Abstract
Purpose
Oral anticoagulants (AC) and antiplatelet (AP) agents are increasingly prescribed to prevent and treat acute and chronic thrombotic conditions. The direct oral anticoagulants (DOAC), a newer class of AC, raise concerns in the trauma setting. Our study aims to compare the mortality rates and other outcomes among adult trauma patients based on pre-admission AC/AP status.
Methods
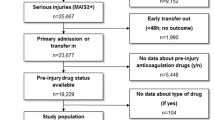
We conducted a retrospective cohort study of a prospectively collected database of trauma patients previously on DOAC, warfarin, aspirin or clopidogrel. A matched control group of trauma patients not receiving AC/AP was used for comparison. Our primary endpoint was in-hospital mortality according to antithrombotic medication class. Secondary endpoints included length of stay (LOS), intensive care unit (ICU) admission, need for blood transfusion, and discharge to a dependent setting. Univariate and multivariate analyses were conducted.
Results
There were 996 exposed patients and 234 controls, with no major clinically significant difference among study groups in terms of gender, injury site, injury severity, mechanism, and comorbidities. The mortality rates were 2.14% (control, 5/234), 2.88% (DOAC, 3/104), 3.34% (aspirin, 17/509), 7.63% (warfarin, 18/236), 9% (clopidogrel, 8/89), and 13.79% (aspirin + clopidogrel, 8/58) (p < 0.001). In multivariate analyses, there was no difference regarding mortality between DOAC and reference groups. Blood transfusion was more likely in patients receiving warfarin or AP than those prescribed DOAC.
Conclusion
There was no evidence of increased mortality or blood transfusion requirement among trauma patients on DOAC, including head trauma patients. Further studies on head trauma and specific subgroups of DOAC are recommended.



Similar content being viewed by others
References
Maung AA, Bhattacharya B, Schuster KM, Davis KA. Trauma patients on new oral anticoagulation agents have lower mortality than those on warfarin. J Trauma Acute Care Surg. 2016;81:652–7. https://doi.org/10.1097/TA.0000000000001189.
Dezman ZD, Comer AC, Smith GS, Narayan M, Hess JR, Hirshon JM. The severity of bleeding and mortality in trauma patients taking Dabigatran. J Emerg Med. 2016;51:238–45. https://doi.org/10.1016/j.jemermed.2016.05.005.
Fohtung RB, Novak E, Rich MW. Effect of new oral anticoagulants on prescribing practices for atrial fibrillation in older adults. J Am Geriatr Soc. 2017;65:2405–12. https://doi.org/10.1111/jgs.15058.
Vranckx P, Valgimigli M, Heidbuchel H. The significance of drug–drug and drug–food interactions of oral anticoagulation. Arrhythm Electrophysiol Rev. 2018;7:55–61. https://doi.org/10.15420/aer.2017.50.1.
Mekaj YH, Mekaj AY, Duci SB, Miftari EI. New oral anticoagulants: their advantages and disadvantages compared with vitamin K antagonists in the prevention and treatment of patients with thromboembolic events. Ther Clin Risk Manag. 2015;11:967–77. https://doi.org/10.2147/TCRM.S84210.
Wood B, Nascimento B, Rizoli S, Sholzberg M, McFarlan A, Phillips A, et al. The anticoagulated trauma patient in the age of the direct oral anticoagulants: a Canadian perspective. Scand J Trauma Resusc Emerg Med. 2017;25:76. https://doi.org/10.1186/s13049-017-0420-y.
Egea-Guerrero JJ, Quintana DM. New oral anticoagulants in severe trauma patients: enemy at the gates? Med Intensiva. 2015;39:167–71. https://doi.org/10.1016/j.medin.2014.09.008.
Feeney JM, Neulander M, DiFiori M, Kis L, Shapiro DS, Jayaraman V, et al. Direct oral anticoagulants compared with warfarin in patients with severe blunt trauma. Injury. 2017;48:47–50. https://doi.org/10.1016/j.injury.2016.08.016.
LaDuke ZJ, Hecht JP, Cain-Nielsen AH, Hemmila MR, Wahl WL. Association of mortality among trauma patients taking preinjury direct oral anticoagulants versus vitamin K antagonists. Surgery. 2019;166:564–71. https://doi.org/10.1016/j.surg.2019.04.039.
Barben J, Menu D, Rosay C, Vovelle J, Mihai AM, Nuss V, et al. The prescription of direct oral anticoagulants in the elderly: an observational study of 19798 ambulatory subjects. Int J Clin Pract. 2019;2019:13420. https://doi.org/10.1111/ijcp.13420.
Kobayashi L, Barmparas G, Bosarge P, Brown CV, Bukur M, Carrick MM, et al. Novel oral anticoagulants and trauma: The results of a prospective American association for the surgery of trauma multi-institutional trial. J Trauma Acute Care Surg. 2017;82:827–35. https://doi.org/10.1097/TA.0000000000001414.
Barletta JF, Hall S, Sucher JF, Dzandu JK, Haley M, Mangram AJ. The impact of pre-injury direct oral anticoagulants compared to warfarin in geriatric G-60 trauma patients. Eur J Trauma Emerg Surg. 2017;43:445–9. https://doi.org/10.1007/s00068-017-0772-z.
Campbell AJ, Spears GF, Borrie MJ. Examination by logistic regression modelling of the variables which increase the relative risk of elderly women falling compared to elderly men. J Clin Epidemiol. 1990;43:1415–20. https://doi.org/10.1016/0895-4356(90)90110-b.
Zeeshan M, Jehan F, O'Keeffe T, Khan M, Zakaria ER, Hamidi M, et al. The novel oral anticoagulants (NOACs) have worse outcomes compared with warfarin in patients with intracranial hemorrhage after TBI. J Trauma Acute Care Surg. 2018;85:915–20. https://doi.org/10.1097/TA.0000000000001995.
Dager WE, Banares L. Reversing the anticoagulation effects of dabigatran. Hosp Pract. 2017;45:29–38. https://doi.org/10.1080/21548331.2017.1298389.
Plitt A, Bansilal S. The nonvitamin K antagonist oral anticoagulants and atrial fibrillation: challenges and considerations. J Atr Fibrillation. 2017;9:1547. https://doi.org/10.4022/jafib.1547.
Mavrakanas TA, Samer C, Fontana P, Perrier A. Direct oral anticoagulants: efficacy and safety in patient subgroups. Swiss Med Wkly. 2015;145:w14081. https://doi.org/10.4414/smw.2015.14081.
Acknowledgements
The study formed part of a master’s thesis of Karry J Felix at the Braun School of Public Health and Community Medicine, Hadassah-Hebrew University. Ellen Sieh provided English language copy editing.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Yuval, J.B., Felix, K.J., Demma, J. et al. Mortality in relation to presence and type of oral antithrombotic agent among adult trauma patients: a single-center retrospective cohort study. Eur J Trauma Emerg Surg 48, 497–505 (2022). https://doi.org/10.1007/s00068-020-01429-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-020-01429-7