Abstract
Purpose
There is a lack of association between coagulation biomarkers and long-term mortality in severe trauma. We aimed to investigate the association between coagulation biomarkers on admission and outcome of late stage of trauma.
Methods
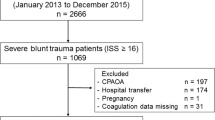
This retrospective observational study included patients admitted with severe trauma between 2012 and 2015. We used the area under the receiver operating characteristic curve (AUROC) of coagulation biomarkers to determine 28-day mortality. Head Abbreviated Injury Scale scores greater than 3 were defined as traumatic brain injury (TBI). The primary outcome was 28-day mortality and the secondary outcome was massive transfusion.
Results
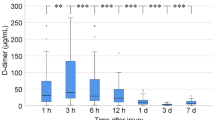
Of the 1266 patients included in the study, 28-day mortality rate was 19.7% (n = 249) and 7.9% (n = 100) of patients received massive transfusion. The AUROC of fibrin/fibrinogen degradation product (FDP) to fibrinogen ratio had a significantly higher prognostic performance than other markers. Multivariate analysis revealed that d-dimer level [odds ratio (OR) 1.033; 95% confidence interval (CI) 1.016–1.051] and FDP/fibrinogen ratio (OR 1.007; 95% CI 1.001–1.013) were independently associated with 28-day mortality. d-dimer (OR 1.028; 95% CI 1.003–1.055) and FDP/fibrinogen ratio (OR 1.035; 95% CI 1.012–1.058) were associated with 28-day mortality in the TBI group. In the non-TBI group, d-dimer was associated with 28-day mortality (OR 1.033; 95% CI 1.008–1.059), but the FDP/fibrinogen ratio was not. FDP/fibrinogen ratio, not d-dimer level, was an independent predictor for massive transfusion (OR 1.005; 95% CI 1.001–1.010).
Conclusions
High FDP/fibrinogen ratio on arrival is a predictor of 28-day mortality and the requirement for massive transfusion in severe trauma.


Similar content being viewed by others
References
MacLeod JB, Winkler AM, McCoy CC, Hillyer CD, Shaz BH. Early trauma induced coagulopathy (ETIC): prevalence across the injury spectrum. Injury. 2014;45:910–5.
Liras IN, Caplan HW, Stensballe J, Wade CE, Cox CS, Cotton BA. Early prediction of acute traumatic coagulopathy. Resuscitation. 2011;82:1208–13.
Hayakawa M, Gando S, Ono Y, Wada T, Yanagida Y, Sawamura A. Fibrinogen level deteriorates before other routine coagulation parameters and massive transfusion in the early phase of severe trauma: a retrospective observational study. Semin Thromb Hemost. 2015;41:35–42.
Cosgriff N, Moore EE, Sauaia A, Kenny-Moynihan M, Burch JM, Galloway B. Predicting life-threatening coagulopathy in the massively transfused trauma patient: hypothermia and acidoses revisited. J Trauma. 1997;42:857 – 61.
Hess JR, Lawson JH. The coagulopathy of trauma versus disseminated intravascular coagulation. J Trauma. 2006;60:S12–S9.
Gando S, Tedo I, Kubota M. Posttrauma coagulation and fibrinolysis. Crit Care Med. 1992;20:594–600.
Gando S. Disseminated intravascular coagulation in trauma patients. Semin Thromb Hemost 2001;27:585–92.
Hayakawa M, Maekawa K, Kushimoto S, et al. High d-dimer levels predict a poor outcome in patients with severe trauma, even with high fibrinogen levels on arrival: a multicenter retrospective study. Shock. 2016;45:308–14.
McQuilten ZK, Wood EM, Bailey M, Cameron PA, Cooper DJ. Fibrinogen is an independent predictor of mortality in major trauma patients: a five-year statewide cohort study. Injury. 2017;48:1074–81.
Sawamura A, Hayakawa M, Gando S, et al. Disseminated intravascular coagulation with a fibrinolytic phenotype at an early phase of trauma predicts mortality. Thromb Res. 2009;124:608–13.
Aoki M, Hagiwara S, Tokue H, et al. Prediction of extravasation in pelvic fracture using coagulation biomarkers. Injury. 2016;47:1702–6.
Skaga NO, Eken T, Jones JM, Steen PA. Different definitions of patient outcome: consequences for performance analysis in trauma. Injury. 2008;39:612–22.
Baker SP, O’Neill B, Haddon W Jr, Long WB. The Injury Severity Score: a method for describing patients with multiple injuries and evaluating emergency care. J Trauma. 1974;14:187–96.
Mellick D, Gerhart KA, Whiteneck GG. Understanding outcomes based on the post-acute hospitalization pathways followed by persons with traumatic brain injury. Brain Inj. 2003;17:55–71.
DeLong ER, DeLong DM, Clarke-Pearson DL. Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics. 1988;44:837–45.
Gando S, Kameue T, Nanzaki S, Nakanishi Y. Massive fibrin formation with consecutive impairment of fibrinolysis in patients with out-of-hospital cardiac arrest. Thromb Haemost. 1997;77:278–82.
Ono Y, Hayakawa M, Maekawa K, et al. Fibrin/fibrinogen degradation products (FDP) at hospital admission predict neurological outcomes in out-of-hospital cardiac arrest patients. Resuscitation. 2017;111:62–7.
Wada H, Sakuragawa N. Are fibrin-related markers useful for the diagnosis of thrombosis? Semin Thromb Hemost. 2008;34:33–8.
Hayakawa M, Sawamura A, Gando S, et al. Disseminated intravascular coagulation at an early phase of trauma is associated with consumption coagulopathy and excessive fibrinolysis both by plasmin and neutrophil elastase. Surgery. 2011;149:221–30.
Gando S, Nakanishi Y, Tedo I. Cytokines and plasminogen activator inhibitor-1 in posttrauma disseminated intravascular coagulation: relationship to multiple organ dysfunction syndrome. Crit Care Med. 1995;23:1835–42.
Dekker SE, Duvekot A, de Vries HM, et al. Relationship between tissue perfusion and coagulopathy in traumatic brain injury. J Surg Res. 2016;205:147–54.
Tian HL, Chen H, Wu BS, et al. D-dimer as a predictor of progressive hemorrhagic injury in patients with traumatic brain injury: analysis of 194 cases. Neurosurg Rev. 2010;33:359–65.
Lansink KW, Gunning AC, Leenen LP. Cause of death and time of death distribution of trauma patients in a Level I trauma centre in the Netherlands. Eur J Trauma Emerg Surg. 2013;39:375–83.
Maegele M. Coagulopathy after traumatic brain injury: incidence, pathogenesis, and treatment options. Transfusion. 2013;53:28Se37.
Oshiro A, Yanagida Y, Gando S, Henzan N, Takahashi I, Makise H. Hemostasis during the early stages of trauma: comparison with disseminated intravascular coagulation. Crit Care. 2014;18:R61.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors (Dong Hun Lee, Byung Kook Lee, Sang Mi Noh, Yong Soo Cho) report no conflicts of interest relevant to this article. No funds were received by any of the authors in support of this study.
Ethical approval
The present study protocol was reviewed and approved by the institutional review board of Chonnam National University College of Medicine (Reg. No. CNUH-2017-076).
Informed consent
Informed consent was waived due to the retrospective nature of the study by the institutional review board.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Lee, D.H., Lee, B.K., Noh, S.M. et al. High fibrin/fibrinogen degradation product to fibrinogen ratio is associated with 28-day mortality and massive transfusion in severe trauma. Eur J Trauma Emerg Surg 44, 291–298 (2018). https://doi.org/10.1007/s00068-017-0844-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-017-0844-0