Abstract
Purpose
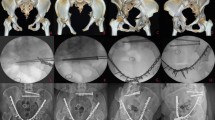
Management of anterior ring injuries is still a matter of discussion, and there are only few studies reporting anterior external fixator as definitive treatment for unstable pelvic injuries. This study aimed to describe the clinical and radiological outcomes of a consecutive series of mechanically unstable pelvic injuries that were treated with definitive anterior supra-acetabular external fixator for the anterior ring, and to identify risk factors for failure.
Methods
We included a consecutive series of patients with unstable pelvic ring fractures who underwent anterior supra-acetabular external fixation for definitive treatment, between January 2012 and January 2020. All demographics, associated injuries and procedures, injury mechanism, and complications were analysed. Pelvic fracture was classified based on Orthopaedic Trauma Association/Tile AO (OTA/AO) and Young–Burgess classifications. Complications associated with the external fixator were revised. All patients were functionally evaluated at final follow-up and asked to report their clinical outcomes using the Majeed score.
Results
A total of 47 patients were included, of which 25 were females. The median age was 44 years (interquartile range 23–59). Median follow-up duration was 14 months (interquartile range 6–31). The most frequent aetiology was motor vehicle accident (35), followed by fall from height (8). All fractures required posterior pelvic ring fixation. The median time during which patients had external fixation in situ was 11 weeks (interquartile range 9–13). All patients achieved healing of pelvic fracture at median time of 10 weeks (interquartile range 8–12). At final follow-up, the median displacement of the anterior pelvis was 6 mm (interquartile range 0–11). Superficial infection was the most common complication (n = 7). No washout procedures were needed. No major complication was reported. No patient required reoperation for anterior ring fracture. The median Majeed score was 88 points (range 60–95; interquartile range 80–90) at final follow-up.
Conclusion
Our findings suggest that the use of supra-acetabular external fixator is safe and effective for definitive treatment of the anterior ring in unstable pelvic fractures. It is a method with high proportion of excellent results, regardless of the type of fracture. The rate of complications is low, and it does not compromise functional results.



Similar content being viewed by others
References
Wojahn RD, Gardner MJ. Fixation of anterior pelvic ring injuries. J Am Acad Orthop Surg. 2019;27:667–76. https://doi.org/10.5435/JAAOS-D-17-00839.
Marecek GS, Scolaro JA. Anterior pelvic ring: introduction to evaluation and management. J Orthop Trauma. 2018;32:8–10. https://doi.org/10.1097/BOT.0000000000001249.
Kleweno CP, Scolaro J, Sciadini MF, McAlister I, Shannon SF, Chip Routt ML. Management of pelvic fractures. Instr Course Lect. 2020;69:489–506.
Gill JR, Murphy C, Quansah B, Carrothers A. Management of the open book APC II pelvis: survey results from pelvic and acetabular surgeons in the United Kingdom. J Orthop. 2017;14:530–6. https://doi.org/10.1016/j.jor.2017.08.004.
Sagi HC, Papp S. Comparative radiographic and clinical outcome of two-hole and multi-hole symphyseal plating. J Orthop Trauma. 2008;22:373–8. https://doi.org/10.1097/BOT.0b013e31817e49ee.
Song W, Zhou D, He Y. Biomechanical characteristics of fixation methods for floating pubic symphysis. J Orthop Surg Res. 2017;12:10–6. https://doi.org/10.1186/s13018-017-0541-z.
Griffin DR, Starr AJ, Reinert CM, Jones AL, Whitlock S. Vertically unstable pelvic fractures fixed with percutaneous iliosacral screws: does posterior injury pattern predict fixation failure? J Orthop Trauma. 2003;17:399–405. https://doi.org/10.1097/00005131-200307000-00001.
Solomon LB, Pohl AP, Sukthankar A, Chehade MJ. The subcristal pelvic external fixator: technique, results, and rationale. J Orthop Trauma. 2009;23:365–9. https://doi.org/10.1097/BOT.0b013e3181a2aec3.
Starr AJ, Nakatani T, Reinert CM, Cederberg K. Superior pubic ramus fractures fixed with percutaneous screws: what predicts fixation failure? J Orthop Trauma. 2008;22:81–7. https://doi.org/10.1097/BOT.0b013e318162ab6e.
Feng Y, Hong J, Guo X, Lin C, Ling W, Zhang L, et al. Percutaneous fixation of traumatic pubic symphysis diastasis using a TightRope and external fixator versus using a cannulated screw. J Orthop Surg Res. 2016;11:1–7. https://doi.org/10.1186/s13018-016-0397-7.
Eastman JG, Krieg JC, Routt MLC. Early failure of symphysis pubis plating. Injury. 2016;47:1707–12. https://doi.org/10.1016/j.injury.2016.05.019.
Collinge C, Archdeacon MT, Dulaney-Cripe E, Moed BR. Radiographic changes of implant failure after plating for pubic symphysis diastasis: an underappreciated reality? Clin Orthop Relat Res. 2012;470:2148–53. https://doi.org/10.1007/s11999-012-2340-5.
Moed BR, Grimshaw CS, Segina DN. Failure of locked design-specific plate fixation of the pubic symphysis: a report of six cases. J Orthop Trauma. 2012;26:e71–5. https://doi.org/10.1097/BOT.0b013e31822c8396.
Morris SAC, Loveridge J, Smart DKA, Ward AJ, Chesser TJS. Is fixation failure after plate fixation of the symphysis pubis clinically important? Clin Orthop Relat Res. 2012;470:2154–60. https://doi.org/10.1007/s11999-012-2427-z.
Hoyt BW, Lundy AE, Purcell RL, Harrington CJ, Gordon WT. Definitive external fixation for anterior stabilization of combat-related pelvic ring injuries, with or without sacroiliac fixation. Clin Orthop Relat Res. 2020;478:779–89. https://doi.org/10.1097/corr.0000000000000961.
Lee C, Sciadini M. The use of external fixation for the management of the unstable anterior pelvic ring. J Orthop Trauma. 2018;32:S14–7. https://doi.org/10.1097/BOT.0000000000001251.
Bellabarba C, Ricci WM, Bolhofner BR. Distraction external fixation in lateral compression pelvic fractures. J Orthop Trauma. 2000;14:475–82. https://doi.org/10.1097/00005131-200009000-00003.
Gänsslen A, Pohlemann T, Krettek C. Supraacetabular external fixation for pelvic ring fractures. Eur J Trauma. 2006;32:489–99. https://doi.org/10.1007/s00068-006-9134-y.
Noordeen MHH, Taylor BA, Briggs TWR, Lavy CBD. Pin placement in pelvic external fixation. Injury. 1993;24:581–4. https://doi.org/10.1016/0020-1383(93)90117-O.
Haidukewych GJ, Kumar S, Prpa B. Placement of half-pins for supra-acetabular external fixation: an anatomic study. Clin Orthop Relat Res. 2003;411:269–73. https://doi.org/10.1097/01.blo.0000069899.31220.d7.
Lidder S, Heidari N, Gänsslen A, Grechenig W. Radiological landmarks for the safe extra-capsular placement of supra-acetabular half pins for external fixation. Surg Radiol Anat. 2013;35:131–5. https://doi.org/10.1007/s00276-012-1016-x.
McDonald C, Firoozabadi R, Routt ML, Kleweno C. Complications associated with pelvic external fixation. Orthopedics. 2017;40:e959–63. https://doi.org/10.3928/01477447-20170918-02.
Scaglione M, Parchi P, Digrandi G, Latessa M, Guido G. External fixation in pelvic fractures. Musculoskelet Surg. 2010;94:63–70. https://doi.org/10.1007/s12306-010-0084-5.
Mitchell PM, Corrigan CM, Patel NA, Silverberg AJ, Greenberg SE, Thakore RV, et al. 13-year experience in external fixation of the pelvis: complications, reduction and removal. Eur J Trauma Emerg Surg. 2016;42:91–6. https://doi.org/10.1007/s00068-015-0499-7.
Guimarães RP, de Góes RA, Ulson O, de Ávila RB, Ono NK, Polesello GC. Supra-acetabular fixation and sacroiliac screws for treating unstable pelvic ring injuries: preliminary results from 20 patients. Rev Bras Ortop (English Ed). 2016;51:132–7. https://doi.org/10.1016/j.rboe.2016.02.010.
Majeed SA. Grading the outcome of pelvic fractures. J Bone Joint Surg Br. 1989;71:304–6. https://doi.org/10.1302/0301-620x.71b2.2925751.
Lefaivre KA, Slobogean GP, Valeriote J, O’Brien PJ, Macadam SA. Reporting and interpretation of the functional outcomes after the surgical treatment of disruptions of the pelvic ring: a systematic review. J Bone Joint Surg Br. 2012;94:549–55. https://doi.org/10.1302/0301-620X.94B4.27960.
Meinberg EG, Agel J, Roberts CS, Karam MD, Kellam JF. Fracture and dislocation classification compendium-2018. J Orthop Trauma. 2018;32(Suppl 1):S1-170. https://doi.org/10.1097/BOT.0000000000001063.
Lefaivre KA, Slobogean G, Starr AJ, Guy P, O’Brien PJ, MacAdam SA. Methodology and interpretation of radiographic outcomes in surgically treated pelvic fractures: a systematic review. J Orthop Trauma. 2012;26:474–81. https://doi.org/10.1097/BOT.0b013e3182323aa2.
Gardner MJ, Nork SE. Stabilization of unstable pelvic fractures with supraacetabular compression external fixation. J Orthop Trauma. 2007;21:269–73. https://doi.org/10.1097/BOT.0b013e318030e3e4.
Sagi HC, Coniglione FM, Stanford JH. Examination under anesthetic for occult pelvic ring instability. J Orthop Trauma. 2011;25:529–36. https://doi.org/10.1097/BOT.0b013e31822b02ae.
Papakostidis C, Kanakaris NK, Kontakis G, Giannoudis PV. Pelvic ring disruptions: treatment modalities and analysis of outcomes. Int Orthop. 2009;33:329–38. https://doi.org/10.1007/s00264-008-0555-6.
Pizanis A, Garcia P, Santelmann M, Culemann U, Pohlemann T. Reduction and fixation capabilities of different plate designs for pubic symphysis disruption: a biomechanical comparison. Injury. 2013;44:183–8. https://doi.org/10.1016/j.injury.2012.09.023.
Merriman DJ, Ricci WM, McAndrew CM, Gardner MJ. Is application of an internal anterior pelvic fixator anatomically feasible? Clin Orthop Relat Res. 2012;470:2111–5. https://doi.org/10.1007/s11999-012-2287-6.
Vaidya R, Colen R, Vigdorchik J, Tonnos F, Sethi A. Treatment of unstable pelvic ring injuries with an internal anterior fixator and posterior fixation: initial clinical series. J Orthop Trauma. 2012;26:1–8. https://doi.org/10.1097/BOT.0b013e318233b8a7.
Yu KH, Hong JJ, Guo XS, Zhou DS. Comparison of reconstruction plate screw fixation and percutaneous cannulated screw fixation in treatment of Tile B1 type pubic symphysis diastasis: a finite element analysis and 10-year clinical experience. J Orthop Surg Res. 2015;10:1–8. https://doi.org/10.1186/s13018-015-0272-y.
Wardle B, Eslick GD, Sunner P. Internal versus external fixation of the anterior component in unstable fractures of the pelvic ring: pooled results from a systematic review. Eur J Trauma Emerg Surg. 2016;42:635–43. https://doi.org/10.1007/s00068-015-0554-4.
Mason WTM, Khan SN, James CL, Chesser TJS, Ward AJ. Complications of temporary and definitive external fixation of pelvic ring injuries. Injury. 2005;36:599–604. https://doi.org/10.1016/j.injury.2004.11.016.
Chiu FY, Chuang TY, Lo WH. Treatment of unstable pelvic fractures: use of a transiliac sacral rod for posterior lesions and an external fixator for anterior lesions. J Trauma Inj Infect Crit Care. 2004;57:141–4. https://doi.org/10.1097/01.ta.0000123040.23231.eb.
Lindahl J, Hirvensalo E, Böstman O, Santavirta S. Failure of reduction with an external fixator in the management of injuries of the pelvic ring. Long-term evaluation of 110 patients. J Bone Joint Surg Br. 1999;81:955–62. https://doi.org/10.1302/0301-620X.81B6.8571.
Kim WY, Hearn TC, Seleem O, Mahalingam E, Stephen D, Tile M. Effect of pin location on stability of pelvic external fixation. Clin Orthop Relat Res. 1999;361:237–44. https://doi.org/10.1097/00003086-199904000-00030.
Stewart RG, Hammer N, Kieser DC. External fixation of unstable pelvic fractures: a systematic review and meta-analysis. ANZ J Surg. 2019;89:1022–7. https://doi.org/10.1111/ans.15027.
Çavusoglu AT, Erbay FK, Özsoy MH, Demir T. Biomechanical comparison of supraacetabular external fixation and anterior pelvic bridge plating. Proc Inst Mech Eng H. 2017;231:931–7. https://doi.org/10.1177/0954411917718223.
Mcdonald E, Theologis AA, Horst P, Kandemir U, Pekmezci M. When do anterior external or internal fixators provide additional stability in an unstable (Tile C) pelvic fracture? A biomechanical study. Eur J Trauma Emerg Surg. 2015;41:665–71. https://doi.org/10.1007/s00068-014-0482-8.
Jordan MC, Brems AC, Heintel T, Jansen H, Hoelscher-Doht S, Meffert RH. The anterior subcutaneous pelvic ring fixator: no biomechanical advantages compared with external fixation. J Bone Joint Surg Am. 2019;101:1724–31. https://doi.org/10.2106/JBJS.18.01363.
MacCormick LM, Chen F, Gilbertson J, Khan S, Schroder LK, Bechtold JE, Cole PA. A biomechanical study comparing minimally invasive anterior pelvic ring fixation techniques to external fixation. Injury. 2018;50(2):251–5. https://doi.org/10.1016/j.injury.2018.07.011.
Stuby FM, Doebele S, Agarwal Y, Windolf M, Gueorguiev B, Ochs BG. Influence of flexible fixation for open book injury after pelvic trauma—a biomechanical study. Clin Biomech. 2014;29:657–63. https://doi.org/10.1016/j.clinbiomech.2014.04.010.
Ohmori T, Kitamura T, Nishida T, Matsumoto T, Tokioka T. The impact of external fixation on mortality in patients with an unstable pelvic ring fracture: a propensity-matched cohort study. Bone Joint J. 2018;100B:233–41. https://doi.org/10.1302/0301-620X.100B2.BJJ-2017-0852.R1.
Tosounidis TH, Sheikh HQ, Kanakaris NK, Giannoudis PV. The use of external fixators in the definitive stabilisation of the pelvis in polytrauma patients: safety, efficacy and clinical outcomes. Injury. 2017;48:1139–46. https://doi.org/10.1016/j.injury.2017.03.033.
Lybrand K, Bell A, Rodericks D, Templeman D, Tornetta P. APC injuries with symphyseal fixation: what affects outcome? J Orthop Trauma. 2017;31:27–30. https://doi.org/10.1097/BOT.0000000000000734.
Stuby FM, Lenz M, Doebele S, et al. Symphyseal fixation in open book injuries cannot fully compensate anterior SI joint injury—a biomechanical study in a two-leg alternating load model. PLoS ONE. 2017;12:1–11. https://doi.org/10.1371/journal.pone.0184000.
Sellei RM, Schandelmaier P, Kobbe P, Knobe M, Pape HC. Can a modified anterior external fixator provide posterior compression of AP compression type III pelvic injuries? Clin Orthop Relat Res. 2013;471:2862–8. https://doi.org/10.1007/s11999-013-2993-8.
Ponson KJ, van Dijke GAH, Joosse P, Snijders CJ. Improvement of external fixator performance in type C pelvic ring injuries by plating of the pubic symphysis: an experimental study on 12 external fixators. J Trauma. 2002;53:907–13. https://doi.org/10.1097/00005373-200211000-00016.
Gardner MJ, Kendoff D, Ostermeier S, Citak M, Hüfner T, Krettek C, et al. Sacroiliac joint compression using an anterior pelvic compressor: a mechanical study in synthetic bone. J Orthop Trauma. 2007;21:435–41. https://doi.org/10.1097/BOT.0b013e318126bb8e.
Funding
No funding was received for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declares that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Barrientos-Mendoza, C., Brañes, J., Wulf, R. et al. The role of anterior supra-acetabular external fixator as definitive treatment for anterior ring fixation in unstable pelvic fractures. Eur J Trauma Emerg Surg 48, 3737–3746 (2022). https://doi.org/10.1007/s00068-021-01711-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-021-01711-2