sykora R, Matejovic M, Cerny V. Anesthesia and the microcirculation. Semin Cardiothorac Vasc Anesth. 2009;13:249–58.
Chalkias A, Papagiannakis N, Saugel B, Flick M, Kolonia K, Angelopoulou1 Z, Ragias D, Papaspyrou D, Bouzia A, Ntalarizou N, Stamoulis K, Kyriakaki A, Eugen-Olsen J, Laou E, Arnaoutoglou E. Association of preoperative plasma suPAR levels with intraoperative sublingual microvascular perfusion in patients undergoing major non-cardiac surgery. medRxiv. 2021. https://doi.org/10.1101/2021.07.03.21259960. Accessed 15 Jan 2021.
Chalkias A, Spyropoulos V, Georgiou G, Laou E, Koutsovasilis A, Pantazopoulos I, Kolonia K, Vrakas S, Papalois A, Demeridou S, Gourgoulianis K, Dontas I, Kaparos G, Baka S, Xanthos T. Baseline values and kinetics of IL-6, procalcitonin, and TNF-α in landrace-large white swine anesthetized with propofol-based total intravenous anesthesia. Biomed Res Int. 2021;2021:6672573.
Acknowledgements
This research was partially supported by the Hellenic Society of Cardiopulmonary Resuscitation. The authors would like to thank the medical and nursing stuff of the Department of Anesthesiology, University Hospital of Larisa, Greece, for their assistance during the study period. We are also thankful to Z. Hossain, medical software engineer at Microvision Medical (Amsterdam, The Netherlands), who provided technical expertise that greatly assisted the research.
Funding
None declared.
Author information
Authors and Affiliations
Contributions
Conceptualization: AC; methodology: AC; investigation: AC, EL, SK, GG, VA, and AK; data curation: AC, EL, MM, AM, NN, GC, and AK; formal analysis: NP; writing—original draft preparation: AC; writing—review and editing: AC, EL, MM, AM, NN, SK, GC, GG, VA, AK, and NP; visualization: AC, EL, and NP; supervision: AC; project administration: AC.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Supplementary Information
Below is the link to the electronic supplementary material.
68_2022_1991_MOESM4_ESM.tiff
Supplementary file4 Supplementary Figure 4: Correlation between glucose levels and microcirculation variables. (TIFF 169 KB)
68_2022_1991_MOESM6_ESM.tiff
Supplementary file6 Supplementary Figure 6: Correlation of microcirculation variables with PGVR, RVR, and Eh. (TIFF 405 KB)
68_2022_1991_MOESM8_ESM.tiff
Supplementary file8 Supplementary Figure 8: Variation of macrocirculatory and microcirculation variables during the intraoperative period. (TIFF 352 KB)
Rights and permissions
About this article
Cite this article
Chalkias, A., Laou, E., Mermiri, M. et al. Microcirculation-guided treatment improves tissue perfusion and hemodynamic coherence in surgical patients with septic shock. Eur J Trauma Emerg Surg 48, 4699–4711 (2022). https://doi.org/10.1007/s00068-022-01991-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-022-01991-2