Abstract
Purpose
Imaging features are known to reflect inherent disease biology in various cancers including brain tumors. We report on the prognostic impact of magnetic resonance imaging (MRI) features on survival in patients with medulloblastoma treated between 2007 and 2018 at our institute.
Methods
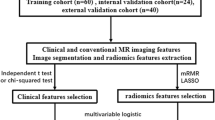
Sixteen semantic imaging features (with predefined categories) were extracted from pre- and postcontrast T1-weighted and T2-weighted MRI by consensus. Univariate analysis and multivariate Cox regression analysis were performed to assess the correlation of semantic features with relapse-free survival (RFS) and overall survival (OS).
Results
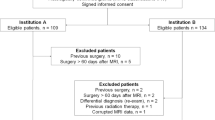
The study cohort comprised 171 medulloblastoma patients (median age 9 years) treated with maximal safe resection followed by risk-stratified adjuvant radio(chemo)therapy. A total of 55 patients experienced recurrent/progressive disease (commonly neuraxial metastases) resulting in 44 deaths, including one treatment-related death. At a median follow-up of 45 months (interquartile range 19–65 months), 5‑year Kaplan–Meier estimates of RFS and OS were 64% and 71%, respectively. Semantic MRI features such as non-central tumor location on vertical axis, absence of brainstem involvement, ≤ 80% solid tumor area with contrast uptake, heterogenous pattern of contrast enhancement, necrosis, calcification, and T2-weighted heterogeneity were associated with significantly worse RFS and/or OS in univariate analysis. Cox regression analysis identified tumor location on the vertical axis, brainstem involvement, and calcification as independent prognostic factors impacting outcomes. Distinctive MRI features correlated with survival even within individual molecular subgroups of medulloblastoma.
Conclusion
Distinctive semantic MRI features correlate significantly with survival outcomes in medulloblastoma, also within individual molecular subgroups, reflecting their prognostic impact.


Similar content being viewed by others
References
Leece R, Xu J, Ostrom QT et al (2017) Global incidence of malignant brain and other central nervous system tumors by histology, 2003–2007. Neuro-Oncology 19:1553–1564. https://doi.org/10.1093/neuonc/nox091
Ostrom QT, Patil N, Cioffi G et al (2020) CBTRUS statistical report: primary brain and other central nervous system tumors diagnosed in the United States in 2013–2017. Neuro-Oncology 22(iv1):iv96. https://doi.org/10.1093/neuonc/noaa200
Northcott PA, Korshunov A, Witt H et al (2011) Medulloblastoma comprises four distinct molecular variants. J Clin Oncol 29:1408–1414. https://doi.org/10.1200/JCO.2009.27.4324
Gajjar A, Bowers DC, Karajannis MA et al (2015) Pediatric brain tumors: innovative genomic information is transforming the diagnostic and clinical landscape. J Clin Oncol 33:2986–2998. https://doi.org/10.1200/JCO.2014.59.9217
Gupta T, Shirsat N, Jalali R (2015) Molecular subgrouping of Medulloblastoma: impact upon research and clinical practice. Curr Pediatr Rev 11:106–119. https://doi.org/10.2174/1573396311666150702104030
Taylor MD, Northcott PA, Korshunov A et al (2012) Molecular subgroups of medulloblastoma: the current consensus. Acta Neuropathol 123:465–472. https://doi.org/10.1007/s00401-011-0922-z
Louis DN, Perry A, Reifenberger G et al (2016) The 2016 World Health Organization classification of tumors of the central nervous system: a summary. Acta Neuropathol 131:803–820. https://doi.org/10.1007/s00401-016-1545-1
Ramaswamy V, Remke M, Bouffet E et al (2016) Risk stratification of childhood medulloblastoma in the molecular era: the current consensus. Acta Neuropathol 131:821–831. https://doi.org/10.1007/s00401-016-1569-6
Kuo MD, Jamshidi N (2014) Behind the numbers: Decoding molecular phenotypes with radiogenomics—Guiding principles and technical considerations. Radiology 270:320–325. https://doi.org/10.1148/radiol.13132195
Gillies RJ, Kinahan PE, Hricak H (2015) Radiomics: images are more than pictures, they are data. Radiology 278:563–577. https://doi.org/10.1148/radiol.2015151169
Kickingereder P, Andronesi OC (2018) Radiomics, metabolic, and molecular MRI for brain tumors. Semin Neurol 38:32–40. https://doi.org/10.1055/s-0037-1618600
Dasgupta A, Gupta T, Pungavkar S et al (2019) Nomograms based on preoperative multiparametric magnetic resonance imaging for prediction of molecular subgrouping in medulloblastoma: results from a radiogenomics study of 111 patients. Neuro-Oncology 21:115–124. https://doi.org/10.1093/neuonc/noy093
Iv M, Zhou M, Shpanskaya K et al (2019) MR imaging-based radiomic signatures of distinct molecular subgroups of Medulloblastoma. AJNR Am J Neuroradiol 40:154–161. https://doi.org/10.3174/ajnr.A5899
Yan J, Liu L, Wang W et al (2020) Radiomic features from multi-parameter MRI combined with clinical parameters predict molecular subgroups in patients with Medulloblastoma. Front Oncol 10:558162. https://doi.org/10.3389/fonc.2020.558162
Dasgupta A, Gupta T (2018) Radiogenomics of medulloblastoma: imaging surrogates of molecular biology. J Transl Genet Genom. https://doi.org/10.20517/jtgg.2018.21
Colafati GS, Voicu IP, Carducci C et al (2018) MRI features as a helpful tool to predict the molecular subgroups of medulloblastoma: state of the art. Ther Adv Neurol Disord. https://doi.org/10.1177/1756286418775375
Kunder R, Jalali R, Sridhar E et al (2013) Real-time PCR assay based on the differential expression of microRNAs and protein-coding genes for molecular classification of formalin-fixed paraffin embedded medulloblastomas. Neuro-Oncology 15:1644–1651. https://doi.org/10.1093/neuonc/not123
Zeltzer PM, Boyett JM, Finlay JL et al (1999) Metastasis stage, adjuvant treatment, and residual tumor are prognostic factors for medulloblastoma in children: conclusions from the Children’s Cancer Group 921 randomized phase III study. J Clin Oncol 17:832–845. https://doi.org/10.1200/JCO.1999.17.3.832
Rabasco Meneghetti A, Zwanenburg A, Löck S (2020) Pictures worth more than a thousand words: Prediction of survival in medulloblastoma patients. EBioMedicine 62:103136. https://doi.org/10.1016/j.ebiom.2020.103136
Gibson P, Tong Y, Robinson G et al (2010) Subtypes of medulloblastoma have distinct developmental origins. Nature 468:1095–1099. https://doi.org/10.1038/nature09587
Thompson EM, Hielscher T, Bouffet E et al (2016) Prognostic value of medulloblastoma extent of resection after accounting for molecular subgroup: a retrospective integrated clinical and molecular analysis. Lancet Oncol 17:484–495. https://doi.org/10.1016/S1470-2045(15)00581-1
Law M, Yang S, Babb JS et al (2004) Comparison of cerebral blood volume and vascular permeability from dynamic susceptibility contrast-enhanced perfusion MR imaging with glioma grade. AJNR Am J Neuroradiol 25:746–755
Łastowska M, Jurkiewicz E, Trubicka J et al (2015) Contrast enhancement pattern predicts poor survival for patients with non-WNT/SHH medulloblastoma tumours. J Neurooncol 123:65–73. https://doi.org/10.1007/s11060-015-1779-0
Liu S, Wang Y, Xu K et al (2017) Relationship between necrotic patterns in glioblastoma and patient survival: fractal dimension and lacunarity analyses using magnetic resonance imaging. Sci Rep. https://doi.org/10.1038/s41598-017-08862-6
Urberuaga A, Navajas A, Burgos J, Pijoán JI (2006) A review of clinical and histological features of Spanish paediatric medulloblastomas during the last 21 years. Childs Nerv Syst 22:466–474. https://doi.org/10.1007/s00381-005-0004-4
Giangaspero F, Wellek S, Masuoka J et al (2006) Stratification of medulloblastoma on the basis of histopathological grading. Acta Neuropathol 112:5–12. https://doi.org/10.1007/s00401-006-0064-x
Verma S, Tavaré CJ, Gilles FH (2008) Histologic features and prognosis in pediatric medulloblastoma. Pediatr Dev Pathol 11:337–343. https://doi.org/10.2350/07-09-0353.1
Michiwaki Y, Hata N, Mizoguchi M et al (2019) Relevance of calcification and contrast enhancement pattern for molecular diagnosis and survival prediction of gliomas based on the 2016 World Health Organization classification. Clin Neurol Neurosurg 187:105556. https://doi.org/10.1016/j.clineuro.2019.105556
Salloum R, Chen Y, Yasui Y et al (2019) Late morbidity and mortality among Medulloblastoma survivors diagnosed across three decades: a report from the childhood cancer survivor study. J Clin Oncol 37:731–740. https://doi.org/10.1200/JCO.18.00969
Acknowledgements
We acknowledge and thank Nazia Bano, Shraddha Churi, and Farnaz Shaikh for their logistic and secretarial assistance during the conduct of the study. We express our gratitude to all patients and their caregivers who participated in the study.
Funding
(i) Intramural grant from Tata Memorial Centre, Mumbai; (ii) Indian Council of Medical Research (ICMR), New Delhi; and (iii) Brain Tumor Foundation (BTF) of India, Mumbai. The funding bodies had no influence on study design, data collection, analysis, interpretation of data, or the manuscript’s writing.
Author information
Authors and Affiliations
Contributions
Conception and design: T. Gupta and R. Jalali conceptualized the study, and A. Dasgupta wrote the study protocol; collection and assembly of data: all authors; data analysis and interpretation: A. Dasgupta, M. Maitre, B. Kalra, and T. Gupta; manuscript writing: A. Dasgupta prepared the initial draft, T. Gupta edited the final draft manuscript; final approval of manuscript: all authors. All the authors are in agreement and accountable for all aspects of the work.
Corresponding author
Ethics declarations
Conflict of interest
A. Dasgupta, T. Gupta, M. Maitre, B. Kalra, A. Chatterjee, R. Krishnatry, J. Sastri Goda, N. Shirsat, S. Epari, A. Sahay, A. Janu, S. Pungavkar, G. Chinnaswamy, V. Patil, A. Moiyadi, P. Shetty, and R. Jalali declare that they have no competing interests.
Additional information
Presentation
Presented in part at the 12th Virtual Annual Conference of the Indian Society of Neuro-Oncology (ISNOCON-2021) hosted by Christian Medical College, Vellore, India, in April 2021.
Availability of data and material
Data will be made available on request to the corresponding author following institutional ethics committee protocols.
Supplementary Information
66_2021_1889_MOESM5_ESM.tif
Figure S5: Kaplan–Meier curves of relapse-free survival (a) and overall survival (b) stratified by molecular subgrouping in medulloblastoma
66_2021_1889_MOESM6_ESM.tif
Figure S6: Kaplan–Meier curves demonstrating the prognostic impact of semantic MRI features—tumor location on the vertical axis (a), brainstem involvement (b), proportion of solid tumor with contrast uptake (c), pattern of contrast enhancement (d), necrosis (e), and calcification (f) on relapse-free survival in medulloblastoma
Rights and permissions
About this article
Cite this article
Dasgupta, A., Gupta, T., Maitre, M. et al. Prognostic impact of semantic MRI features on survival outcomes in molecularly subtyped medulloblastoma. Strahlenther Onkol 198, 291–303 (2022). https://doi.org/10.1007/s00066-021-01889-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00066-021-01889-9