Abstract
Purpose
Pediatric fractures are common and are often managed by manipulation under general anesthesia (MUA). This study’s aim was to assess the changing pattern of pediatric fractures over 6 years and use this data to perform a workload forecast and estimate cost implications of treatment under general anesthesia.
Methods
The Emergency Department (ED), operating theater and ward admissions data of children aged 1–11 years presenting with fractures was analyzed. We calculated caseload trends, delay to operation, various parameters of service provision, and the current cost of treating each fracture. We then performed predictive cost analysis for the next 3 years to estimate potential savings by manipulating fractures in ED under ketamine sedation.
Results
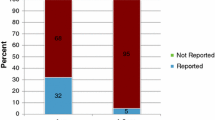
The case load has increased >350% in 6 years (total fractures increasing at 23% and MUAs increasing at 17% per year, respectively). The summer months and evenings have been consistently busier. 72% of fractures were managed by pure reduction alone (MUA), 22% by reduction + K-wires, and various other procedures were performed in 1%. The median delays from ED presentation to admission, definitive procedure and discharge were 4, 21 and 33 h, respectively. Each MUA took 52 min and cost the hospital £723. Assuming that the current trends continue, the expenditures would be £101 K, £114 K, and £128 K for 2010, 2011 and 2012, respectively.
Discussion
Fracture manipulation in children under general anesthesia often requires an overnight hospital stay, which is not only uncomfortable for the child and inconvenient for the parents but it also increases the burden on the limited National Health Service (NHS) resources. There is a 23% annual increase in fractures and children have to wait for 21 h before the definitive procedure. Using ketamine to manipulate children’s fractures in the ED could offer potential service and cost improvements.




Similar content being viewed by others
References
Landin LA. Epidemiology of children’s fractures. J Pediatr Orthop B. 1997;6(2):79–83.
Landin LA. Fracture patterns in children. Analysis of 8,682 fractures with special reference to incidence, etiology and secular changes in a Swedish urban population 1950–1979. Acta Orthop Scand Suppl. 1983;202:1–109.
Wareham K, Johansen A, Stone MD, Saunders J, Jones S, Lyons RA. Seasonal variation in the incidence of wrist and forearm fractures, and its consequences. Injury. 2003;34(3):219–22.
Atherton WG, Harper WM, Abrams KR. A year’s trauma admissions and the effect of the weather. Injury. 2005;36(1):40–6.
Stargatt R, Davidson AJ, Huang GH, Czarnecki C, Gibson MA, Stewart SA, et al. A cohort study of the incidence and risk factors for negative behavior changes in children after general anesthesia. Paediatr Anaesth. 2006;16(8):846–59.
Ben-Amitay G, Kosov I, Reiss A, Toren P, Yoran-Hegesh R, Kotler M, et al. Is elective surgery traumatic for children and their parents? J Paediatr Child Health. 2006;42(10):618–24.
Cramer KE, Glasson S, Mencio G, Green NE. Reduction of forearm fractures in children using axillary block anesthesia. J Orthop Trauma. 1995;9(5):407–10.
Barnes CL, Blasier RD, Dodge BM. Intravenous regional anesthesia: a safe and cost-effective outpatient anesthetic for upper extremity fracture treatment in children. J Pediatr Orthop. 1991;11(6):717–20.
McCarty EC, Mencio GA, Walker LA, Green NE. Ketamine sedation for the reduction of children’s fractures in the emergency department. J Bone Joint Surg Am. 2000;82-A(7):912–8.
McGlone RG, Howes MC, Joshi M. The Lancaster experience of 2.0 to 2.5 mg/kg intramuscular ketamine for paediatric sedation: 501 cases and analysis. Emerg Med J. 2004;21(3):290–5.
Mitchell L, Archer E, Middleton S, Maclean A, Jones L, Benger J, et al. Paediatric distal radial fracture manipulation: multicentre analysis of process times. Emerg Med J. 2009;26(1):41–2.
Varela CD, Lorfing KC, Schmidt TL. Intravenous sedation for the closed reduction of fractures in children. J Bone Joint Surg Am. 1995;77(3):340–5.
Dolansky G, Shah A, Mosdossy G, Rieder M. What is the evidence for the safety and efficacy of using ketamine in children? Paediatr Child Health. 2008;13(4):307–8.
White PF, Way WL, Trevor AJ. Ketamine—its pharmacology and therapeutic uses. Anesthesiology. 1982;56(2):119–36.
Hollister GR, Burn JM. Side effects of ketamine in pediatric anesthesia. Anesth Analg. 1974;53(2):264–7.
Green SM, Johnson NE. Ketamine sedation for pediatric procedures: part 2, review and implications. Ann Emerg Med. 1990;19(9):1033–46.
Leicester City Council (2010) Mid-year population estimates for Leicester. http://www.leicester.gov.uk/your-council-services/council-and-democracy/city-statistics/population-statistics/mid-year-estimates/.
Wootton M, Harris D. Trampolining injuries presenting to a children’s emergency department. Emerg Med J. 2009;26(10):728–31. doi:10.1136/emj.2008.069344.
Hurson C, Browne K, Callender O, O’Donnell T, O’Neill A, Moore DP et al. Pediatric trampoline injuries. J Pediatr Orthop. 2007;27(7):729–32. doi:10.1097/BPO.0b013e318155ab1.
Proudfoot J. Analgesia, anesthesia, and conscious sedation. Emerg Med Clin North Am. 1995;13(2):357–79.
Bourke DL, Malit LA, Smith TC. Respiratory interactions of ketamine and morphine. Anesthesiology. 1987;66(2):153–6.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gulati, A., Dixit, A. & Taylor, G.J. Pediatric fractures: temporal trends and cost implications of treatment under general anesthesia. Eur J Trauma Emerg Surg 38, 59–64 (2012). https://doi.org/10.1007/s00068-011-0130-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-011-0130-5