Abstract
Purpose
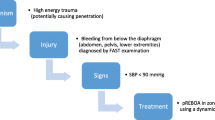
Aortic occlusion (AO) increases proximal perfusion and may improve rates of return of spontaneous circulation (ROSC). The objective of this study was to investigate the hemodynamic effects of cardiopulmonary resuscitation (CPR) and AO by REBOA on patients in traumatic cardiac arrest.
Methods
Patients admitted between February 2013 and May 2017 at a tertiary center who suffered traumatic arrest, had an arterial line placed during resuscitation, and received CPR and REBOA which were included. In-hospital CPR data were obtained from videography. Arterial waveforms were recorded at 240 Hz.
Results
11 consecutive patients were included, 82% male; mean (± SD) age 37 ± 19 years. 55% suffered blunt trauma and the remaining penetrating injuries. 64% arrested out of hospital. During compressions with AO, the mean systolic blood pressure (SBP) was 70 ± 22 mmHg, mean arterial pressure (MAP) 43 ± 19 mmHg, and diastolic blood pressure (DBP) 26 ± 17 mmHg. Nine (82%) had ROSC, with eight having multiple periods of ROSC and arrest in the initial period. In-hospital mortality was 82%. Cardiac ultrasonography was used during arrest in 73%. In two patients with arterial line data before and after AO, SBP (mmHg) improved from 51 to 73 and 55 to 96 during arrest after AO.
Conclusions
High-quality chest compressions coupled with aortic occlusion may generate adequate perfusion pressures to increase the rate of ROSC. New technology capable of transducing central arterial pressure may help us to understand the effectiveness of CPR with and without aortic occlusion. REBOA may be a useful adjunct to high-quality chest compressions during arrest.




Similar content being viewed by others
References
Gräsner JT, Wnent J, Seewald S, Meybohm P, Fischer M, Paffrath T, Wafaisade A, Bein B, Lefering R, German Resuscitation Registry Working Group. Trauma Registry of the German Society for Trauma Surgery (DGU). Cardiopulmonary resuscitation traumatic cardiac arrest there are survivors. An analysis of two national emergency registries. Crit Care. 2011;15(6):R276.
Harris T, Masud S, Lamond A, Abu-Habsa M. Traumatic cardiac arrest: a unique approach. Eur J Emerg Med. 2015;22(2):72–8.
Zwingmann J, Mehlhorn AT, Hammer T, Bayer J, Südkamp NP, Strohm PC. Survival and neurologic outcome after traumatic out-of-hospital cardiopulmonary arrest in a pediatric and adult population: a systematic review. Crit Care. 2012;16(4):R117.
Seamon MJ, Chovanes J, Fox N, Green R, Manis G, Tsiotsias G, Warta M, Ross SE. The use of emergency department thoracotomy for traumatic cardiopulmonary arrest. Injury. 2012;43(9):1355–61.
Brenner ML, Moore LJ, DuBose JJ, Tyson GH, McNutt MK, Albarado RP, Holcomb JB, Scalea TM, Rasmussen TE. A clinical series of resuscitative endovascular balloon occlusion of the aorta for hemorrhage control and resuscitation. J Trauma Acute Care Surg. 2013;75(3):506–11.
DuBose JJ, Scalea TM, Brenner M, Skiada D, Inaba K, Cannon J, Moore L, Holcomb J, Turay D, Arbabi CN, Kirkpatrick A, Xiao J, Skarupa D, Poulin N, AAST AORTA Study Group. The AAST prospective aortic occlusion for resuscitation in trauma and acute care surgery (AORTA) registry: data on contemporary utilization and outcomes of aortic occlusion and resuscitative balloon occlusion of the aorta (REBOA). J Trauma Acute Care Surg. 2016;81(3):409–19.
Gedeborg R, Rubertsson S, Wiklund L. Improved haemodynamics and restoration of spontaneous circulation with constant aortic occlusion during experimental cardiopulmonary resuscitation. Resuscitation. 1999;40(3):171–80.
Rubertsson S, Bircher N, Alexander H. Effects of intra-aortic balloon occlusion on hemodynamics during, and survival after cardiopulmonary resuscitation in dogs. Crit Care Med. 1997;25:1003–9.
Sesma J, Labandeira J, Sara MJ, Espila JL, Arteche A, Saez MJ. Effect of intra-aortic occlusion balloon in external thoracic compressions during CPR in pigs. Am J Emerg Med. 2002;20(5):453–62.
Hu PF, Yang S, Li HC, Stansbury LG, Yang F, Hagegeorge G, Miller C, Rock P, Stein DM, Mackenzie CF. Reliable collection of real-time patient physiologic data from less reliable networks: a “monitor of monitors” system (MoMs). J Med Syst. 2017;41(1):3.
Jennett B, Bond M. Assessment of outcome after severe brain damage. Lancet. 1975;1(7905):480–4.
Reynolds J, Salcido D, Menegazzi J. Coronary perfusion pressure and return of spontaneous circulation after prolonged cardiac arrest. Prehosp Emerg Care. 2010;14(1):78–84.
Paradis NA, Martin GB, Rivers EP, Goetting MG, Appleton TJ, Feingold M, Nowak RM. Coronary perfusion pressure and the return of spontaneous circulation in human cardiopulmonary resuscitation. JAMA J Am Med Assoc. 1990;263(8):1106–13.
Anderson KL, Fiala KC, Castaneda MG, Boudreau SM, Araña AA, Bebarta VS. Left ventricular compressions improve return of spontaneous circulation and hemodynamics in a swine model of traumatic cardiopulmonary arrest. J Trauma Acute Care Surg (Epub 2018 Apr 2).
Watts S, Smith J, Gwyther R, Kirkman E. Closed chest compressions reduce survival in a model of haemorrhage-induced traumatic cardiac arrest. Emerg Med J. 2017;34(12):A866.
Funding
This study was funded in part by a grant from the Department of Defense (Grant number W81XWH-15-1-0025).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. Megan Brenner is a clinical advisory board member for Prytime Medical Inc. Drs. Philip Wasicek, Shiming Yang, William Teeter, Peter Hu, Deborah Stein, and Thomas Scalea declare that they have no conflicts of interest.
Research involving animal and human participants
This study involved human subjects and was compliant with the 1964 Helsinki Declaration and its later amendments, and was compliant with the Institutional Review Board of the University of Maryland, Baltimore.
Ethical approval
This study was approved by the Institutional Review Board of the University of Maryland, Baltimore.
Informed consent
This was a retrospective observational study of prospective collected data, for which formal consent was not required.
Rights and permissions
About this article
Cite this article
Wasicek, P.J., Yang, S., Teeter, W.A. et al. Traumatic cardiac arrest and resuscitative endovascular balloon occlusion of the aorta (REBOA): a preliminary analysis utilizing high fidelity invasive blood pressure recording and videography. Eur J Trauma Emerg Surg 45, 1097–1105 (2019). https://doi.org/10.1007/s00068-018-0989-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-018-0989-5