Abstract
Purpose
By increasing lung volume and decreasing respiration-induced tumour motion amplitude, administration of continuous positive airway pressure (CPAP) during stereotactic ablative radiotherapy (SABR) could allow for better sparing of the lungs and heart. In this study, we evaluated the effect of CPAP on lung volume, tumour motion amplitude and baseline shift, as well as the dosimetric impact of the strategy.
Methods
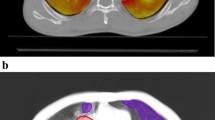
Twenty patients with lung tumours referred for SABR underwent 4D-computed tomography (CT) scans with and without CPAP (CPAP/noCPAP) at two timepoints (T0/T1). First, CPAP and noCPAP scans were compared for lung volume, tumour motion amplitude, and baseline shift. Next, CPAP and noCPAP treatment plans were computed and compared for lung dose parameters (mean lung dose (MLD), lung volume receiving 20 Gy (V20Gy), 13 Gy (V13Gy), and 5 Gy (V5Gy)) and mean heart dose (MHD).
Results
On average, CPAP increased lung volume by 8.0% (p < 0.001) and 6.3% (p < 0.001) at T0 and T1, respectively, but did not change tumour motion amplitude or baseline shift. As a result, CPAP administration led to an absolute decrease in MLD, lung V20Gy, V13Gy and V5Gy of 0.1 Gy (p = 0.1), 0.4% (p = 0.03), 0.5% (p = 0.04) and 0.5% (p = 0.2), respectively, while having no significant influence on MHD.
Conclusions
In patients referred for SABR for lung tumours, CPAP increased lung volume without modifying tumour motion or baseline shift. As a result, CPAP allowed for a slight decrease in radiation dose to the lungs, which is unlikely to be clinically significant.
Zusammenfassung
Zielsetzung
Aus der Erhöhung des Lungenvolumens und der Verringerung der atembedingten Tumorbewegungsamplitude beim Einsatz des kontinuierlichen positiven Atemwegsdrucks (CPAP „continuous positive airway pressure“) während der stereotaktischen ablativen Strahlentherapie (SABR „stereotactic ablative radiotherapy“) könnte ein erhöhter Schutz von Lunge und Herz resultieren. Diese Studie untersucht die Auswirkung der CPAP auf Lungenvolumen, Tumorbewegungsamplitude und „baseline shift“ sowie deren Einfluss auf die Dosisverteilung.
Methoden
Von 20 Patienten mit Lungentumoren, für die eine SABR indiziert ist, wurden zu zwei verschiedenen Zeitpunkten (T0/T1) 4‑D-Computertomographie-(CT-)Aufnahmen mit und ohne CPAP (CPAP/noCPAP) angefertigt. Zuerst wurden die CPAP- und noCPAP-Aufnahmen hinsichtlich Lungenvolumen, Tumorbewegungsamplitude und „baseline shift“ verglichen. Anschließend wurden CPAP- und noCPAP-Bestrahlungspläne erstellt und bezüglich der Dosisverteilung auf Herz und Lunge gegenübergestellt.
Ergebnisse
Im Durchschnitt vergrößerte CPAP das Lungenvolumen zu T0 und T1 um 8% (p < 0,001) bzw. 6,3% (p < 0,001), ohne Tumorbewegungsamplitude und „baseline shift“ zu verändern. Im Ergebnis verringerte die CPAP die mittlere Strahlendosis auf die Lunge um 0,1 Gy (p = 0,1) und die Volumenparameter V20Gy, V13Gy und V5Gy jeweils um 0,4% (p = 0,03), 0,5% (p = 0,04) und 0,5% (p = 0,2), ohne die Strahlendosis auf das Herz zu beeinflussen.
Schlussfolgerung
Bei Patienten, deren Lungentumor einer SABR unterzogen wurde, vergrößerte die CPAP das Lungenvolumen, ohne die Tumorbewegungsamplitude oder den „baseline shift“ zu beeinflussen. Infolgedessen wurde die Strahlendosis auf die Lunge leicht verringert, deren klinische Relevanz ist jedoch unwahrscheinlich.


Similar content being viewed by others
References
Vansteenkiste J, De Ruysscher D, Eberhardt WE et al (2013) Early and locally advanced non-small-cell lung cancer (NSCLC): ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol 24(Suppl 6):vi89–vi98
Verstegen NE, Lagerwaard FJ, Hashemi SM et al (2015) Patterns of disease recurrence after SABR for early stage non-small-cell lung cancer: optimizing follow-up schedules for salvage therapy. J Thorac Oncol 10:1195–1200
Goossens S, Senny F, Lee JA et al (2014) Assessment of tumor motion reproducibility with audio-visual coaching through successive 4D CT sessions. J Appl Clin Med Phys 15:4332
Kwint M, Conijn S, Schaake E et al (2014) Intra thoracic anatomical changes in lung cancer patients during the course of radiotherapy. Radiother Oncol 113:392–397
Goldstein JD, Lawrence YR, Appel S et al (2015) Continuous positive airway pressure for motion management in stereotactic body radiation therapy to the lung: a controlled pilot study. Int J Radiat Oncol Biol Phys 93:391–399
Janssens G, Jacques L, Orban de Xivry J et al (2011) Diffeomorphic registration of images with variable contrast enhancement. Int J Biomed Imaging 2011:891585
Wanet M, Sterpin E, Janssens G et al (2014) Validation of the mid-position strategy for lung tumors in helical TomoTherapy. Radiother Oncol 110:529–537
van Herk M, Remeijer P, Rasch C et al (2000) The probability of correct target dosage: dose-population histograms for deriving treatment margins in radiotherapy. Int J Radiat Oncol Biol Phys 47:1121–1135
Bissonnette JP, Franks KN, Purdie TG et al (2009) Quantifying interfraction and intrafraction tumor motion in lung stereotactic body radiotherapy using respiration-correlated cone beam computed tomography. Int J Radiat Oncol Biol Phys 75:688–695
Sonke JJ, Lebesque J, van Herk M (2008) Variability of four-dimensional computed tomography patient models. Int J Radiat Oncol Biol Phys 70:590–598
Wolthaus JW, Schneider C, Sonke JJ et al (2006) Mid-ventilation CT scan construction from four-dimensional respiration-correlated CT scans for radiotherapy planning of lung cancer patients. Int J Radiat Oncol Biol Phys 65:1560–1571
Wolthaus JW, Sonke JJ, van Herk M et al (2008) Comparison of different strategies to use four-dimensional computed tomography in treatment planning for lung cancer patients. Int J Radiat Oncol Biol Phys 70:1229–1238
Paddick I (2000) A simple scoring ratio to index the conformity of radiosurgical treatment plans. Technical note. J Neurosurg 93(Suppl 3):219–222
Parkes MJ, Green S, Stevens AM et al (2016) Reducing the within-patient variability of breathing for radiotherapy delivery in conscious, unsedated cancer patients using a mechanical ventilator. Br J Radiol 89:20150741
Fritz P, Kraus HJ, Dolken W et al (2006) Technical note: gold marker implants and high-frequency jet ventilation for stereotactic, single-dose irradiation of liver tumors. Technol Cancer Res Treat 5:9–14
Fritz P, Kraus HJ, Muhlnickel W et al (2010) High-frequency jet ventilation for complete target immobilization and reduction of planning target volume in stereotactic high single-dose irradiation of stage I non-small cell lung cancer and lung metastases. Int J Radiat Oncol Biol Phys 78:136–142
Peguret N, Ozsahin M, Zeverino M et al (2016) Apnea-like suppression of respiratory motion: first evaluation in radiotherapy. Radiother Oncol 118:220–226
Santiago A, Jelen U, Ammazzalorso F et al (2013) Reproducibility of target coverage in stereotactic spot scanning proton lung irradiation under high frequency jet ventilation. Radiother Oncol 109:45–50
Prior JO, Peguret N, Pomoni A et al (2016) Reduction of respiratory motion during PET/CT by pulsatile-flow ventilation: a first clinical evaluation. J Nucl Med 57:416–419
Acknowledgements
We would like to thank Valérie Lacroix who provided the original idea for this article and Karolin Schneider who translated the abstract into German.
Funding
This study was funded by the Fonds de la Recherche Scientifique—FNRS—Télévie (grant n°7.4572.13F) and the Fondation Contre le Cancer (grant n°2014-086).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
D. Di Perri, A. Colot, A. Delor, R. Ghoul, G. Janssens, V Lacroix, P. Matte, A. Robert, K. Souris and X. Geets declare that they have no competing interests.
Ethical standards
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee (registration number of the ethical approval: B403201524475) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Di Perri, D., Colot, A., Delor, A. et al. Effect of continuous positive airway pressure administration during lung stereotactic ablative radiotherapy: a comparative planning study. Strahlenther Onkol 194, 591–599 (2018). https://doi.org/10.1007/s00066-018-1278-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00066-018-1278-2