Abstract
Purpose
To evaluate the recovery of urinary functions and the factors predicting urinary recovery, following delayed decompression in complete cauda equina syndrome (CESR) secondary to Lumbar disc herniation (LDH).
Methods
Retrospective study evaluated 19 cases of CESR due to single-level LDH, all presenting beyond 72 h. Mean delay in decompression was 11.16 ± 7.59 days and follow-up of 31.71 ± 13.90 months. Urinary outcomes were analysed on two scales, a 4-tier ordinal and a dichotomous scale. Logistic regression analysis was used for various predictors including delay in decompression, age, sex, radiation, level of LDH, motor deficits, type and severity of presentation. Time taken to full recovery was correlated with a delay in decompression. using Spearman-correlation.
Results
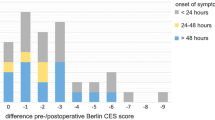
Optimal recovery was seen in 73.7% patients and time to full recovery was moderately correlated with a delay in decompression (r = 0.580, p = 0.030). For those with optimal bladder recovery, mean recovery time was 7.43 ± 5.33 months. Time to decompression and other evaluated factors were not found contributory to urinary outcomes on either scales. Three (15.8%) patients had excellent, 11 (57.9%) had good, while 3 (15.8%) and 2 (10.5%) had fair and poor outcomes respectively.
Conclusions
Occurrence of CESR is not a point of no-return and complete recovery of urinary functions occur even after delayed decompression. Longer delay leads to slower recovery but it is not associated with the extent of recovery. Since time to decompression is positively correlated with time to full recovery, early surgery is still advised in the next available optimal operative setting.
Level of evidence
IV.
Similar content being viewed by others
Data availability
The datasets generated during and/analysed during the current study are available from the corresponding author on reasonable request.
References
Gleave JR, Macfarlane R. Prognosis for recovery of bladder function following lumbar central disc prolapse. Br J Neurosurg. 1990;4(3):205–9. https://doi.org/10.3109/02688699008992725.
Kapetanakis S, Chaniotakis C, Kazakos C, Papathanasiou JV. Cauda equina syndrome due to lumbar disc herniation: a review of literature. Folia Med (Plovdiv). 2017;59(4):377–86. https://doi.org/10.1515/folmed-2017-0038.
Todd NV, Dickson RA. Standards of care in cauda equina syndrome. Br J Neurosurg. 2016;30(5):518–22. https://doi.org/10.1080/02688697.2016.1187254.
Balasubramanian K, Kalsi P, Greenough CG, Kuskoor Seetharam MP. Reliability of clinical assessment in diagnosing cauda equina syndrome. Br J Neurosurg. 2010;24(4):383–6. https://doi.org/10.3109/02688697.2010.505987.
Ahad A, Elsayed M, Tohid H. The accuracy of clinical symptoms in detecting cauda equina syndrome in patients undergoing acute MRI of the spine. Neuroradiol J. 2015;28(4):438–42. https://doi.org/10.1177/1971400915598074.
Angus M, Berg A, Carrasco R, Horner D, Leach J, Siddique I. The Cauda Scale—validation for clinical practice. Br J Neurosurg. 2020. https://doi.org/10.1080/02688697.2020.1754337.
Srikandarajah N, Wilby M, Clark S, Noble A, Williamson P, Marson T. Outcomes reported after surgery for cauda equina syndrome: a systematic literature review. Spine. 2018;43(17):E1005–13. https://doi.org/10.1097/BRS.0000000000002605 (Phila Pa 1976).
Hoeritzauer I, Wood M, Copley PC, Demetriades AK, Woodfield J. What is the incidence of cauda equina syndrome? A systematic review. J Neurosurg Spine. 2020. https://doi.org/10.3171/2019.12.SPINE19839 (published online ahead of print, 14 Feb 2020).
Fraser S, Roberts L, Murphy E. Cauda equina syndrome: a literature review of its definition and clinical presentation. Arch Phys Med Rehabil. 2009;90(11):1964–8. https://doi.org/10.1016/j.apmr.2009.03.021.
Korse NS, Pijpers JA, van Zwet E, Elzevier HW, Vleggeert-Lankamp CLA. Cauda Equina Syndrome: presentation, outcome, and predictors with focus on micturition, defecation, and sexual dysfunction. Eur Spine J. 2017;26(3):894–904. https://doi.org/10.1007/s00586-017-4943-8.
Gleave JR, Macfarlane R. Cauda equina syndrome: what is the relationship between timing of surgery and outcome? Br J Neurosurg. 2002;16(4):325–8. https://doi.org/10.1080/0268869021000032887.
Srikandarajah N, Boissaud-Cooke MA, Clark S, Wilby MJ. Does early surgical decompression in cauda equina syndrome improve bladder outcome? Spine. 2015;40(8):580–3. https://doi.org/10.1097/BRS.0000000000000813(Phila Pa 1976).
Chau AM, Xu LL, Pelzer NR, Gragnaniello C. Timing of surgical intervention in cauda equina syndrome: a systematic critical review. World Neurosurg. 2014;81(3–4):640–50. https://doi.org/10.1016/j.wneu.2013.11.007.
Shapiro S. Medical realities of cauda equina syndrome secondary to lumbar disc herniation. Spine. 2000;25(3):348–52. https://doi.org/10.1097/00007632-200002010-00015 (Phila Pa 1976).
Korse NS, Veldman AB, Peul WC, Vleggeert-Lankamp CL. The long term outcome of micturition, defecation and sexual function after spinal surgery for cauda equina syndrome. PLoS ONE. 2017;12(4):e0175987. https://doi.org/10.1371/journal.pone.0175987.
Song H, Song Q, Sun C, Yu L, Wang Z, Li Y. Early surgery predicts a better prognosis of urinary function in cauda equina syndrome with retention: a systematic review and metaanalysis. Int J Clin Exp Med. 2016;9(2):544–51.
Todd NV. Cauda equina syndrome: the timing of surgery probably does influence outcome. Br J Neurosurg. 2005;19(4):301–6. https://doi.org/10.1080/02688690500305324.
Dhatt S, Tahasildar N, Tripathy SK, Bahadur R, Dhillon M. Outcome of spinal decompression in cauda equina syndrome presenting late in developing countries: case series of 50 cases. Eur Spine J. 2011;20(12):2235–9. https://doi.org/10.1007/s00586-011-1840-4.
Fritz JM, Irrgang JJ. A comparison of a modified Oswestry low back pain disability questionnaire and the Quebec back pain disability scale. Phys Ther. 2001;81(2):776–88. https://doi.org/10.1093/ptj/81.2.776.
Tandon PN, Sankaran B. Cauda equina syndrome due to lumbar disc prolapse. Indian J Orthop. 1967;1(02):112–9.
Delong WB, Polissar N, Neradilek B. Timing of surgery in cauda equina syndrome with urinary retention: meta-analysis of observational studies. J Neurosurg Spine. 2008;8(4):305–20. https://doi.org/10.3171/spi/2008/8/4/305.
Todd NV. Neurological deterioration in cauda equina syndrome is probably progressive and continuous. Implications for clinical management. Br J Neurosurg. 2015;29(5):630–4. https://doi.org/10.3109/02688697.2015.1054364.
Delamarter RB, Sherman J, Carr JB. Cauda equina syndrome: Neurologic recovery following immediate, early, late decompression. Spine. 1991;16:493–9 (Phila Pa 1976).
Pronin S, Koh CH, Bulovaite E, Macleod MR, Statham PF. Compressive pressure versus time in cauda equina syndrome: a systematic review and metaanalysis of experimental studies. Spine. 2019;44(17):1238–47. https://doi.org/10.1097/brs.0000000000003045(Phila Pa 1976).
Rydevik BL, Pedowitz RA, Hargens AR, Swenson MR, Myers RR, Garfin SR. Effects of acute, graded compression on spinal nerve root function and structure. An experimental study of the pig cauda equina. Spine. 1991;16(5):487–93. https://doi.org/10.1097/00007632-199105000-00001 (Phila Pa 1976).
Olmarker KJ, Rydevik BJ, Holm ST. Edema formation in spinal nerve roots induced by experimental, graded compression An experimental study on the pig cauda equina with special reference to differences in effects between rapid and slow onset of compression. Spine. 1989;14(6):569–73 (Phila Pa 1976).
Reddy AP, Mahajan R, Rustagi T, Chhabra HS. Bladder recovery patterns in patients with complete cauda equina syndrome: a single-center study. Asian Spine J. 2018;12(6):981–6. https://doi.org/10.31616/asj.2018.12.6.981.
Ahn UM, Ahn NU, Buchowski JM, Garrett ES, Sieber AN, Kostuik JP. Cauda equina syndrome secondary to lumbar disc herniation: a meta-analysis of surgical outcomes. Spine. 2000;25(12):1515–22. https://doi.org/10.1097/00007632-200006150-00010(Phila Pa 1976).
Kohles SS, Kohles DA, Karp AP, Erlich VM, Polissar NL. Time-dependent surgical outcomes following cauda equina syndrome diagnosis: comments on a meta-analysis. Spine. 2004;29(11):1281–7. https://doi.org/10.1097/00007632-200406010-00019(Phila Pa 1976).
Bečulić H, Skomorac R, Jusić A, et al. Impact of timing on surgical outcome in patients with cauda equina syndrome caused by lumbar disc herniation. Med Glas (Zenica). 2016;13(2):136–41. https://doi.org/10.17392/861-16.
Aly TA, AboRamadan MO. Efficacy of delayed decompression of lumbar disk herniation causing cauda equina syndrome. Orthopedics. 2014;37(2):e153–6. https://doi.org/10.3928/01477447-20140124-18.
Chen C, Fan P, Huang L, Zhen H, Liu L, Wang Y. Percutaneous endoscopic lumbar discectomy as an emergent surgery for cauda equina syndrome caused by lumbar disc herniation. Pain Physician. 2020;23(3):E259–64.
Krishnan A, Kohli R, Degulmadi D, Mayi S, Ranjan R, Dave B. Cauda equina syndrome: a review of 15 patients who underwent percutaneous transforaminal endoscopic lumbar discectomy (PTELD) under local anaesthesia. Malays Orthop J. 2020;14(2):101–10. https://doi.org/10.5704/MOJ.2007.019.
Qureshi A, Sell P. Cauda equina syndrome treated by surgical decompression: the influence of timing on surgical outcome. Eur Spine J. 2007;16(12):2143–51. https://doi.org/10.1007/s00586-007-0491-y.
Bharuka AD, Phunde R, Patel HB. Evaluation of relationship between timing of surgery and functional outcome considering the extent of neurological deficit in patients with cauda equina syndrome secondary to lumbar disc herniation. Int J Res Orthop. 2017;3(5):998–1003. https://doi.org/10.18203/issn.2455-4510.IntJResOrthop20173120.
Kaiser R, Nasto LA, Venkatesan M, Waldauf P, Perez B, Stokes OM, Haddad S, Mehdian H, Tsegaye M. Time factor and disc herniation size: are they really predictive for outcome of urinary dysfunction in patients with cauda equina syndrome? Neurosurgery. 2018;83(6):1193–200. https://doi.org/10.1093/neuros/nyx607.
Heyes G, Jones M, Verzin E, McLorinan G, Darwish N, Eames N. Influence of timing of surgery on cauda equina syndrome: Outcomes at a national spinal centre. J Orthop. 2018;15(1):210–5. https://doi.org/10.1016/j.jor.2018.01.020.
Lai XW, Li W, Wang JX, Zhang HJ, Peng HM, Yang DH. Delayed decompression for cauda equina syndrome secondary to lumbar disc herniation: long-term follow-up results. Nan Fang Yi Ke Da Xue Xue Bao. 2017;37(9):1143–8. https://doi.org/10.3969/j.issn.1673-4254.2017.09.01.
Podnar S, Trsinar B, Vodusek DB. Bladder dysfunction in patients with cauda equina lesions. Neurourol Urodyn. 2006;25(1):23–31. https://doi.org/10.1002/nau.20188.
Funding
No funding was received for the study.
Author information
Authors and Affiliations
Contributions
All authors made substantial contributions in the study, approve the version to be published and agree to be accountable for all aspects of work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The Manuscript submitted does not contain information about medical device(s)/drug(s). No copy righted material has been used in the manuscript. The authors grant permission to reproduce copyrighted materials or signed patient consent forms.
Corresponding author
Ethics declarations
Conflict of interests
The authors declare that they have no conflict of interest.
Ethics approval
Approval by the Institutional Ethical Committee was obtained. All procedures performed in the study involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The study was approved by Institutional Ethical Committee of AIIMS Rishikesh. Approval letter no: AIIMS/IEC/20/91, dated 08.02.2020.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent for publication
Not applicable. No identifying information submitted in the article.
Rights and permissions
About this article
Cite this article
Jha, V., Deep, G., Pandita, N. et al. Factors affecting urinary outcome after delayed decompression in complete cauda equina syndrome: “A regression model study”. Eur J Trauma Emerg Surg 48, 1009–1016 (2022). https://doi.org/10.1007/s00068-020-01589-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-020-01589-6