Abstract
Purpose
Chest tube insertion requires interdisciplinary teamwork including an emergency surgeon or physician in conjunction with a nurse. The purpose of the study was to validate an interdisciplinary performance assessment scale for chest tube insertion developed from literature analysis.
Methods
This prospective study took place in the simulation center of the University of Paris. The participants included untrained emergency/intensivist residents and trained novice emergency/intensivist physicians with less than 2 years of clinical experience and 6 months following training in thoracostomy, and nursing students. Each interdisciplinary pair participated in a high-fidelity simulation session. Two independent observers (O1 and O2) evaluated 61 items. Internal coherence using the Cronbach’s α coefficient, intraclass correlation coefficient (ICC), and correlation of scores by regression analysis (R2) were analyzed. Comparison between O1 and O2 mean scores used a t test and F test for SDs. p Value < 0.05 was significant.
Results
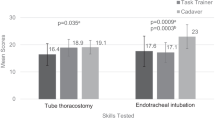
From an initial selection of 11,277 articles, 19 were selected to create the initial scale. The final scale comprises 61 items scored out of 80, including 24 items for nursing items, 24 items for medical competence, and 13 mixed items for the competence of both. 40 simulations including 80 participants were evaluated. Cronbach’s α = 0.76, ICC = 0.92, R2 = 0.88. There was no difference between the observers’ assessments of means (p = 0.82) and SDs (p = 0.92). Score was 51.6 ± 5.9 in the group of untrained residents and nursing student, and 57.2 ± 2.8 in the trained group of novice physicians and nursing students (p = 0.0003).
Conclusions
This first performance assessment scale for interdisciplinary chest tube insertion is valid and reliable.

Similar content being viewed by others
Availability of data and materials
All data analyzed during this study are included in the manuscript and supplemental files. Materials described in the manuscript, including all relevant raw data, are freely available to any scientist wishing to use them for non-commercial purposes, without breaching participant confidentiality. For more details, please contact the corresponding author.
References
Baru A, Weldegiorgis E, Zewdu T, Hussien H. Characteristics and outcome of traumatic chest injury patients visited a specialized hospital in Addis Ababa, Ethiopia: a one-year retrospective study. Chin J Traumatol. 2020;23(3):139–44. https://doi.org/10.1016/j.cjtee.2020.02.001.
Kulshrestha P, Munshi I, Wait R. Profile of chest trauma in a level I trauma center. J Trauma. 2004;57(3):57681. https://doi.org/10.1097/01.ta.0000091107.00699.c7.
Bouzat P, Raux M, David JS, et al. Chest trauma: first 48 hours management. Anaesth Crit Care Pain Med. 2017;36(2):13545. https://doi.org/10.1016/j.accpm.2017.01.003.
Parlak M, Uil SM, van den Berg JWK. A prospective, randomised trial of pneumothorax therapy: manual aspiration versus conventional chest tube drainage. Respir Med. 2012;106(11):16005. https://doi.org/10.1016/j.rmed.2012.08.005.
Drinhaus H, Annecke T, Hinkelbein J. Chest decompression in emergency medicine and intensive care. Anaesthesist. 2016;65(10):768–75. https://doi.org/10.1007/s00101-016-0219-7.
Kong VY, Oosthuizen GV, Sartorius B, Keene C, Clarke DL. An audit of the complications of intercostal chest drain insertion in a high volume trauma service in South Africa. Ann R Coll Surg Engl. 2014;96(8):609–13. https://doi.org/10.1308/003588414X14055925058599.
Sethuraman KN, Duong D, Mehta S, et al. Complications of tube thoracostomy placement in the emergency department. J Emerg Med. 2011;40(1):1420. https://doi.org/10.1016/j.jemermed.2008.06.033.
Laws D, Neville E, Duffy J, Pleural Diseases Group, Standards of Care Committee, British Thoracic Society. BTS guidelines for the insertion of a chest drain. Thorax. 2003;58(Suppl 2):ii53–9. https://doi.org/10.1136/thorax.58.suppl_2.ii53.
Ghazali A, Breque C, Léger A, Scépi M, Oriot D. Testing of a complete training model for chest tube insertion in traumatic pneumothorax. Simul Healthc J. 2015;10(4):23944. https://doi.org/10.1097/SIH.0000000000000071.
Elsayed H, Roberts R, Emadi M, Whittle I, Shackcloth M. Chest drain insertion is not a harmless procedure—are we doing it safely? Interact Cardiovasc Thorac Surg. 2010;11(6):7458. https://doi.org/10.1510/icvts.2010.243196.
Ober J, Haubruck P, Nickel F, et al. Development and validation of an objective assessment scale for chest tube insertion under ‘direct’ and ‘indirect’ rating. BMC Med Educ. 2018. https://doi.org/10.1186/s12909-018-1430-9.
L’Hers E, Geeraerts T, Desclefs JP, et al. Recommandations de Pratiques Professionnelles SRLF, SFAR, SFMU, SOFRASIMS. Intérêts de l’apprentissage par simulation en soins critiques. 2019 [In French]. https://sfar.org/wp-content/uploads/2019/05/rfe-interets-de-lapprentissage-par-simulation-en-soins-critiques.pdf. Accessed 6 May 2021.
Léger A, Ghazali A, Petitpas F, Guéchi Y, Boureau-Voultoury A, Oriot D. Impact of simulation-based training in surgical chest tube insertion on a model of traumatic pneumothorax. Adv Simul Lond Engl. 2016;1:21. https://doi.org/10.1186/s41077-016-0021-2.
Chung TN, Kim SW, You JS, Chung HS. Tube thoracostomy training with a medical simulator is associated with faster, more successful performance of the procedure. Clin Exp Emerg Med. 2016;3(1):169. https://doi.org/10.15441/ceem.15.097.
Ghazali A, Leger A, Petitpas F, Guéchi Y, Boureau-Voultoury A, Oriot D. Development and validation of a performance assessment scale for chest tube insertion in traumatic pneumothorax. J Pulm Respir Med. 2016;6:3. https://doi.org/10.4172/2161-105X.1000346.
Tarhan M, Gökduman S, Ayan A. Nurses’ knowledge levels of chest drain management: a descriptive study. Eurasian J Pulmonol. 2016;18(3):153–9.
Labrague LJ, McEnroe-Petitte DM, Fronda DC, Obeidat AA. Interprofessional simulation in undergraduate nursing program: an integrative review. Nurse Educ Today. 2018;67(1):46–55. https://doi.org/10.1016/j.nedt.2018.05.001.
Downing SM. Validity: on meaningful interpretation of assessment data. Med Educ. 2003;37:830–7. https://doi.org/10.1046/j.1365-2923.2003.01594.x.
Ghazali A, Richard A, Chaudet A, Choquet C, Guericolas M, Casalino E. Profile and motivation of patients consulting in emergency departments while not requiring such a level of care. Int J Environ Res Public Health. 2019;16(22):4431. https://doi.org/10.3390/ijerph16224431.
Ghazali D, Ilha-Schuelter P, Barbosa S, et al. Interdisciplinary teamwork for chest tube insertion and management: an integrative review. Anaesthesiol Intensive Ther. 2021;53(5):456–65. https://doi.org/10.5114/ait.2021.111349.
Peterson RA. A meta-analysis of Cronbach’s coefficient alpha. J Consum Res. 1994;21(2):381–91.
Koo TK, Li MY. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med. 2016;15(2):155–63. https://doi.org/10.1016/j.jcm.2016.02.012.
Kesieme EB, Essu IS, Arekhandia BJ, Welcker K, Prisadov G. Nurses’ knowledge of care of chest drain: a survey in a Nigerian semiurban university hospital. Ann Afr Med. 2016;15(1):28–33. https://doi.org/10.4103/1596-3519.172556.
Reeves S, Pelone F, Harrison R, Goldman J, Zwarenstein M. Interprofessional collaboration to improve professional practice and healthcare outcomes. Cochrane Database Syst Rev. 2017;6(6):CD000072. https://doi.org/10.1002/14651858.CD000072.pub3.
Reeves S, Xyrichis A, Zwarenstein M. Teamwork, collaboration, coordination, and networking: why we need to distinguish between different types of interprofessional practice. J Interprof Care. 2018;32(1):1–3. https://doi.org/10.1080/13561820.2017.1400150.
Freixinet Gilart J, Ramírez Gil ME, Gallardo Valera G, Moreno Casado P. Traumatismos torácicos [Chest trauma]. Arch Bronconeumol. 2011;47(Suppl 3):9–14. https://doi.org/10.1016/S0300-2896(11)70023-0 (Spanish).
Durai R, Ng PCH. How to insert a perfect chest drain. Acta Chir Belg. 2009;109(5):6524. https://doi.org/10.1080/00015458.2009.11680510.
American College of surgeons (2018) Chapiter 4 Thoracic Trauma, Appendix G, skill station B, breathing: finger and tube thoracostomy. In: Advanced trauma life support, student course manual (10th edn). Chicago, pp 346–347
Acknowledgements
The authors would like to thank Jeffrey Arsham, an American medical translator, for having reviewed the English-language text.
Funding
None declared. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
Conceptualization: DAG: ideas; DAG, DO, and PP: formulation or evolution of overarching research goals and aims. Methodology: DAG: development or design of methodology; DAG and PIS: creation of models. Validation: DO, and PP: verification, whether as a part of the activity or separate, of the overall replication/reproducibility of results/experiments and other research outputs. Formal analysis: DAG: application of statistical, mathematical, computational, or other formal techniques to analyze or synthesize study data. Investigation: DAG: conducting a research and investigation process, specifically performing the experiments, or data/evidence collection. Resources: DO and PP: provision of study materials, reagents, materials, patients, laboratory samples, animals, instrumentation, computing resources, or other analysis tools. Data curation: PIS, LB, and SSB: management activities to annotate (produce metadata), scrub data and maintain research data (including software code, where it is necessary for interpreting the data itself) for initial use and later reuse. Writing—original draft: DAG, OS, and LB: preparation, creation and/or presentation of the published work, specifically writing the initial draft (including substantive translation). Writing—review and editing: DO, FSVT: preparation, creation, and/or presentation of the published work by those from the original research group, specifically critical review, commentary or revision—including pre- or postpublication stages. Supervision: FSVT and PP: oversight and leadership responsibility for the research activity planning and execution, including mentorship external to the core team. Project administration: DAG and PP: management and coordination responsibility for the research activity planning and execution.
Corresponding author
Ethics declarations
Conflict of interest
To the author’s knowledge, no conflict of interest, financial or other, exists.
Ethics approval
Research was performed in accordance with the Declaration of Helsinki. According to the French ethics law of the public health code (article R1121-1), ethical approval by the national ethical committee (CPP, Comité de Protection des Personnes) was not required for this educational and observational study. The study protocol was approved by the local committee on research and ethics (IRB number SL-DG-2020-5.1).
Consent to participate
Participants consented to participate, and “informed consent” was obtained from all subjects.
Consent for publication
Participants consented to the publication of de-identified data and individual details. The manuscript does not contain individual images or videos.
Publication statement
The manuscript has not been previously published and is not under consideration in the same or substantially similar form in any other journal.
Appendix 1: Interdisciplinary performance assessment scale in the chest tube insertion
Appendix 1: Interdisciplinary performance assessment scale in the chest tube insertion


Rights and permissions
About this article
Cite this article
Ghazali, D.A., Ilha-Schuelter, P., Barreyre, L. et al. Development and validation of the first performance assessment scale for interdisciplinary chest tube insertion: a prospective multicenter study. Eur J Trauma Emerg Surg 48, 4069–4078 (2022). https://doi.org/10.1007/s00068-022-01928-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-022-01928-9