Abstract
Background
The management of recurrent diverticulitis after initial non-operative treatment remains controversial. Recurrences after medical treatment have been described up to 36% but only 3 to 5% develop complicated disease.
Aim
To investigate the effectiveness of conservative treatment during a prolonged follow-up after first episode of complicated diverticulitis.
Methods
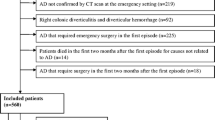
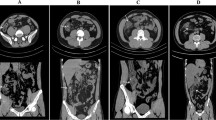
This retrospective single-center study describes the conservative management and outcomes of 207 with complicated acute colonic diverticulitis treated at Parma University Hospital from 1 January 2012 until 31 December 2019. The follow-up was performed until December 2020. Diverticulitis severity was staged according to WSES CT driven classification for acute diverticulitis.
Results
We enrolled 207 patients (118 males, 89 females). The mean age was 59 ± 14.5 years. CT scan of the abdomen was always performed. Almost all patients were treated with bowel rest and antibiotics (98.5%). Percutaneous drainage of abscessed diverticulitis was performed 12 times (5.7%). Average follow-up was 48 ± 28.8 months. 79 patients had new episodes of diverticulitis (38.1%) and 23 patients had high severity new episodes (11.1%). 11 patients underwent surgery (7.7%). Lower CT-Stages showed a higher recurrence rate (P = 0.002). Grade III diverticulitis showed a lower recurrence rate (P = 0.007).
Patients with chronic NSAID use showed a higher incidence of high severity new episodes (P = 0.039).
No recurrence rate differences were noted among patients with or without home therapy (P > 0.05).
Conclusions
Non-operative treatment is an effective and safe option in selected patients with complicated diverticulitis. The recurrence’s severity is generally lower than the previous episodes and this can justify the conservative management.


Similar content being viewed by others
Data availability
The original dataset generated during the current study is available from the corresponding author on reasonable request.
Abbreviations
- ACD:
-
Acute colonic diverticulitis
- NSAID:
-
Nonsteroidal anti-inflammatory drug
References
Kang JY, Hoare J, Tinto A, Subramanian S, Ellis C, Majeed A, Melville D, Maxwell JD. Diverticular disease of the colon–on the rise: a study of hospital admissions in England between 1989/1990 and 1999/2000. Aliment Pharmacol Ther. 2003;17(9):1189–95. https://doi.org/10.1046/j.1365-2036.2003.01551.x (PMID: 12752356).
Nguyen GC, Sam J, Anand N. Epidemiological trends and geographic variation in hospital admissions for diverticulitis in the United States. World J Gastroenterol. 2011;17(12):1600–5. https://doi.org/10.3748/wjg.v17.i12.1600.PMID:21472127 (PMCID: PMC3070132).
Paterson HM, Arnott ID, Nicholls RJ, Clark D, Bauer J, Bridger PC, Crowe AM, Knight AD, Hodgkins P, Solomon D, Dunlop MG. Diverticular disease in Scotland: 2000–2010. Colorectal Dis. 2015;17(4):329–34. https://doi.org/10.1111/codi.12811 (PMID: 25359603).
Jamal Talabani A, Lydersen S, Endreseth BH, Edna TH. Major increase in admission- and incidence rates of acute colonic diverticulitis. Int J Colorectal Dis. 2014;29(8):937–45. https://doi.org/10.1007/s00384-014-1888-9 (Epub 2014 May 8. PMID: 24802814; PMCID: PMC4101254).
Everhart JE, Ruhl CE. Burden of digestive diseases in the United States part II: lower gastrointestinal diseases. Gastroenterology. 2009;136(3):741–54. https://doi.org/10.1053/j.gastro.2009.01.015.
Binda GA, Mataloni F, Bruzzone M, Carabotti M, Cirocchi R, Nascimbeni R, Gambassi G, Amato A, Vettoretto N, Pinnarelli L, Cuomo R, Annibale B. Trends in hospital admission for acute diverticulitis in Italy from 2008 to 2015. Tech Coloproctol. 2018;22(8):597–604. https://doi.org/10.1007/s10151-018-1840-z (Epub 2018 Sep 8 PMID: 30196450).
Shahedi K, Fuller G, Bolus R, Cohen E, Vu M, Shah R, Agarwal N, Kaneshiro M, Atia M, Sheen V, Kurzbard N, van Oijen MG, Yen L, Hodgkins P, Erder MH, Spiegel B. Long-term risk of acute diverticulitis among patients with incidental diverticulosis found during colonoscopy. Clin Gastroenterol Hepatol. 2013;11(12):1609–13. https://doi.org/10.1016/j.cgh.2013.06.020 (Epub 2013 Jul 12. PMID: 23856358; PMCID: PMC5731451).
Stollman N, Raskin JB. Diverticular disease of the colon. Lancet. 2004;363(9409):631–9. https://doi.org/10.1016/S0140-6736(04)15597-9 (PMID: 14987890).
Rustom LBO, Sharara AI. The natural history of colonic diverticulosis: much ado about nothing? Inflamm Intest Dis. 2018;3(2):69–74. https://doi.org/10.1159/000490054 (Epub 2018 Jul 12. PMID: 30733950; PMCID: PMC6361501).
Bharucha AE, Parthasarathy G, Ditah I, Fletcher JG, Ewelukwa O, Pendlimari R, Yawn BP, Melton LJ, Schleck C, Zinsmeister AR. Temporal trends in the incidence and natural history of diverticulitis: a population-based study. Am J Gastroenterol. 2015;110(11):1589–96. https://doi.org/10.1038/ajg.2015.302 (Epub 2015 Sep 29. PMID: 26416187; PMCID: PMC4676761).
Peery AF, Dellon ES, Lund J, Crockett SD, McGowan CE, Bulsiewicz WJ, Gangarosa LM, Thiny MT, Stizenberg K, Morgan DR, Ringel Y, Kim HP, DiBonaventura MD, Carroll CF, Allen JK, Cook SF, Sandler RS, Kappelman MD, Shaheen NJ. Burden of gastrointestinal disease in the United States: 2012 update. Gastroenterology. 2012;143(5):1179-1187.e3. https://doi.org/10.1053/j.gastro.2012.08.002 (Epub 2012 Aug 8. PMID: 22885331; PMCID: PMC3480553).
Humes DJ, Solaymani-Dodaran M, Fleming KM, Simpson J, Spiller RC, West J. A population-based study of perforated diverticular disease incidence and associated mortality. Gastroenterology. 2009;136(4):1198–205. https://doi.org/10.1053/j.gastro.2008.12.054 (Epub 2008 Dec 27 PMID: 19185583).
Klarenbeek BR, Samuels M, van der Wal MA, van der Peet DL, Meijerink WJ, Cuesta MA. Indications for elective sigmoid resection in diverticular disease. Ann Surg. 2010;251(4):670–4. https://doi.org/10.1097/SLA.0b013e3181d3447d (PMID: 20224374).
Stocchi L. Current indications and role of surgery in the management of sigmoid diverticulitis. World J Gastroenterol. 2010;16(7):804–17. https://doi.org/10.3748/wjg.v16.i7.804 (PMID:20143459;PMCID:PMC2825327).
Wong WD, Wexner SD, Lowry A, Vernava A 3rd, Burnstein M, Denstman F, Fazio V, Kerner B, Moore R, Oliver G, Peters W, Ross T, Senatore P, Simmang C. Practice parameters for the treatment of sigmoid diverticulitis–supporting documentation. The standards task force. The american society of colon and rectal surgeons. Dis Colon Rectum. 2000;43(3):290–7. https://doi.org/10.1007/BF02258291 (PMID: 10733108).
Ritz JP, Lehmann KS, Frericks B, Stroux A, Buhr HJ, Holmer C. Outcome of patients with acute sigmoid diverticulitis: multivariate analysis of risk factors for free perforation. Surgery. 2011;149(5):606–13. https://doi.org/10.1016/j.surg.2010.10.005 (Epub 2010 Dec 10 PMID: 21145569).
Haglund U, Hellberg R, Johnsén C, Hultén L. Complicated diverticular disease of the sigmoid colon. an analysis of short and long term outcome in 392 patients. Ann Chir Gynaecol. 1979;68(2):41–6 (PMID: 507737).
Schultz JK, Azhar N, Binda GA, Barbara G, Biondo S, Boermeester MA, Chabok A, Consten ECJ, van Dijk ST, Johanssen A, Kruis W, Lambrichts D, Post S, Ris F, Rockall TA, Samuelsson A, Di Saverio S, Tartaglia D, Thorisson A, Winter DC, Bemelman W, Angenete E. European society of coloproctology: guidelines for the management of diverticular disease of the colon. Colorectal Dis. 2020. https://doi.org/10.1111/codi.15140 (Epub ahead of print. PMID: 32638537).
Sartelli M, Weber DG, Kluger Y, Ansaloni L, Coccolini F, Abu-Zidan F, Augustin G, Ben-Ishay O, Biffl WL, Bouliaris K, Catena R, Ceresoli M, Chiara O, Chiarugi M, Coimbra R, Cortese F, Cui Y, Damaskos D, De’ Angelis GL, Delibegovic S, Demetrashvili Z, De Simone B, Di Marzo F, Di Saverio S, Duane TM, Faro MP, Fraga GP, Gkiokas G, Gomes CA, Hardcastle TC, Hecker A, Karamarkovic A, Kashuk J, Khokha V, Kirkpatrick AW, Kok KYY, Inaba K, Isik A, Labricciosa FM, Latifi R, Leppäniemi A, Litvin A, Mazuski JE, Maier RV, Marwah S, McFarlane M, Moore EE, Moore FA, Negoi I, Pagani L, Rasa K, Rubio-Perez I, Sakakushev B, Sato N, Sganga G, Siquini W, Tarasconi A, Tolonen M, Ulrych J, Zachariah SK, Catena F. 2020 update of the WSES guidelines for the management of acute colonic diverticulitis in the emergency setting. World J Emerg Surg. 2020;15(1):32. https://doi.org/10.1186/s13017-020-00313-4 (PMID:32381121;PMCID:PMC7206757).
Eglinton T, Nguyen T, Raniga S, Dixon L, Dobbs B, Frizelle FA. Patterns of recurrence in patients with acute diverticulitis. Br J Surg. 2010;97(6):952–7. https://doi.org/10.1002/bjs.7035 (PMID: 20474006).
Hall JF, Roberts PL, Ricciardi R, Read T, Scheirey C, Wald C, Marcello PW, Schoetz DJ. Long-term follow-up after an initial episode of diverticulitis: what are the predictors of recurrence? Dis Colon Rectum. 2011;54(3):283–8. https://doi.org/10.1007/DCR.0b013e3182028576 (PMID: 21304297).
Peppas G, Bliziotis IA, Oikonomaki D, Falagas ME. Outcomes after medical and surgical treatment of diverticulitis: a systematic review of the available evidence. J Gastroenterol Hepatol. 2007;22(9):1360–8. https://doi.org/10.1111/j.1440-1746.2007.05118.x (PMID: 17716342).
Ritz JP, Gröne J, Engelmann S, Lehmann KS, Buhr HJ, Holmer C. Welchen Erfolg bringt die Sigmaresektion bei der akuten Sigmadivertikulitis tatsächlich Funktionelle Ergebnisse nach operativer und konservativer Therapie What is the actual benefit of sigmoid resection for acute diverticulitisFunctional outcome after surgical and conservative treatment. Chirurg 2013; 84(8):673–80. https://doi.org/10.1007/s00104-013-2485-0. German PMID: 23519381
van Dijk ST, Daniels L, de Korte N, Stockmann HB, Vrouenraets BC, Consten JEC, van der Hoeven BJA, Faneyte IF, Dijkgraaf WMG, Boermeester MA. Dutch diverticular disease (3D) collaborative study group quality of life and persistent symptoms after uncomplicated acute diverticulitis. Dis Colon Rectum. 2019;62(5):608–14. https://doi.org/10.1097/DCR.0000000000001361 (PMID: 30807455).
van de Wall BJM, Stam MAW, Draaisma WA, Stellato R, Bemelman WA, Boermeester MA, Broeders IAMJ, Belgers EJ, Toorenvliet BR, Prins HA, Consten ECJ. DIRECT trial collaborators. surgery versus conservative management for recurrent and ongoing left-sided diverticulitis (DIRECT trial): an open-label, multicentre, randomised controlled trial. Lancet Gastroenterol Hepatol. 2017;2(1):13–22. https://doi.org/10.1016/S2468-1253(16)30109-1 (Epub 2016 Oct 19. PMID: 28404008).
Bolkenstein HE, Consten ECJ, van der Palen J, van de Wall BJM, Broeders IAMJ, Bemelman WA, Lange JF, Boermeester MA, Draaisma WA. Dutch diverticular disease (3D) collaborative study group long-term outcome of surgery versus conservative management for recurrent and ongoing complaints after an episode of diverticulitis: 5-year follow-up results of a multicenter randomized controlled trial (DIRECT-Trial). Ann Surg. 2019;269(4):612–20. https://doi.org/10.1097/SLA.0000000000003033 (PMID: 30247329).
Sartelli M, Moore FA, Ansaloni L, Di Saverio S, Coccolini F, Griffiths EA, Coimbra R, Agresta F, Sakakushev B, Ordoñez CA, Abu-Zidan FM, Karamarkovic A, Augustin G, Costa Navarro D, Ulrych J, Demetrashvili Z, Melo RB, Marwah S, Zachariah SK, Wani I, Shelat VG, Kim JI, McFarlane M, Pintar T, Rems M, Bala M, Ben-Ishay O, Gomes CA, Faro MP, Pereira GA Jr, Catani M, Baiocchi G, Bini R, Anania G, Negoi I, Kecbaja Z, Omari AH, Cui Y, Kenig J, Sato N, Vereczkei A, Skrovina M, Das K, Bellanova G, Di Carlo I, Segovia Lohse HA, Kong V, Kok KY, Massalou D, Smirnov D, Gachabayov M, Gkiokas G, Marinis A, Spyropoulos C, Nikolopoulos I, Bouliaris K, Tepp J, Lohsiriwat V, Çolak E, Isik A, Rios-Cruz D, Soto R, Abbas A, Tranà C, Caproli E, Soldatenkova D, Corcione F, Piazza D, Catena F. A proposal for a CT driven classification of left colon acute diverticulitis. World J Emerg Surg. 2015;19(10):3. https://doi.org/10.1186/1749-7922-10-3 (PMID:25972914;PMCID:PMC4429354).
Sartelli M, Catena F, Abu-Zidan FM, Ansaloni L, Biffl WL, Boermeester MA, Ceresoli M, Chiara O, Coccolini F, De Waele JJ, Di Saverio S, Eckmann C, Fraga GP, Giannella M, Girardis M, Griffiths EA, Kashuk J, Kirkpatrick AW, Khokha V, Kluger Y, Labricciosa FM, Leppaniemi A, Maier RV, May AK, Malangoni M, Martin-Loeches I, Mazuski J, Montravers P, Peitzman A, Pereira BM, Reis T, Sakakushev B, Sganga G, Soreide K, Sugrue M, Ulrych J, Vincent JL, Viale P, Moore EE. Management of intra-abdominal infections: recommendations by the WSES 2016 consensus conference. World J Emerg Surg. 2017;4(12):22. https://doi.org/10.1186/s13017-017-0132-7 (PMID:28484510;PMCID:PMC5418731).
Perrone G, Sartelli M, Mario G, Chichom-Mefire A, Labricciosa FM, Abu-Zidan FM, Ansaloni L, Biffl WL, Ceresoli M, Coccolini F, Coimbra R, Demetrashvili Z, Di Saverio S, Fraga GP, Khokha V, Kirkpatrick AW, Kluger Y, Leppaniemi A, Maier RV, Moore EE, Negoi I, Ordonez CA, Sakakushev B, Lohse HAS, Velmahos GC, Wani I, Weber DG, Bonati E, Catena F. Management of intra-abdominal-infections: 2017 world society of emergency surgery guidelines summary focused on remote areas and low-income nations. Int J Infect Dis. 2020;99:140–8. https://doi.org/10.1016/j.ijid.2020.07.046 (Epub 2020 Jul 31 PMID: 32739433).
Sigurdardottir J, Chabok A, Thorisson A, Smedh K, Nikberg M. Elective surgery should be considered after successful conservative treatment of recurrent diverticular abscesses. Scand J Gastroenterol. 2020;55(4):454–9. https://doi.org/10.1080/00365521.2020.1740940 (Epub 2020 Mar 23 PMID: 32202966).
Buchwald P, Dixon L, Wakeman CJ, Eglinton TW, Frizelle FA. Hinchey I and II diverticular abscesses: long-term outcome of conservative treatment. ANZ J Surg. 2017;87(12):1011–4. https://doi.org/10.1111/ans.13501 (Epub 2016 Apr 8 PMID: 27062439).
Gregersen R, Mortensen LQ, Burcharth J, Pommergaard HC, Rosenberg J. Treatment of patients with acute colonic diverticulitis complicated by abscess formation: a systematic review. Int J Surg. 2016;35:201–8. https://doi.org/10.1016/j.ijsu.2016.10.006 (Epub 2016 Oct 11 PMID: 27741423).
Li D, de Mestral C, Baxter NN, McLeod RS, Moineddin R, Wilton AS, Nathens AB. Risk of readmission and emergency surgery following nonoperative management of colonic diverticulitis: a population-based analysis. Ann Surg. 2014;260(3):423–30. https://doi.org/10.1097/SLA.0000000000000870 (discussion 430–1 PMID: 25115418).
Benn PL, Wolff BG, Ilstrup DM. Level of anastomosis and recurrent colonic diverticulitis. Am J Surg. 1986;151(2):269–71. https://doi.org/10.1016/0002-9610(86)90085-1 (PMID: 3946763).
Thaler K, Baig MK, Berho M, Weiss EG, Nogueras JJ, Arnaud JP, Wexner SD, Bergamaschi R. Determinants of recurrence after sigmoid resection for uncomplicated diverticulitis. Dis Colon Rectum. 2003;46(3):385–8. https://doi.org/10.1007/s10350-004-6560-y (PMID: 12626916).
Thornblade LW, Simianu VV, Davidson GH, Flum DR. Elective surgery for diverticulitis and the risk of recurrence and ostomy. Ann Surg. 2019. https://doi.org/10.1097/SLA.0000000000003639 (Epub ahead of print. PMID: 31651534; PMCID: PMC7174092).
Egger B, Peter MK, Candinas D. Persistent symptoms after elective sigmoid resection for diverticulitis. Dis Colon Rectum. 2008;51(7):1044–8. https://doi.org/10.1007/s10350-008-9234-3 (Epub 2008 May 1 PMID: 18449609).
Haas JM, Singh M, Vakil N. Mortality and complications following surgery for diverticulitis: systematic review and meta-analysis. United Eur Gastroenterol J. 2016;4(5):706–13. https://doi.org/10.1177/2050640615617357 (Epub 2015 Nov 13. PMID: 27733913; PMCID: PMC5042306).
Chapman JR, Dozois EJ, Wolff BG, Gullerud RE, Larson DR. Diverticulitis: a progressive disease? do multiple recurrences predict less favorable outcomes? Ann Surg. 2006;243(6):876–830. https://doi.org/10.1097/01.sla.0000219682.98158.11 (discussion 880–3.PMID: 16772791; PMCID: PMC1570566).
Justin V, Uranues S, Rabl H, Fingerhut A. Quality of life in uncomplicated recurrent diverticulitis: surgical vs conservative treatment. Sci Rep. 2020;10(1):10261. https://doi.org/10.1038/s41598-020-67094-3 (PMID: 32581229; PMCID: PMC7314856).
Elagili F, Stocchi L, Ozuner G, Kiran RP. Antibiotics alone instead of percutaneous drainage as initial treatment of large diverticular abscess. Tech Coloproctol. 2015;19(2):97–103. https://doi.org/10.1007/s10151-014-1250-9 (Epub 2014 Nov 23 PMID: 25417122).
Strate LL, Liu YL, Huang ES, Giovannucci EL, Chan AT. Use of aspirin or nonsteroidal anti-inflammatory drugs increases risk for diverticulitis and diverticular bleeding. Gastroenterology. 2011;140(5):1427–33. https://doi.org/10.1053/j.gastro.2011.02.004 (Epub 2011 Feb 12. PMID: 21320500; PMCID: PMC3081980).
Reichert MC, Krawczyk M, Appenrodt B, Casper M, Friesenhahn-Ochs B, Grünhage F, Jüngst C, Zimmer V, Lammert F, Dauer M. Selective association of nonaspirin NSAIDs with risk of diverticulitis. Int J Colorectal Dis. 2018;33(4):423–30. https://doi.org/10.1007/s00384-018-2968-z (Epub 2018 Feb 6 PMID: 29411119).
Campbell K, Steele RJ. Non-steroidal anti-inflammatory drugs and complicated diverticular disease: a case-control study. Br J Surg. 1991;78(2):190–1. https://doi.org/10.1002/bjs.1800780218 (PMID: 2015469).
Humes DJ, Fleming KM, Spiller RC, West J. Concurrent drug use and the risk of perforated colonic diverticular disease: a population-based case-control study. Gut. 2011;60(2):219–24. https://doi.org/10.1136/gut.2010.217281 (Epub 2010 Oct 12 PMID: 20940283).
Kruis W, Germer CT, Leifeld L. German society for gastroenterology, digestive and metabolic diseases and the german society for general and visceral surgery diverticular disease: guidelines of the german society for gastroenterology, digestive and metabolic diseases and the german society for general and visceral surgery. Digestion. 2014;90(3):190–207. https://doi.org/10.1159/000367625 (Epub 2014 Nov 19. PMID: 25413249).
Perrone G, Giuffrida M, Bonati E, et al. Conservative management of complicated colonic diverticulitis in early and late elderly. Medicina (Kaunas). 2021;58(1):29. https://doi.org/10.3390/medicina58010029 (Published 2021 Dec 24).
Carter F, Alsayb M, Marshall JK, Yuan Y. Mesalamine (5-ASA) for the prevention of recurrent diverticulitis. Cochrane Database Syst Rev. 2017;10(10):CD009839. https://doi.org/10.1002/14651858.CD009839.pub2 (PMID: 28973845; PMCID: PMC6485423).
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
Author information
Authors and Affiliations
Contributions
All authors participated equally in this research and preparation of manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The author declares no competing interest.
Ethical approval
The study has been approved by independent ethics committee (Comitato etico AVEN – area vasta Emilia nord).
Consent to participate
All study participants or their legal guardian provided informed written consent about personal and medical data collection prior to study enrolment.
Rights and permissions
About this article
Cite this article
Perrone, G., Giuffrida, M., Tarasconi, A. et al. Conservative management of complicated colonic diverticulitis: long-term results. Eur J Trauma Emerg Surg 49, 2225–2233 (2023). https://doi.org/10.1007/s00068-022-01922-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-022-01922-1