Abstract
Background
Base deficit provides a more objective indicator of physiological stress following injury as compared with vital signs constituting the revised trauma score (RTS). We have previously developed a base deficit-based trauma survival prediction model [base deficit and injury severity score model (BISS)], in which RTS was replaced by base deficit as a measurement of physiological imbalance.
Purpose
To externally validate BISS in a large cohort of trauma patients and to compare its performance with established trauma survival prediction models including trauma and injury severity score (TRISS) and a severity characterization of trauma (ASCOT). Moreover, we examined whether the predictive accuracy of BISS model could be improved by replacement of injury severity score (ISS) by new injury severity score (NISS) in the BISS model (BNISS).
Methods
In this retrospective, observational study, clinical data of 3737 trauma patients (age ≥15 years) admitted consecutively from 2003 to 2007 were obtained from a prospective trauma registry to calculate BISS, TRISS, and ASCOT models. The models were evaluated in terms of discrimination [area under curve (AUC)] and calibration.
Results
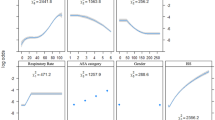
The in-hospital mortality rate was 8.1 %. The discriminative performance of BISS to predict survival was similar to that of TRISS and ASCOT [AUCs of 0.883, 95 % confidence interval (CI) 0.865–0.901 for BISS, 0.902, 95 % CI 0.858–0.946 for TRISS and 0.864, 95 % CI 0.816–0.913 for ASCOT]. Calibration tended to be optimistic in all three models. The updated BNISS had an AUC of 0.918 indicating that substitution of ISS with NISS improved model performance.
Conclusions
The BISS model, a base deficit-based trauma model for survival prediction, showed equivalent performance as compared with that of TRISS and ASCOT and may offer a more simplified calculation method and a more objective assessment. Calibration of BISS model was, however, less good than that of other models. Replacing ISS by NISS can considerably improve model accuracy, but further confirmation is needed.

Similar content being viewed by others
References
Champion HR, Copes WS, Sacco WJ, Lawnick MM, Keast SL, Bain LW Jr, Flanagan ME, Frey CF. The Major Trauma Outcome Study: establishing national norms for trauma care. J Trauma. 1990;30:1356–65.
Hannan EL, Farrell LS, Bessey PQ, Cayten CG, Cooper A, Mottley L. Accounting for intubation status in predicting mortality for victims of motor vehicle crashes. J Trauma. 2000;48:76–81.
Eberhard LW, Morabito DJ, Matthay MA, Mackersie RC, Campbell AR, Marks JD, Alonso JA, Pittet JF. Initial severity of metabolic acidosis predicts the development of acute lung injury in severely traumatized patients. Crit Care Med. 2000;28:125–31.
Juern J, Khatri V, Weigelt J. Base excess: a review. J Trauma Acute Care Surg. 2012;73:27–32.
Davis JW, Parks SN, Kaups KL, Gladen HE, O’Donnell-Nicol S. Admission base deficit predicts transfusion requirements and risk of complications. J Trauma. 1996;41:769–74.
Kroezen F, Bijlsma TS, Liem MS, Meeuwis JD, Leenen LP. Base deficit-based predictive modeling of outcome in trauma patients admitted to intensive care units in Dutch trauma centers. J Trauma. 2007;63:908–13.
Chawda MN, Hildebrand F, Pape HC, Giannoudis PV. Predicting outcome after multiple trauma: which scoring system? Injury. 2004;35:347–58.
Champion HR, Copes WS, Sacco WJ, Lawnick MM, Bain LW, Gann DS, Gennarelli T, Mackenzie E, Schwaitzberg S. A new characterization of injury severity. J Trauma. 1990;30:539–45.
Champion HR, Copes WS, Sacco WJ, Frey CF, Holcroft JW, Hoyt DB, Weigelt JA. Improved predictions from a severity characterization of trauma (ASCOT) over Trauma and Injury Severity Score (TRISS): results of an independent evaluation. J Trauma. 1996;40:42–8.
Lavoie A, Moore L, LeSage N, Liberman M, Sampalis JS. The New Injury Severity Score: a more accurate predictor of in-hospital mortality than the Injury Severity Score. J Trauma. 2004;56:1312–20.
Osler T, Baker SP, Long W. A modification of the injury severity score that both improves accuracy and simplifies scoring. J Trauma. 1997;43:922–5.
Champion HR, Sacco WJ, Copes WS. Injury severity scoring again. J Trauma. 1995;38:94–5.
Rubin DB. Multiple imputation for nonresponse in surveys. New York: Wiley; 1987.
Kincaid EH, Chang MC, Letton RW, Chen JG, Meredith JW. Admission base deficit in pediatric trauma: a study using the National Trauma Data Bank. J Trauma. 2001;51:332–5.
Paladino L, Sinert R, Wallace D, Anderson T, Yadav K, Zehtabchi S. The utility of base deficit and arterial lactate in differentiating major from minor injury in trauma patients with normal vital signs. Resuscitation. 2008;77:363–8.
Lam SW, Leenen LP, van Solinge WW, Hietbrink F, Huisman A. Comparison between the prognostic value of the white blood cell differential count and morphological parameters of neutrophils and lymphocytes in severely injured patients for 7-day in-hospital mortality. Biomarkers. 2012;17:642–7.
Lam SW, Leenen LP, van Solinge WW, Hietbrink F, Huisman A. Evaluation of hematological parameters on admission for the prediction of 7-day in-hospital mortality in a large trauma cohort. Clin Chem Lab Med. 2011;49:493–9.
ten Berg MJ, Huisman A, van den Bemt PM, Schobben AF, Egberts AC, van Solinge WW. Linking laboratory and medication data: new opportunities for pharmacoepidemiological research. Clin Chem Lab Med. 2007;45:13–9.
Compliance with ethical requirements
According to Dutch regulation, this type of study does not require consent by the medical ethical review board.
Conflict of interest
Siu Lam, Hester Lingsma, Ed van Beeck, Loek Leenen declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lam, S.W., Lingsma, H.F., van Beeck, E.F. et al. Validation of a base deficit-based trauma prediction model and comparison with TRISS and ASCOT. Eur J Trauma Emerg Surg 42, 627–633 (2016). https://doi.org/10.1007/s00068-015-0592-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-015-0592-y