Abstract
Purpose
This study sought to investigate the screening accuracy of procalcitonin (PCT) for bacteremia, as defined by a positive blood culture, in a South African trauma ICU.
Methods
This was a retrospective chart review study involving 149 patients who were admitted to the ICU of a level-1 trauma center in South Africa between 2016 and 2017. Median PCT levels in patients with and without positive blood cultures were compared. The screening accuracy of PCT for a positive blood culture was summarized as sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV). Two PCT cut-points were investigated: a general cut-point in the South African context (> 2.0 ng/mL), and a trauma ICU-specific cut-point (prioritizing specificity while optimizing sensitivity) which was determined from a receiver-operator-characteristic curve.
Results
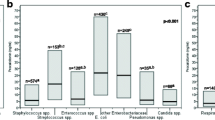
Bacteremic patients had higher median PCT levels when compared with non-bacteremic patients (30.5 ng/mL versus 6.6 ng/mL, p = 0.002). The sensitivity, specificity, PPV, and NPV of PCT > 2.0 ng/mL was 86% (95% confidence interval-CI 71–94%), 29% (CI 22–38%), 28% (CI 20–37%), and 87% (CI 73–94%), respectively. The unit-specific cut-point was PCT > 31.0 ng/mL, which had a sensitivity, specificity, PPV, and NPV of 50% (CI 34–66%), 80% (CI 71–86%), 44% (CI 30–59%), and 83% (CI 75–89%), respectively. Unlike PCT > 2.0 ng/mL, PCT > 31.0 ng/mL demonstrated fair-to-good test specificity in a sub-analysis of patients who underwent recent surgery.
Conclusions
Increased PCT levels were associated with bacteremia in this study. PCT > 31.0 ng/mL may be used to rule in suspected bacteremia in this trauma ICU setting.
Similar content being viewed by others
References
Christaki E, Giamarellos-Bourboulis EJ. The complex pathogenesis of bacteremia: from antimicrobial clearance mechanisms to the genetic background of the host. Virulence. 2014;5(1):57–655.
Valles J, Leon C, Alvarez-Lerma F. Nosocomial bacteremia in critically ill patients: a multicenter study evaluating epidemiology and prognosis. Spanish Collaborative Group for Infections in Intensive Care Units of Sociedad Espanola de Medicina Intensiva y Unidades Coronarias (SEMIUC). Clin Infect Dis. 1997;24(3):387–95.
Laupland KB, Zygun DA, Davies HD, Church DL, Louie TJ, Doig CJ. Population-based assessment of intensive care unit-acquired bloodstream infections in adults: incidence, risk factors, and associated mortality rate. Crit Care Med. 2002;30(11):2462–7.
Garrouste-Orgeas M, Timsit JF, Tafflet M, et al. Excess risk of death from intensive care unit-acquired nosocomial bloodstream infections: a reappraisal. Clin Infect Dis. 2006;42(8):1118–26.
Valles J, Ferrer R. Bloodstream infection in the ICU. Infect Dis Clin North Am. 2009;23(3):557–69.
Gounder M, Hardcastle T, Muckart D. A review of the complications encountered in a quaternary trauma intensive care unit in South Africa. S Afr J Surg. 2019;57(1):43–8.
Calandra T, Cometta A. Antibiotic therapy for gram-negative bacteremia. Infect Dis Clin North Am. 1991;5(4):817–34.
Jin M, Khan AI. Procalcitonin: uses in the clinical laboratory for the diagnosis of sepsis. Lab Med. 2010;41(3):173–7.
Claxton AN, Dark PM. Biomarker-guided antibiotic cessation in sepsis: evidence and future challenges. Br J Hosp Med (Lond). 2018;79(3):136–41.
Hoeboer SH, van der Geest PJ, Nieboer D, Groeneveld AB. The diagnostic accuracy of procalcitonin for bacteraemia: a systematic review and meta-analysis. Clin Microbiol Infect. 2015;21(5):474–81.
Meisner M, Tschaikowsky K, Hutzler A, Schick C, Schuttler J. Postoperative plasma concentrations of procalcitonin after different types of surgery. Intensive Care Med. 1998;24(7):680–4.
Cheddie S, Muckart DJ, Hardcastle TC, Den Hollander D, Cassimjee H, Moodley S. Direct admission versus inter-hospital transfer to a level I trauma unit improves survival: an audit of the new Inkosi Albert Luthuli Central Hospital trauma unit. S Afr Med J. 2011;101(3):176–8.
Vetter TR, Schober P, Mascha EJ. Diagnostic testing and decision-making: beauty is not just in the eye of the beholder. Anesth Analg. 2018;127(4):1085–91.
Maceneaney PM, Malone DE. The meaning of diagnostic test results: a spreadsheet for swift data analysis. Clin Radiol. 2000;55(3):227–35.
Eisenberg MJ. Accuracy and predictive values in clinical decision-making. Cleve Clin J Med. 1995;62(5):311–6.
Parikh R, Mathai A, Parikh S, Chandra Sekhar G, Thomas R. Understanding and using sensitivity, specificity and predictive values. Indian J Ophthalmol. 2008;56(1):45–50.
Bujang MA, Adnan TH. Requirements for minimum sample size for sensitivity and specificity analysis. J Clin Diagn Res. 2016;10(10):Ye01–Ye06.
Caffarini EM, DeMott J, Patel G, Lat I. Determining the clinical utility of an absolute procalcitonin value for predicting a positive culture result. Antimicrob Agents Chemother. 2017;61(5):e02007–e020016.
Yu Y, Li XX, Jiang LX, et al. Procalcitonin levels in patients with positive blood culture, positive body fluid culture, sepsis, and severe sepsis: a cross-sectional study. Infect Dis (Lond). 2016;48(1):63–9.
Yunus I, Fasih A, Wang Y. The use of procalcitonin in the determination of severity of sepsis, patient outcomes and infection characteristics. PLoS ONE. 2018;13(11):e0206527.
Bassetti M, Russo A, Righi E, et al. Role of procalcitonin in bacteremic patients and its potential use in predicting infection etiology. Expert Rev Anti Infect Ther. 2019;17(2):99–105.
Vincent JL, Bassetti M, Francois B, et al. Advances in antibiotic therapy in the critically ill. Crit Care. 2016;20(1):133.
Acknowledgements
The authors thank Gulshan Yashveer Beejan for the assistance with the first draft grammar edit and Ms. Tonya Esterhuizen and Prof. Yoshan Moodley for their statistical expertise.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
No authors declare any conflict of interest. This work is toward the degree MMed(Surgery) for the first author and the third author was the supervisor.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ramasawmy, D., Pillay, M. & Hardcastle, T.C. Correlation of procalcitonin to positive blood culture results in a sample of South African trauma ICU patients between 2016 and 2017. Eur J Trauma Emerg Surg 47, 1183–1188 (2021). https://doi.org/10.1007/s00068-019-01295-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-019-01295-y