Abstract
Purpose
In this retrospective study, we have explored the anatomical factors that lead to the development of radiation necrosis (RN) in the setting of stereotactic radiosurgery (SRS) for melanoma brain metastases (MBM).
Methods
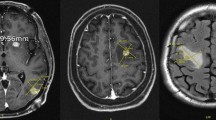
Between 2014 and 2018, 137 patients underwent SRS for 311 MBM. Lesions were assessed according to anatomical zones: zone 1—peripheral grey-white matter junction and cortical mantle, zone 2—deep white matter, including tumours located at base of sulci, zone 3—tumours adjacent to ependymal lining or in deep locations such as brainstem, basal ganglia and thalamus. Other anatomical factors including lobes, medial-peripheral, supra or infratentorial locations were also recorded.
Results
In all, 12.4% (n = 17) of patients and 6.1% (n = 20) of lesions developed RN, actuarial incidence of RN at 12 and 24 months was 10% and 14.2% respectively. Zone 2 lesions recorded the highest rate of development of RN (n = 7/19; 36%), zone 3 (N = 4/24; 16%) and zone 1 (n = 9/268; 3%). Five of 17 patients developed symptomatic RN and 7/17 patients underwent surgery for RN.
Conclusion
This study raises awareness of the increased likelihood of deep lesions particularly in white matter structures to develop RN after SRS. Further studies including larger cohorts would be useful in identifying statistical differences in the rate of development of RN in different anatomical zones.



Similar content being viewed by others
References
Tio M et al (2018) Survival and prognostic factors for patients with melanoma brain metastases in the era of modern systemic therapy. Pigment Cell Melanoma Res 31(4):509–515
Larkin J et al (2019) Five-year survival with combined nivolumab and ipilimumab in advanced melanoma. N Engl J Med 381(16):1535–1546
Tawbi HA et al (2018) Combined nivolumab and Ipilimumab in melanoma metastatic to the brain. N Engl J Med 379(8):722–730
Long GV et al (2018) Combination nivolumab and ipilimumab or nivolumab alone in melanoma brain metastases: a multicentre randomised phase 2 study. Lancet Oncol 19(5):672–681
Fang P et al (2017) Radiation necrosis with stereotactic radiosurgery combined with CTLA‑4 blockade and PD‑1 inhibition for treatment of intracranial disease in metastatic melanoma. J Neurooncol 133(3):595–602
Greene-Schloesser D et al (2012) Radiation-induced brain injury: a review. Front Oncol 2:73
Sneed PK et al (2015) Adverse radiation effect after stereotactic radiosurgery for brain metastases: incidence, time course, and risk factors. J Neurosurg 123(2):373–386
Kaidar-Person O et al (2017) The incidence of radiation necrosis following stereotactic radiotherapy for melanoma brain metastases: the potential impact of immunotherapy. Anticancer Drugs 28(6):669–675
Minniti G et al (2019) Stereotactic radiosurgery combined with nivolumab or Ipilimumab for patients with melanoma brain metastases: evaluation of brain control and toxicity. J Immunother Cancer 7(1):102
Pires da Silva I et al (2019) Incidence, features and management of radionecrosis in melanoma patients treated with cerebral radiotherapy and anti-PD‑1 antibodies. Pigment Cell Melanoma Res 32(4):553–563
Kotecha R et al (2018) Melanoma brain metastasis: the impact of stereotactic radiosurgery, BRAF mutational status, and targeted and/or immune-based therapies on treatment outcome. J Neurosurg 129(1):50–59
Sheline GE, Wara WM, Smith V (1980) Therapeutic irradiation and brain injury. Int J Radiat Oncol Biol Phys 6(9):1215–1228
Tsuruda JS et al (1987) Radiation effects on cerebral white matter: MR evaluation. AJR Am J Roentgenol 149(1):165–171
Kudo S et al (2014) Comparison of the radiosensitivities of neurons and glial cells derived from the same rat brain. Exp Ther Med 8(3):754–758
Furuse M et al (2015) Delayed brain radiation necrosis: pathological review and new molecular targets for treatment. Med Mol Morphol 48(4):183–190
Walker AJ et al (2014) Postradiation imaging changes in the CNS: how can we differentiate between treatment effect and disease progression? Future Oncol 10(7):1277–1297
Kohutek ZA et al (2015) Long-term risk of radionecrosis and imaging changes after stereotactic radiosurgery for brain metastases. J Neurooncol 125(1):149–156
Lohmann P et al (2018) Combined FET PET/MRI radiomics differentiates radiation injury from recurrent brain metastasis. Neuroimage Clin 20:537–542
Mitsuya K et al (2010) Perfusion weighted magnetic resonance imaging to distinguish the recurrence of metastatic brain tumors from radiation necrosis after stereotactic radiosurgery. J Neurooncol 99(1):81–88
Ohtakara K et al (2012) Significance of target location relative to the depth from the brain surface and high-dose irradiated volume in the development of brain radionecrosis after micromultileaf collimator-based stereotactic radiosurgery for brain metastases. J Neurooncol 108(1):201–209
Korytko T et al (2006) 12 Gy gamma knife radiosurgical volume is a predictor for radiation necrosis in non-AVM intracranial tumors. Int J Radiat Oncol Biol Phys 64(2):419–424
Minniti G et al (2011) Stereotactic radiosurgery for brain metastases: analysis of outcome and risk of brain radionecrosis. Radiat Oncol 6:48
Patel KR et al (2016) BRAF inhibitor and stereotactic radiosurgery is associated with an increased risk of radiation necrosis. Melanoma Res 26(4):387–394
Miller JA et al (2016) Association between radiation necrosis and tumor biology after stereotactic radiosurgery for brain metastasis. Int J Radiat Oncol Biol Phys 96(5):1060–1069
Martin AM et al (2018) Immunotherapy and symptomatic radiation necrosis in patients with brain metastases treated with stereotactic radiation. JAMA Oncol 4(8):1123–1124
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
S. Choi, A. Hong, T. Wang, S. Lo, B. Chen, I. Silva, R. Kapoor, E. Hsiao, G. B. Fogarty, M. S. Carlino, A. M. Menzies, G. V. Long and B. S. Shivalingam declare that they have no competing interests. We confirm that this manuscript is original and is not being considered for publication elsewhere. All figures and tables in this manuscript have been created by the authors of this manuscript.
Ethical standards
All procedures performed in studies involving human participants or on human tissue were in accordance with the ethical standards of the institutional (granted by the Melanoma Institute of Australia) and/or national research committee and with the 1975 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Choi, S., Hong, A., Wang, T. et al. Risk of radiation necrosis after stereotactic radiosurgery for melanoma brain metastasis by anatomical location. Strahlenther Onkol 197, 1104–1112 (2021). https://doi.org/10.1007/s00066-021-01798-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00066-021-01798-x