Abstract
Background
In addition to local tumor control, the aim of any curative radio-oncological treatment is to maintain quality of life. In the treatment of patients with meningioma with a close relationship to optical structures, the preservation of visual performance is a particular challenge. Use of proton therapy can reduce the dose burden to organs at risk immediately adjacent to the tumor. The aim of this study was to score the subjective assessment of visual performance in patients with meningioma involving the optical structures before and after proton therapy.
Methods
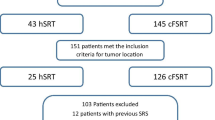
All proton-treated patients with meningioma WHO I whose planning target volumes (PTV) included parts of the optic nerve and/or chiasm were included in this study. Subjective assessment of visual performance was evaluated using the Visual Disorder Scale (VDS) of the EORTC QLQ-BN20 questionnaire. This scale includes values from 0 to 100, whereby high values reflect a high degree of subjective symptom burden and thus subjective visual impairment. The visual acuity in externally performed eye tests at baseline and follow-ups (FU) was also evaluated. The timepoints for testing were before the start of radiotherapy, at the end of treatment, and 3, 6, 12, and 24 months in FU (times t1–t6). All patients with at least the first annual postradiation FU at the time of the evaluation were included. The correlation between VDS changes and potential influencing factors such as previous therapies, dosimetric data, initial tumor volume, and tumor shrinkage 1 year after treatment was assessed.
Results
A total of 56 patients (45 female/11 male) aged 24–82 years (mean ± SD = 53.9 ± 13.3) treated between March 2017 and September 2019 were included in the analysis. The prescription dose was 54.0 Gy (RBE) with active scanned proton therapy. The mean/D2% dose ± SD for the optic chiasm and ipsilateral optic nerve was 43.4 ± 8.9 Gy (RBE)/49.9 ± 7.1 Gy (RBE) and 35.6 ± 11.7 Gy (RBE)/51.7 ± 4.8 Gy (RBE); the mean/D2% dose ± SD of the contralateral optic nerve was 18.8 ± 12.1 Gy (RBE)/42.4 ± 14.6 Gy (RBE), respectively. A total of 302 data collections were available (t1/t2/t3/t4/t5/t6: n = 56/56/48/56/52/34). Median observation time was 23.6 months. Mean symptom burden decreased over time (mean VDS: t1 29.8 ± 27.9; t2 25.0 ± 27.9; t3 21.8 ± 26.0; t4 22.2 ± 26.0; t5 21.4 ± 26.2; t6 17.3 ± 23.6) with statistically significant improvement at 3‑ and 6‑month FU as well as 1 year after proton therapy (p = 0.0205; p = 0.0187; p = 0.0054). Objective eye tests available in 41/52 patients confirm the trend towards improved visual acuity (97.5% stable/improved until 24-month FU). However, no potential predictor for VDS changes was revealed.
Conclusion
Proton treatment of patients with meningioma WHO I with involvement of optical structures does not impair subjective visual performance. After treatment, there is a significant improvement in perceived visual performance.


Similar content being viewed by others
References
Ostrom QT, Patil N, Cioffi G, Waite K, Kruchko C, Barnholtz-Sloan JS (2020) CBTRUS statistical report: primary brain and other central nervous system tumors diagnosed in the United States in 2013–2017. Neuro Oncol 22(12 Suppl 2):iv1–iv96
Nayeni M, Dang A, Mao AJ, Malvankar-Mehta MS (2021) Quality of life of low vision patients: a systematic review and meta-analysis. Can J Ophthalmol 56(3):151–157. https://doi.org/10.1016/j.jcjo.2020.10.014
Karsy M, Jensen MR, Guan J, Ravindra VM, Bisson EF, Couldwell WT (2019) EQ-5D quality-of-life analysis and cost-effectiveness after skull base meningioma resection. Neurosurgery 85(3):E543–E552. https://doi.org/10.1093/neuros/nyz040
Haider S, Taphoorn MJB, Drummond KJ, Walbert T (2021) Health-related quality of life in meningioma. Neuro Oncol Adv 3(1):vdab89. https://doi.org/10.1093/noajnl/vdab089
Fabian A, Domschikowski J, Greiner W, Bockelmann G, Karsten E, Rühle A, Nicolay NH, Grosu AL, Dunst J, Krug D (2022) Financial toxicity in cancer patients treated with radiotherapy in Germany—a cross-sectional study. Strahlenther Onkol. https://doi.org/10.1007/s00066-022-01936-z
Sindou M, Nebbal M, Guclu B (2015) Cavernous sinus meningiomas: imaging and surgical strategy. Adv Tech Stand Neurosurg 42:103–121. https://doi.org/10.1007/978-3-319-09066-5_6
Noel G, Gondi V (2016) Proton therapy for tumors of the base of the skull. Chin Clin Oncol 5(4):51. https://doi.org/10.21037/cco.2016.07.05
Combs SE (2017) Does proton therapy have a future in CNS tumors? Curr Treat Options Neurol 19(3):12. https://doi.org/10.1007/s11940-017-0447-4
Albrecht F, Wolters H, Ziert Y, Timmermann B, Kortmann RD, Matuschek C, Rübe C, Martini C, Christiansen H, Eich HT, Willich N, Steinmann D (2021) Evaluation of treatment-associated eye toxicity after irradiation in childhood and adolescence-results from the registry of the evaluation of side effects after radiotherapy in childhood and adolescence (RiSK). Strahlenther Onkol 197(8):700–710. https://doi.org/10.1007/s00066-021-01793-2
Ahmed KA, Demetriou SK, McDonald M, Johnstone PA (2016) Clinical benefits of proton beam therapy for tumors of the skull base. Cancer Control 23(3):213–219. https://doi.org/10.1177/107327481602300304
Margolis MK, Coyne K, Kennedy-Martin T, Baker T, Schein O, Revicki DA (2002) Vision-specific instruments for the assessment of health-related quality of life and visual functioning: a literature review. PharmacoEconomics 20(12):791–812. https://doi.org/10.2165/00019053-200220120-00001
Taphoorn MJ, Claassens L, Aaronson NK, Coens C, Mauer M, Osoba D, Stupp R, Mirimanoff RO, van den Bent MJ, Bottomley A (2010) An international validation study of the EORTC brain cancer module (EORTC QLQ-BN20) for assessing health-related quality of life and symptoms in brain cancer patients. Eur J Cancer 46(6):1033–1040. https://doi.org/10.1016/j.ejca .2010.01.012
Maringwa J, Quinten C, King M, Ringash J, Osoba D, Coens C, Martinelli F, Reeve BB, Gotay C, Greimel E, Flechtner H, Cleeland CS, Schmucker-Von Koch J, Weis J, Van Den Bent MJ, Stupp R, Taphoorn MJ, Bottomley A (2011) Minimal clinically meaningful differences for the EORTC QLQ-C30 and EORTC QLQ-BN20 scales in brain cancer patients. Ann Oncol 22(9):2107–2112. https://doi.org/10.1093/annonc/mdq726
Osoba D, Rodrigues G, Myles J, Zee B, Pater J (1998) Interpreting the significance of changes in health-related quality-of-life scores. J Clin Oncol 16(1):139–144. https://doi.org/10.1200/JCO.1998.16.1.139
El Shafie RA, Czech M, Kessel KA, Habermehl D, Weber D, Rieken S, Bougatf N, Jäkel O, Debus J, Combs SE (2018) Clinical outcome after particle therapy for meningiomas of the skull base: toxicity and local control in patients treated with active rasterscanning. Radiat Oncol 13(1):54. https://doi.org/10.1186/s13014-018-1002-5
Vernimmen FJ, Harris JK, Wilson JA, Melvill R, Smit BJ, Slabbert JP (2001) Stereotactic proton beam therapy of skull base meningiomas. Int J Radiat Oncol Biol Phys 49(1):99–105. https://doi.org/10.1016/S0360-3016(00)01457-7
Weber DC, Lomax AJ, Rutz HP, Stadelmann O, Egger E, Timmermann B, Pedroni ES, Verwey J, Miralbell R, Goitein G (2004) Spot-scanning proton radiation therapy for recurrent, residual or untreated intracranial meningiomas. Radiother Oncol 71(3):251–258. https://doi.org/10.1016/j.radonc.2004.02.011
Vaishnav YJ, Singh R, Didwania P, Lehrer EJ, Bakaeva T, Harris TJ, Migliori ME, Sheehan JP, Trifiletti DM (2022) Radiotherapy and radiosurgery in the management of optic nerve sheath meningiomas: an international systematic review and meta-analysis of twenty studies. World Neurosurg 164:e929–e944. https://doi.org/10.1016/j.wneu.2022.05.064
Marchetti M, Conti A, Beltramo G, Pinzi V, Pontoriero A, Tramacere I, Senger C, Pergolizzi S, Fariselli L (2019) Multisession radiosurgery for perioptic meningiomas: medium-to-long term results from a CyberKnife cooperative study. J Neurooncol 143(3):597–604. https://doi.org/10.1007/s11060-019-03196-x
Kheir V, Faouzi M, Borruat FX (2019) Visual outcomes of fractionated radiotherapy in optic nerve sheath meningioma: a retrospective study. Klin Monbl Augenheilkd 236(4):526–529. https://doi.org/10.1055/a-0828-7335
Combs SE, Adeberg S, Dittmar JO, Welzel T, Rieken S, Habermehl D, Huber PE, Debus J (2013) Skull base meningiomas: Long-term results and patient self-reported outcome in 507 patients treated with fractionated stereotactic radiotherapy (FSRT) or intensity modulated radiotherapy (IMRT). Radiother Oncol 106(2):186–191. https://doi.org/10.1016/j.radonc.2012.07.008
Castle-Kirszbaum M, Kam J, Dixon B, Goldschlager T, King J, Wang YY (2022) Surgical outcomes and longitudinal quality of life after endoscopic endonasal surgery for anterior skull base meningioma. J Neurosurg. https://doi.org/10.3171/2021.11.JNS212090
Pintea B, Boström A, Katsigiannis S, Gousias K, Pintea R, Baumert B, Boström J (2021) Prognostic factors for functional outcome of patients with optic nerve sheath meningiomas treated with stereotactic radiotherapy-evaluation of own and meta-analysis of published data. Cancers 13(3):522. https://doi.org/10.3390/cancers13030522
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
B. Flechl, L. Konrath, E. Hug, P. Fossati, C. Lütgendorf-Caucig, M. Achtaewa, M. Pelak, and P. Georg declare that they have no competing interests.
Ethical standards
The manuscript was performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Supplementary Information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Flechl, B., Konrath, L., Hug, E. et al. Meningioma WHO I with involvement of the optical structures—does proton therapy lead to changes in quality of life with regard to subjective visual performance?. Strahlenther Onkol 199, 404–411 (2023). https://doi.org/10.1007/s00066-022-02024-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00066-022-02024-y