Abstract
Purpose
The geometric distortion related to magnetic resonance (MR) imaging in a diagnostic radiology (MRDR) and radiotherapy (MRRT) setup is evaluated, and the dosimetric impact of MR distortion on fractionated stereotactic radiotherapy (FSRT) in patients with brain metastases is simulated.
Materials and methods
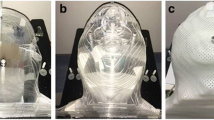
An anthropomorphic skull phantom was scanned using a 1.5‑T MR scanner, and the magnitude of MR distortion was calculated with (MRDR-DC and MRRT-DC) and without (MRDR-nDC and MRRT-nDC) distortion-correction algorithms. Automated noncoplanar volumetric modulated arc therapy (HyperArc, HA; Varian Medical Systems, Palo Alto, CA, USA) plans were generated for 53 patients with 186 brain metastases. The MR distortion at each gross tumor volume (GTV) was calculated using the distance between the center of the GTV and the MR image isocenter (MIC) and the quadratic regression curve derived from the phantom study (MRRT-DC and MRRT-nDC). Subsequently, the radiation isocenter of the HA plans was shifted according to the MR distortion at each GTV (HADC and HAnDC).
Results
The median MR distortions were approximately 0.1 mm when the distance from the MIC was < 30 mm, whereas the median distortion varied widely when the distance was > 60 mm (0.23, 0.47, 0.37, and 0.57 mm in MRDR-DC, MRDR-nDC, MRRT-DC, and MRRT-nDC, respectively). The dose to the 98% of the GTV volume (D98%) decreased as the distance from the MIC increased. In the HADC plans, the relative dose difference of D98% was less than 5% when the GTV was located within 70 mm from the MIC, whereas the underdose of GTV exceeded 5% when it was 48 mm (−26.5% at maximum) away from the MIC in the HAnDC plans.
Conclusion
Use of a distortion-correction algorithm in the studied MR diagnoses is essential, and the dosimetric impact of MR distortion is not negligible, particularly for tumors located far away from the MIC.





Similar content being viewed by others
Abbreviations
- AP:
-
Anterior–posterior
- CT:
-
Computed tomography
- DC:
-
Distortion correction
- DX% :
-
Dose to the X% volume of the gross tumor volume
- FSRT:
-
Fractionated stereotactic radiotherapy
- GTV:
-
Gross tumor volume
- HA:
-
HyperArc
- HADC :
-
HyperArc plan simulating the impact of MR distortion with DC
- HAnDC :
-
HyperArc plan simulating impact of MR distortion without DC
- LR:
-
Left–right
- MIC:
-
MR image isocenter
- MR:
-
Magnetic resonance
- MRDR :
-
MR image in diagnostic radiology setup
- MRDR-DC:
-
MR image in diagnostic radiology setup with DC
- MRDR-nDC:
-
MR image in diagnostic radiology setup without DC
- MRRT :
-
MR image in radiotherapy setup
- MRRT-DC:
-
MR image in radiotherapy setup with DC
- MRRT-nDC:
-
MR image in radiotherapy setup without DC
- PTV:
-
Planning target volume
- RIC:
-
Radiation isocenter
- ShiftAP :
-
Positional shift of GTV due to MR distortion in the AP direction
- ShiftLR :
-
Positional shift of GTV due to MR distortion in the LR direction
- ShiftSI :
-
Positional shift of GTV due to MR distortion in the superior-inferior direction
- SI:
-
Superior–posterior
- SRS:
-
Stereotactic radiosurgery
- TC:
-
Tumor center
- WBRT:
-
Whole-brain radiotherapy
References
Yao S, Zuo H, Li W, Cai Y, Zhang Q, Pang L et al (2023) The correlations between psychological distress, cognitive impairment and quality of life in patients with brain metastases after whole-brain radiotherapy. Clin Transl Oncol 25(1):207–217. https://doi.org/10.1007/s12094-022-02927-3
Chang EL, Wefel JS, Hess KR, Allen PK, Lang FF, Kornguth DG et al (2009) Neurocognition in patients with brain metastases treated with radiosurgery or radiosurgery plus whole-brain irradiation: a randomised controlled trial. Lancet Oncol 10:1037–1044
DeAngelis LM, Delattre JY, Posner JB (1989) Radiation-induced dementia in patients cured of brain metastases. Neurology 39:789–796
Gaebe K, Li AY, Park A, Parmar A, Lok BH, Sahgal A et al (2022) Stereotactic radiosurgery versus whole brain radiotherapy in patients with intracranial metastatic disease and small-cell lung cancer: a systematic review and meta-analysis. Lancet Oncol 23:931–939
van Grinsven EE, Nagtegaal SHJ, Verhoeff JJC, van Zandvoort MJE (2021) The impact of Stereotactic or whole brain radiotherapy on neurocognitive functioning in adult patients with brain metastases: a systematic review and meta-analysis. Oncol Res Treat 44:622–636
Lee WJ, Choi JW, Kong DS, Seol HJ, Nam DH, Lee JI (2022) Clinical outcomes of patients with multiple courses of radiosurgery for brain metastases from non-small cell lung cancer. Sci Rep 12:10712
Ohira S, Ueda Y, Akino Y, Hashimoto M, Masaoka A, Hirata T et al (2018) HyperArc VMAT planning for single and multiple brain metastases stereotactic radiosurgery: a new treatment planning approach. Radiat Oncol 13:13
Kirkpatrick JP, Wang Z, Sampson JH, McSherry F, Herndon JE 2nd, Allen KJ et al (2015) Defining the optimal planning target volume in image-guided stereotactic radiosurgery of brain metastases: results of a randomized trial. Int J Radiat Oncol Biol Phys 91:100–108
Sze G, Milano E, Johnson C, Heier L (1990) Detection of brain metastases: comparison of contrast-enhanced MR with unenhanced MR and enhanced CT. AJNR Am J Neuroradiol 11:785–791
Tong E, McCullagh KL, Iv M (2020) Advanced imaging of brain metastases: from augmenting visualization and improving diagnosis to evaluating treatment response. Front Neurol 11:270
Ulin K, Urie MM, Cherlow JM (2010) Results of a multi-institutional benchmark test for cranial CT/MR image registration. Int J Radiat Oncol Biol Phys 77:1584–1589
Paulson ES, Crijns SP, Keller BM, Wang J, Schmidt MA, Coutts G et al (2016) Consensus opinion on MRI simulation for external beam radiation treatment planning. Radiother Oncol 121:187–192
Zaitsev M, Maclaren J, Herbst M (2015) Motion artifacts in MRI: A complex problem with many partial solutions. J Magn Reson Imaging 42:887–901
Cuccia F, Alongi F, Belka C, Boldrini L, Horner-Rieber J, McNair H et al (2021) Patient positioning and immobilization procedures for hybrid MR-Linac systems. Radiat Oncol 16:183
Koike Y, Akino Y, Sumida I, Shiomi H, Mizuno H, Yagi M et al (2020) Feasibility of synthetic computed tomography generated with an adversarial network for multi-sequence magnetic resonance-based brain radiotherapy. J Radiat Res 61:92–103
Lerner M, Medin J, Jamtheim Gustafsson C, Alkner S, Siversson C, Olsson LE (2021) Clinical validation of a commercially available deep learning software for synthetic CT generation for brain. Radiat Oncol 16:66
Liu X, Emami H, Nejad-Davarani SP, Morris E, Schultz L, Dong M et al (2021) Performance of deep learning synthetic CTs for MR-only brain radiation therapy. J Appl Clin Med Phys 22:308–317
Seibert TM, White NS, Kim GY, Moiseenko V, McDonald CR, Farid N et al (2016) Distortion inherent to magnetic resonance imaging can lead to geometric miss in radiosurgery planning. Pract Radiat Oncol 6:e319–e28
Alzahrani M, Broadbent DA, Chuter R, Al-Qaisieh B, Jackson S, Michael H et al (2020) Audit feasibility for geometric distortion in magnetic resonance imaging for radiotherapy. Phys Imaging Radiat Oncol 15:80–84
Kavaluus H, Nousiainen K, Kaijaluoto S, Seppala T, Saarilahti K, Tenhunen M (2021) Determination of acceptance criteria for geometric accuracy of magnetic resonance imaging scanners used in radiotherapy planning. Phys Imaging Radiat Oncol 17:58–64
Peerlings J, Compter I, Janssen F, Wiggins CJ, Postma AA, Mottaghy FM et al (2019) Characterizing geometrical accuracy in clinically optimised 7T and 3T magnetic resonance images for high-precision radiation treatment of brain tumours. Phys Imaging Radiat Oncol 9:35–42
Mengling V, Bert C, Perrin R, Masitho S, Weissmann T, Mansoorian S et al (2021) Implementation of a dedicated 1.5T MR scanner for radiotherapy treatment planning featuring a novel high-channel coil setup for brain imaging in treatment position. Strahlenther Onkol 197:246–256
Ohira S, Kanayama N, Komiyama R, Ikawa T, Toratani M, Ueda Y et al (2021) Intra-fractional patient setup error during fractionated intracranial stereotactic irradiation treatment of patients wearing medical masks: comparison with and without bite block during COVID-19 pandemic. J Radiat Res 62:163–171
Kanayama N, Ikawa T, Ohira S, Hirata T, Morimoto M, Ogawa K et al (2022) Volumetric reduction of brain metastases after stereotactic radiotherapy: Prognostic factors and effect on local control. Cancer Med 11(24):4806–4815. https://doi.org/10.1002/cam4.4809
Karger CP, Hoss A, Bendl R, Canda V, Schad L (2006) Accuracy of device-specific 2D and 3D image distortion correction algorithms for magnetic resonance imaging of the head provided by a manufacturer. Phys Med Biol 51:N253–61
Schilling KG, Blaber J, Huo Y, Newton A, Hansen C, Nath V et al (2019) Synthesized b0 for diffusion distortion correction (Synb0-DisCo). Magn Reson Imaging 64:62–70
Boudreau M, Tardif CL, Stikov N, Sled JG, Lee W, Pike GB (2017) B(1) mapping for bias-correction in quantitative T(1) imaging of the brain at 3T using standard pulse sequences. J Magn Reson Imaging 46:1673–1682
Torfeh T, Hammoud R, Paloor S, Arunachalam Y, Aouadi S, Al-Hammadi N (2021) Design and construction of a customizable phantom for the characterization of the three-dimensional magnetic resonance imaging geometric distortion. J Appl Clin Med Phys 22:149–157
Yahanda AT, Goble TJ, Sylvester PT, Lessman G, Goddard S, McCollough B et al (2020) Impact of 3‑dimensional versus 2‑dimensional image distortion correction on Stereotactic neurosurgical navigation image fusion reliability for images acquired with Intraoperative magnetic resonance imaging. Oper Neurosurg (hagerstown) 19:599–607
Retif P, Djibo Sidikou A, Mathis C, Letellier R, Verrecchia-Ramos E, Dupres R et al (2022) Evaluation of the ability of the Brainlab elements cranial distortion correction algorithm to correct clinically relevant MRI distortions for cranial SRT. Strahlenther Onkol 198:907–918
Vergalasova I, Liu H, Alonso-Basanta M, Dong L, Li J, Nie K et al (2019) Multi-institutional dosimetric evaluation of modern day Stereotactic Radiosurgery (SRS) treatment options for multiple brain metastases. Front Oncol 9:483
Lucia F, Key S, Dissaux G, Goasduff G, Lucia AS, Ollivier L et al (2019) Inhomogeneous tumor dose distribution provides better local control than homogeneous distribution in stereotactic radiotherapy for brain metastases. Radiother Oncol 130:132–138
Dupic G, Brun L, Molnar I, Leyrat B, Chassin V, Moreau J et al (2021) Significant correlation between gross tumor volume (GTV) D98 % and local control in multifraction stereotactic radiotherapy (MF-SRT) for unresected brain metastases. Radiother Oncol 154:260–268
AAPM (1984) Physical aspects of quality assurance in radiation therapy. American Association of Physicists in Medicine Report Series, vol 13. American Institute of Physics, New York
Kraft J, van Timmeren JE, Mayinger M, Frei S, Borsky K, Stark LS et al (2021) Distance to isocenter is not associated with an increased risk for local failure in LINAC-based single-isocenter SRS or SRT for multiple brain metastases. Radiother Oncol 159:168–175
Kaufmann TJ, Smits M, Boxerman J, Huang R, Barboriak DP, Weller M et al (2020) Consensus recommendations for a standardized brain tumor imaging protocol for clinical trials in brain metastases. Neuro Oncol 22:757–772
Lewis BC, Snyder WJ, Kim S, Kim T (2018) Monitoring frequency of intra-fraction patient motion using the ExacTrac system for LINAC-based SRS treatments. J Appl Clin Med Phys 19:58–63
Ohira S, Komiyama R, Kanayama N, Ueda Y, Inui S, Miyazaki M et al (2022) Intra-fractional motion error during HyperArc stereotactic radiosurgery on patients with brain metastases: Comparison of open and full-face clamshell-style immobilization devices. J Appl Clin Med Phys 23:e13536
Funding
This study was supported by a JSPS KAKENHI grant (Grant-in-Aid for Scientific Research (C) 21K07742).
Author information
Authors and Affiliations
Contributions
All authors participated in the writing of this article and took responsibility for its content. The authors confirm that the content of this manuscript has not been published or submitted for publication elsewhere.
Corresponding author
Ethics declarations
Conflict of interest
S. Ohira, Y. Suzuki, H. Washio, Y. Yamamoto, S. Tateishi, S. Inui, N. Kanayama, M. Kawamata, M. Miyazaki, T. Nishio, M. Koizumi, K. Nakanishi, and K. Konishi declare that they have no competing interests.
Ethical standards
For this article no studies with human participants or animals were performed by any of the authors. All studies mentioned were in accordance with the ethical standards indicated in each case.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ohira, S., Suzuki, Y., Washio, H. et al. Impact of magnetic resonance imaging-related geometric distortion of dose distribution in fractionated stereotactic radiotherapy in patients with brain metastases. Strahlenther Onkol 200, 39–48 (2024). https://doi.org/10.1007/s00066-023-02120-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00066-023-02120-7