Abstract
Purpose
To analyze the reasons and patient-related and injury-related risk factors for reoperation after surgery for acute subdural hematoma (SDH) and the effects of reoperation on treatment outcome.
Methods
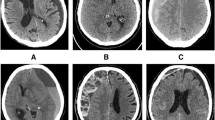
Among adult patients operated on for acute SDH between 2013 and 2017, patients reoperated within 14 days after the primary surgery were identified. In all patients, parameters were identified that related to the patient (age, anticoagulation, antiplatelet, and antiepileptic treatment, and alcohol intoxication), trauma (Glasgow Coma Score, SDH thickness, midline shift, midline shift /hematoma thickness rate, other surgical lesion, primary surgery—trephination, craniotomy, or decompressive craniotomy), and Glasgow Outcome Score (GOS). The reasons for reoperation and intervals between primary surgery and reoperation were studied.
Results
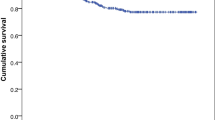
Of 86 investigated patients, 24 patients were reoperated (27.9%), with a median interval of 2 days between primary surgery and reoperation. No significant differences in patients and injury-related factors were found between reoperated and non-reoperated patients. The rate of primary craniectomies was higher in non-reoperated patients (P = 0.066). The main indications for reoperation were recurrent /significant residual SDH (10 patients), contralateral SDH (5 patients), and expansive intracerebral hematoma or contusion (5 patients). The final median GOS was 3 in non-reoperated and 1.5 in reoperated patients, with good outcomes in 41.2% of non-reoperated and 16.7% of reoperated patients.
Conclusions
Reoperation after acute SDH surgery is associated with a significantly worse prognosis. Recurrent /significant residual SDH and contralateral SDH are the most frequently found reasons for reoperation. None of the analyzed parameters were significant reoperation predictors.
Similar content being viewed by others
References
Kwinta BM, Krzyżewski RM, Kliś KM, Donicz P, Gackowska M, Polak J, Stachura K, Moskała M. Emergency reoperations in cranial neurosurgery. World Neurosurg. 2017;105:749–4.
Desai VR, Grossman R, Sparrow H. Incidence of intracranial hemorrhage after a cranial operation. Cureus. 2016;8:e616.
Chen SH, Chen Y, Fang WK, Huang DW, Huang KC, Tseng SH. Comparison of craniotomy and decompressive craniectomy in severely head-injured patients with acute subdural hematoma. J Trauma. 2011;71:1632–6.
Lenzi J, Caporlingua F, Caporlingua A, Anichini G, Nardone A, Passacantilli E, Santoro A. Relevancy of positive trends in mortality and functional recovery after surgical treatment of acute subdural hematomas. Our 10-year experience. Br J Neurosurg. 2017;31:78–83.
Servadei F, Nasi MT, Giuliani G, Cremonin AM, Cenni P, Zappi D, Taylor GS. CT prognostic factors in acute subdural hematomas. The value of the worst CT scan. Br J Neurosurg. 2000;14:110–6.
Al-Mufti F, Mayer SA. Neurocritical care of acute subdural hemorrhage. Neurosurg Clin N Am. 2017;28(2):267–78.
Han H, Koh EJ, Choi H, Kim BC, Yang SY, Cho KT. The effect of preoperative antiplatelet therapy on hemorrhagic complications after decompressive craniectomy in patients with traumatic brain injury. Korean J Neurotrauma. 2016;12:61–6.
Su TM, Lee TH, Chen WF, Lee TC, Cheng CH. Contralateral acute epidural hematoma after decompressive surgery of acute subdural hematoma: clinical features and outcome. J Trauma. 2008;65:1298–302.
Tomycz ND, Germanwala AV, Walter KA. Contralateral acute subdural haematoma after surgical evacuation of acute subdural hematoma. J Trauma. 2010;68:E2–11.
Matsuno A, Katayama H, Wada H, Morikawa K, Tahala K, Tahala H, Murazaki M, Fuke E, Nagashima T. Significance of consecutive bilateral surgeries for patients with acute subdural haematoma who developed contralateral acute epi - or subdural haematoma. Surg Neurol. 2003;60:23–30.
Flordelís Lasierra JL, García Fuentes C, Toral Vázquez D, Chico Fernández M, Bermejo Aznárez S. Alted López E. Contralateral extraaxial hematomas after urgent neurosurgery of a mass lesion in patients with traumatic brain injury. Eur J Trauma Emerg Surg. 2013;39:277–83.
Shen J, Fan Z, Ji T, Pan J, Zhou Y, Zhan R. Contralateral acute subdural haematoma following traumatic acute subdural hematoma evacuation. Neurol Med Chir (Tokyo). 2013;53:221–3.
Kwon H, Choi KS, Yi HJ, Chun HJ, Lee YJ, Kim DW. Risk factors of delayed surgical intervention after conservatively treated acute traumatic subdural Hematoma. J Korean Neurosurg Soc. 2017;60:723–9.
Oertel M, Kelly DF, McArthur D, Boscardin WJ, Glenn TC, Lee JH, Gravori T, Obukhov D, McBride DQ, Martin NA. Progressive hemorrhage after head trauma: predictors and consequences of the evolving injury. J Neurosurg. 2002;96:109–16.
Panczykowski DM, Okonkwo DO. Premorbid oral antithrombotic therapy and risk for reaccumulation, reoperation, and mortality in acute subdural hematomas. J Neurosurg. 2011;114:47–52.
Palmer JD, Sparrow OC, Iannotti F. Postoperative hematoma: a 5-year survey and identification of avoidable risk factors. Neurosurgery. 1994;35:1061–4.
Fabbri A, Servadei BF, Marchesini G, Stein SC, Vandelli A. Predicting intracranial lesion by antiplatelet agents in subjects with mild head injury. J Neurol Neurosurg Psychiatry. 2010;81:1275–9.
Chrastina J, Hrabovský D, Zvarová M, Ríha I, Novák Z. [The effect of anticoagulation and anti-platelet treatment on the extent, development and prognosis of acute craniocerebral injury] [Article in Czech]. Acta Chir Orthop Traumatol Cech. 2014;81:77–84.
Moussa WMM, Khedr WM, Elwany AH. Prognostic significance of hematoma thickness to midline shift ratio in patients with acute intracranial subdural hematoma: a retrospective study. Neurosurg Rev. 2018;41:483–8.
Bartels RH, Meijer FJ, van der Hoeven H, Edwards M, Prokop M. Midline shift in relation to thickness of traumatic acute subdural hematoma predicts mortality. BMC Neurol. 2015;15:220.
Liu X, Qiu Y, Zhang J, Zhang Q, Chen L, Chen L, Sun X. Emergent single burr hole evacuation for traumatic acute subdural hematoma with cerebral herniation: a retrospective cohort comparison analysis. World Neurosurg. 2018. https://doi.org/10.1016/j.wneu.2018.08.219. (Epub ahead of print).
Lu T, Guan J, An C. Preoperative trepanation and drainage for acute subdural hematoma: Two case reports. Exp Ther Med. 2015;10(1):225–30.
Endo H, Fukawa O, Mashiyama S, Kawase M. [Single burr hole surgery for acute spontaneous subdural hematoma in the aged: patient reports of three cases]. No Shinkei Geka. 2004;32(3):271–6.
Di Rienzo A, Iacoangeli M, Almaro L, Colasanti R, Somma LGMD, Nocchi N, Gladi M, Scerrati M. Mini-craniotomy under local anesthesia to treat acute subdural haematoma in deteriorating elderly patient. J Neurol Surg A Centr Eur Neurorosurg. 2017;78:535–40.
Yokosuka K, Uno M, Matsumura K, Takai H, Hagino H, Matsushita N, Matsubara S. Endoscopic haematoma evacuation for acute and subacute subdural hematoma in elderly patient. J Neurosurg. 2015;123:1065–9.
Li X, von Holst H, Kleiven S. Decompressive craniectomy causes a significant strain increase in axonal fiber tracts. J Clin Neurosci. 2013;30:509–13.
Vilcinis R, Bunevicius A, Tamasauskas A. The association of surgical method with outcomes of acute subdural hematoma patients: experience with 643 consecutive patients. World Neurosurg. 2017;101:335–42.
Tsermoulas G, Shah O, Wijesinghe HE, Silva AH, Ramalingam SK, Belli A. Surgery for acute subdural hematoma: replace or remove the bone flap? World Neurosurg. 2016;88:569–75.
Kim H, Suh SJ, Kang HJ, Lee MS, Lee YS, Lee JH, Kang DG. Predictable values of decompressive craniectomy in patients with acute subdural hematoma: comparison between decompressive craniectomy after craniotomy group and craniotomy only group. Korean J Neurotrauma. 2018;14(1):14–9.
Zhao HX, Liao Y, Xu D, Wang QP, Gan Q, You C, Yang CH. The value of intraoperative intracranial pressure monitoring for predicting re-operation using salvage decompressive craniectomy after craniotomy in patients with traumatic mass lesions. BMC Surg. 2015;15:111.
Acknowledgements
The paper was not supported by any grant and received no funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflicts of interest.
Rights and permissions
About this article
Cite this article
Chrastina, J., Šilar, Č., Zeman, T. et al. Reoperations after surgery for acute subdural hematoma: reasons, risk factors, and effects. Eur J Trauma Emerg Surg 46, 347–355 (2020). https://doi.org/10.1007/s00068-019-01077-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-019-01077-6