Abstract
Purpose
It has been suggested to define the Trauma-induced coagulopathy (TIC) with a PTratio threshold of 1.20. We hypothesized that a more pragmatic classification would grade severity according to the PTratio (or corresponding ROTEM clotting time: EXTEM-CT), and that this would correlate better with the need for blood products (BP) and prognosis.
Methods
Retrospective analysis of prospectively collected data of 1076 severely injured patients admitted from 01/2011 to 12/2019 in a university hospital. To determine the number of TIC categories and the best PTratio or EXTEM-CT thresholds for mortality at 24-h, a modified Mazumdar approach was used. Multivariate regression analyses were done to describe the relationship between PTratio and ROTEM parameter subclasses with mortality.
Results
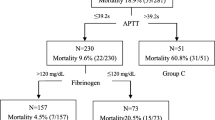
Three thresholds were, respectively, identified for PTratio (1.20, 1.90 and 3.00) and EXTEM-CT (90 s, 130 s, 200 s). The following categories were defined for PTratio: ≤ 1.20 (No TIC), 1.21–1.90 (Moderate TIC), 1.91–3.00 (severe TIC), > 3.00 (major TIC); and for EXTEM-CT: < 91 s (no TIC), 91–130 s (moderate TIC), 131–200 s (severe TIC) and > 200 s (major TIC). We observed that when the PTratio (or EXTEM-CT) increased, mortality and BP requirements increased. After multiple adjustments, we observed that each subclass of PTratio and EXTEM-CT was independently associated with mortality at 24-h.
Conclusion
In this study, we have described a pragmatic classification of coagulopathy utilizing PTratio and EXTEM-CT where increasing severity was associated with prognosis and the amount of BP administered. This could allow clinicians to better predict the outcome and anticipate the need for blood products.



Similar content being viewed by others

Availability of data
The data that support the findings of this study are available on request from the corresponding author, [JSD].
References
Cap A, Hunt B. Acute traumatic coagulopathy. Curr Opin Crit Care. 2014;20(6):638–45.
David JS, Voiglio EJ, Cesareo E, Vassal O, Decullier E, et al. Prehospital parameters can help to predict coagulopathy and massive transfusion in trauma patients. Vox Sang. 2017;112:557–66.
Floccard B, Rugeri L, Faure A, Saint Denis M, Boyle EM, Peguet O, Levrat A, Guillaume C, Marcotte G, Vulliez A, et al. Early coagulopathy in trauma patients: an on-scene and hospital admission study. Injury. 2012;43(1):26–32.
Spahn DR, Bouillon B, Cerny V, Duranteau J, Filipescu D, Hunt BJ, Komadina R, Maegele M, Nardi G, Riddez L, et al. The European guideline on management of major bleeding and coagulopathy following trauma: fifth edition. Crit Care. 2019;23(1):98.
Hess JR, Lindell AL, Stansbury LG, Dutton RP, Scalea TM. The prevalence of abnormal results of conventional coagulation tests on admission to a trauma center. Transfusion. 2009;49(1):34–9.
Peltan ID, Vande Vusse LK, Maier RV, Watkins TR. An international normalized ratio-based definition of acute traumatic coagulopathy is associated with mortality, venous thromboembolism, and multiple organ failure after injury. Crit Care Med. 2015;43(7):1429–38.
Frith D, Goslings JC, Gaarder C, Maegele M, Cohen MJ, Allard S, Johansson PI, Stanworth S, Thiemermann C, Brohi K. Definition and drivers of acute traumatic coagulopathy: clinical and experimental investigations. J Thromb Haemost. 2010;8(9):1919–25.
Guth C, Vassal O, Friggeri A, Wey PF, Inaba K, Decullier E, Ageron FX, David JS. Effects of modification of trauma bleeding management: a before and after study. Anaesth Crit Care Pain Med. 2019;38:469–76.
Brockamp T, Nienaber U, Mutschler M, Wafaisade A, Peiniger S, Lefering R, Bouillon B, Maegele M, TraumaRegister DGU. Predicting on-going hemorrhage and transfusion requirement after severe trauma: a validation of six scoring systems and algorithms on the TraumaRegister DGU. Crit Care. 2012;16(4):R129.
Lefering R, Huber-Wagner S, Nienaber U, Maegele M, Bouillon B. Update of the trauma risk adjustment model of the TraumaRegister DGU: the revised injury severity classification, version II. Crit Care. 2014;18(5):476.
Goodman MD, Makley AT, Hanseman DJ, Pritts TA, Robinson BR. All the bang without the bucks: defining essential point-of-care testing for traumatic coagulopathy. J Trauma Acute Care Surg. 2015;79(1):117–24 (Discussion 124).
David JS, Levrat A, Inaba K, Macabeo C, Rugeri L, Fontaine O, Cheron A, Piriou V. Utility of a point-of-care device for rapid determination of prothrombin time in trauma patients: a preliminary study. J Trauma Acute Care Surg. 2012;72(3):703–7.
Francis RCE, Theurl I, Maegele M, Graw JA. Point-of-care diagnostics of coagulation in the management of bleeding and transfusion in trauma patients. Curr Opin Anaesthesiol. 2020;33(2):246–52.
Bugaev N, Como JJ, Golani G, Freeman JJ, Sawhney JS, Vatsaas CJ, Yorkgitis BK, Kreiner LA, Garcia NM, Aziz HA, et al. Thromboelastography and rotational thromboelastometry in bleeding patients with coagulopathy: practice management guideline from the Eastern Association for the Surgery of Trauma. J Trauma Acute Care Surg. 2020;89(6):999–1017.
Einersen PM, Moore EE, Chapman MP, Moore HB, Gonzalez E, Silliman CC, Banerjee A, Sauaia A. Rapid thrombelastography thresholds for goal-directed resuscitation of patients at risk for massive transfusion. J Trauma Acute Care Surg. 2017;82(1):114–9.
Kelly JM, Rizoli S, Veigas P, Hollands S, Min A. Using rotational thromboelastometry clot firmness at 5 minutes (ROTEM((R)) EXTEM A5) to predict massive transfusion and in-hospital mortality in trauma: a retrospective analysis of 1146 patients. Anaesthesia. 2018;73(9):1103–9.
Veigas PV, Callum J, Rizoli S, Nascimento B, da Luz LT. A systematic review on the rotational thrombelastometry (ROTEM(R)) values for the diagnosis of coagulopathy, prediction and guidance of blood transfusion and prediction of mortality in trauma patients. Scand J Trauma Resusc Emerg Med. 2016;24(1):114.
Schochl H, Cotton B, Inaba K, Nienaber U, Fischer H, Voelckel W, Solomon C. FIBTEM provides early prediction of massive transfusion in trauma. Crit Care. 2011;15(6):R265.
Davenport R, Manson J, De’Ath H, Platton S, Coates A, Allard S, Hart D, Pearse R, Pasi KJ, MacCallum P, et al. Functional definition and characterization of acute traumatic coagulopathy. Crit Care Med. 2011;39(12):2652–8.
Hagemo JS, Christiaans SC, Stanworth SJ, Brohi K, Johansson PI, Goslings JC, Naess PA, Gaarder C. Detection of acute traumatic coagulopathy and massive transfusion requirements by means of rotational thromboelastometry: an international prospective validation study. Crit Care. 2015;19(1):97.
David JS, Bouzat P, Raux M. Evolution and organisation of trauma systems. Anaesth Crit Care Pain Med. 2019;38(2):161–7.
Hans GA, Besser MW. The place of viscoelastic testing in clinical practice. Br J Haematol. 2016;173(1):37–48.
Carll T, Wool GD. Basic principles of viscoelastic testing. Transfusion. 2020;60(Suppl 6):S1–9.
Mazumdar M, Glassman JR. Categorizing a prognostic variable: review of methods, code for easy implementation and applications to decision-making about cancer treatments. Stat Med. 2000;15(19):113–32.
Sartorius D, Le Manach Y, David JS, Rancurel E, Smail N, Thicoipe M, Wiel E, Ricard-Hibon A, Berthier F, Gueugniaud PY, et al. Mechanism, glasgow coma scale, age, and arterial pressure (MGAP): a new simple prehospital triage score to predict mortality in trauma patients. Crit Care Med. 2010;38(3):831–7.
Leemann H, Lustenberger T, Talving P, Kobayashi L, Bukur M, Brenni M, Bruesch M, Spahn DR, Keel MJ. The role of rotation thromboelastometry in early prediction of massive transfusion. J Trauma. 2010;69(6):1403–8.
Daniel Y, Habas S, Malan L, Escarment J, David JS, Peyrefitte S. Tactical damage control resuscitation in austere military environments. J R Army Med Corps. 2016;162:419–27.
Abraham P, Pasquier P, Rimmele T, David JS. Trauma patients do not benefit from a viscoelastic haemostatic assay-guided protocol, but why? Intensive Care Med. 2021;47(6):726–7.
Baksaas-Aasen K, Gall LS, Stensballe J, Juffermans NP, Curry N, Maegele M, Brooks A, Rourke C, Gillespie S, Murphy J, et al. Viscoelastic haemostatic assay augmented protocols for major trauma haemorrhage (ITACTIC): a randomized, controlled trial. Intensive Care Med. 2021;47(1):49–59.
Haider AH, David JS, Zafar SN, Gueugniaud PY, Efron DT, Floccard B, MacKenzie EJ, Voiglio E. Comparative effectiveness of inhospital trauma resuscitation at a French trauma center and matched patients treated in the United States. Ann Surg. 2013;258(1):178–83.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
JSD conceived the study and designed the trial. CC and LF supervised data collection. JSD, LF and CC managed the data. CC and CHV provided statistical advice on study design and analyzed the data. PB, AF, KI and MM did a critical review of the manuscript. JSD drafted the manuscript, and all authors contributed substantially to its revision. JSD takes responsibility for the paper as a whole.
Corresponding author
Ethics declarations
Conflict of interest
JS David and P Bouzat received honoraria for lectures, advisory boards (LFB, Les Ullis, France; Werfen/TEM International, Le pré St Germain, France), M Maegele received honoraria for lectures, speakers’ bureaus, advisory boards and research projects from Astra Zeneca, Bayer, Biotest, CSL Behring, IL-Werfen/TEM International and LFB Biomedicaments. No conflict of interest for the other authors.
Ethics approval
The regional emergency network RESUVAL obtained official approval from the Commission Nationale Informatique et Liberte (DE 2012-059), the CCTIRS (Comité consultatif sur le traitement de l'information en matière de recherche) and the Institutional review board (02/2020).
Informed consent
Written informed consent was not required and all patients (or their next of kin) were provided with information about the registry.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
David, JS., Friggeri, A., Vacheron, CH. et al. Is it possible to improve prediction of outcome and blood requirements in the severely injured patients by defining categories of coagulopathy?. Eur J Trauma Emerg Surg 48, 2751–2761 (2022). https://doi.org/10.1007/s00068-022-01882-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-022-01882-6