Abstract
Background
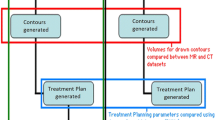
The present work aimed to analyze the feasibility of a shuttle-based MRI-guided radiation therapy (MRgRT) in the treatment of pelvic malignancies.
Patients and methods
20 patients with pelvic malignancies were included in this prospective feasibility analysis. Patients underwent daily MRI in treatment position prior to radiotherapy at the German Cancer Research Center. Positional inaccuracies, time and patient compliance were assessed for the application of off-line MRgRT.
Results
In 78% of applied radiation fractions, MR imaging for position verification could be performed without problems. Additionally, treatment-related side effects and reduced patient compliance were only responsible for omission of MRI in 9% of radiation fractions. The study workflow took a median time of 61 min (range 47–99 min); duration for radiotherapy alone was 13 min (range 7–26 min). Patient positioning, MR imaging and CT imaging including patient repositioning and the shuttle transfer required median times of 10 min (range 7–14 min), 26 min (range 15–60 min), 5 min (range 3–8 min) and 8 min (range 2–36 min), respectively.
To assess feasibility of shuttle-based MRgRT, the reference point coordinates for the x, y and z axis were determined for the MR images and CT obtained prior to the first treatment fraction and correlated with the coordinates of the planning CT. In our dataset, the median positional difference between MR imaging and CT-based imaging based on fiducial matching between MR and CT imaging was equal to or less than 2 mm in all spatial directions. The limited space in the MR scanner influenced patient selection, as the bore of the scanner had to accommodate the immobilization device and the constructed stereotactic frame. Therefore, obese, extremely muscular or very tall patients could not be included in this trial in addition to patients for whom exposure to MRI was generally judged inappropriate.
Conclusion
This trial demonstrated for the first time the feasibility and patient compliance of a shuttle-based off-line approach to MRgRT of pelvic malignancies.
Zusammenfassung
Hintergrund
Diese Arbeit analysiert die Machbarkeit einer MR-geführten Radiotherapie (MRgRT) im Beckenbereich mittels Shuttlesystem.
Patienten und Methoden
20 Patienten mit Tumorerkrankungen im Beckenbereich wurden in diese prospektive Machbarkeitsstudie eingeschlossen. Alle Patienten erhielten am Deutschen Krebsforschungszentrum Heidelberg jeweils vor Bestrahlung eine tägliche MRT-Bildgebung in Behandlungsposition. Lageungenauigkeiten, Zeitaufwand und Patientenakzeptanz dieses Offline-MRgRT-Ansatzes wurden erfasst.
Ergebnisse
Bei insgesamt 78 % der Bestrahlungsfraktionen konnte eine MRT-Bildgebung zur Lageverifikation der Patienten problemlos durchgeführt werden. Nur bei 9 % der Bestrahlungsfraktionen führten behandlungsbedingte Nebenwirkungen und eingeschränkte Patientenakzeptanz zum Ausfall der MRT-Scans. Der Zeitaufwand für diesen Offline-MRgRT-Ansatz betrug im Median 61 min (Spanne 47–99 min), davon 13 min für die Bestrahlung (Spanne 7–26 min). Patientenlagerung, MRT-Bildgebung, Cone-Beam-CT-Bildgebung und Transfer beanspruchten nacheinander im Median 10 min (Spanne 7–14 min), 26 min (Spanne 15–60 min), 5 min (Spanne 3–8 min) und 8 min (Spanne 2–36 min). Um die Anwendbarkeit der shuttlebasierten MRgRT zu überprüfen, wurden die Koordinaten des Referenzpunkts auf der MRT- und CT-Bildgebung zu Beginn der Radiotherapie erfasst und mit den Koordinaten der Planungs-CT korreliert. In dieser Studie war die nach Korrelation der Positionsmarker gemessene mediane Lageabweichung zwischen MRT- und Cone-Beam-CT-Bildgebung in allen Raumrichtungen maximal 2 mm. Die Platzvorgaben des MRT-Scanners beeinflussten in dieser Studie die Patientenauswahl dadurch, dass die „Gantry“ sowohl die Immobilisationshilfe als auch den stereotaktischen Rahmen fassen musste. Dadurch konnten adipöse, sehr muskulöse oder sehr große Patienten sowie Patienten mit Kontraindikationen für eine MRT-Untersuchung nicht in diese Studie eingeschlossen werden.
Schlussfolgerung
Diese Studie zeigte zum ersten Mal die Machbarkeit und Patientenakzeptanz eines shuttlebasierten Offline-Konzepts für die MRgRT pelviner Tumore.


Similar content being viewed by others
References
Guerrero Urbano MT, Nutting CM (2004) Clinical use of intensity-modulated radiotherapy: part II. Br J Radiol 77(915):177–182
Guckenberger M, Andratschke N, Alheit H, Holy R, Moustakis C, Nestle U, Sauer O, Deutsche Gesellschaft fur Radioonkologie (2014) Definition of stereotactic body radiotherapy: principles and practice for the treatment of stage I non-small cell lung cancer. Strahlenther Onkol 190(1):26–33
Schulz-Ertner D, Tsujii H (2007) Particle radiation therapy using proton and heavier ion beams. J Clin Oncol 25(8):953–964
Dawson LA, Jaffray DA (2007) Advances in image-guided radiation therapy. J Clin Oncol 25(8):938–946
Dawson LA, Sharpe MB (2006) Image-guided radiotherapy: rationale, benefits, and limitations. Lancet Oncol 7(10):848–858
Antonuk LE, Boudry J, Huang W, McShan DL, Morton EJ, Yorkston J, Longo MJ, Street RA (1992) Demonstration of megavoltage and diagnostic x‑ray imaging with hydrogenated amorphous silicon arrays. Med Phys 19(6):1455–1466
Jaffray DA, Siewerdsen JH, Wong JW, Martinez AA (2002) Flat-panel cone-beam computed tomography for image-guided radiation therapy. Int J Radiat Oncol Biol Phys 53(5):1337–1349
Rasch C, Steenbakkers R, van Herk M (2005) Target definition in prostate, head, and neck. Semin Radiat Oncol 15(3):136–145
Fiorentino A, Caivano R, Pedicini P, Fusco V (2013) Clinical target volume definition for glioblastoma radiotherapy planning: magnetic resonance imaging and computed tomography. Clin Transl Oncol 15(9):754–758
Thorwarth D (2015) Functional imaging for radiotherapy treatment planning: current status and future directions—a review. Br J Radiol 88(1051):20150056. https://doi.org/10.1259/bjr.20150056
Tsien C, Cao Y, Chenevert T (2014) Clinical applications for diffusion magnetic resonance imaging in radiotherapy. Semin Radiat Oncol 24(3):218–226
Lupo JM, Nelson SJ (2014) Advanced magnetic resonance imaging methods for planning and monitoring radiation therapy in patients with high-grade glioma. Semin Radiat Oncol 24(4):248–258
Dirix P, Haustermans K, Vandecaveye V (2014) The value of magnetic resonance imaging for radiotherapy planning. Semin Radiat Oncol 24(3):151–159
Kerkhof EM, Raaymakers BW, van der Heide UA, van de Bunt L, Jurgenliemk-Schulz IM, Lagendijk JJ (2008) Online MRI guidance for healthy tissue sparing in patients with cervical cancer: an IMRT planning study. Radiother Oncol 88(2):241–249
Chen L, Price RA Jr., Wang L, Li J, Qin L, McNeeley S, Ma CM, Freedman GM, Pollack A (2004) MRI-based treatment planning for radiotherapy: dosimetric verification for prostate IMRT. Int J Radiat Oncol Biol Phys 60(2):636–647
Beavis AW, Gibbs P, Dealey RA, Whitton VJ (1998) Radiotherapy treatment planning of brain tumours using MRI alone. Br J Radiol 71(845):544–548
Mutic S, Dempsey JF (2014) The ViewRay system: magnetic resonance-guided and controlled radiotherapy. Semin Radiat Oncol 24(3):196–199
Raaymakers BW, Lagendijk JJ, Overweg J, Kok JG, Raaijmakers AJ, Kerkhof EM, van der Put RW, Meijsing I, Crijns SP, Benedosso F et al (2009) Integrating a 1.5 T MRI scanner with a 6 MV accelerator: proof of concept. Phys Med Biol 54(12):N229–N237
Karlsson M, Karlsson MG, Nyholm T, Amies C, Zackrisson B (2009) Dedicated magnetic resonance imaging in the radiotherapy clinic. Int J Radiat Oncol Biol Phys 74(2):644–651
Jaffray DA, Carlone MC, Milosevic MF, Breen SL, Stanescu T, Rink A, Alasti H, Simeonov A, Sweitzer MC, Winter JD (2014) A facility for magnetic resonance-guided radiation therapy. Semin Radiat Oncol 24(3):193–195
Bostel T, Nicolay NH, Grossmann JG, Mohr A, Delorme S, Echner G, Haring P, Debus J, Sterzing F (2014) MR-guidance—a clinical study to evaluate a shuttle- based MR-linac connection to provide MR-guided radiotherapy. Radiat Oncol 9:12
Noel CE, Parikh PJ, Spencer CR, Green OL, Hu Y, Mutic S, Olsen JR (2015) Comparison of onboard low-field magnetic resonance imaging versus onboard computed tomography for anatomy visualization in radiotherapy. Acta Oncol 54(9):1474–1482
Acharya S, Fischer-Valuck BW, Kashani R, Parikh P, Yang D, Zhao T, Green O, Wooten O, Li HH, Hu Y et al (2016) Online magnetic resonance image guided adaptive radiation therapy: first clinical applications. Int J Radiat Oncol Biol Phys 94(2):394–403
Nyholm T, Nyberg M, Karlsson MG, Karlsson M (2009) Systematisation of spatial uncertainties for comparison between a MR and a CT-based radiotherapy workflow for prostate treatments. Radiat Oncol 4:54
Lagendijk JJ, Raaymakers BW, Raaijmakers AJ, Overweg J, Brown KJ, Kerkhof EM, van der Put RW, Hardemark B, van Vulpen M, van der Heide UA (2008) MRI/linac integration. Radiother Oncol 86(1):25–29
Constantin DE, Fahrig R, Keall PJ (2011) A study of the effect of in-line and perpendicular magnetic fields on beam characteristics of electron guns in medical linear accelerators. Med Phys 38(7):4174–4185
Fallone BG, Murray B, Rathee S, Stanescu T, Steciw S, Vidakovic S, Blosser E, Tymofichuk D (2009) First MR images obtained during megavoltage photon irradiation from a prototype integrated linac-MR system. Med Phys 36(6):2084–2088
Kron T, Eyles D, John SL, Battista J (2006) Magnetic resonance imaging for adaptive cobalt tomotherapy: a proposal. J Med Phys 31(4):242–254
Ghilezan MJ, Jaffray DA, Siewerdsen JH, Van Herk M, Shetty A, Sharpe MB, Zafar Jafri S, Vicini FA, Matter RC, Brabbins DS et al (2005) Prostate gland motion assessed with cine-magnetic resonance imaging (cine-MRI). Int J Radiat Oncol Biol Phys 62(2):406–417
Kotte AN, Hofman P, Lagendijk JJ, van Vulpen M, van der Heide UA (2007) Intrafraction motion of the prostate during external-beam radiation therapy: analysis of 427 patients with implanted fiducial markers. Int J Radiat Oncol Biol Phys 69(2):419–425
Roberson PL, McLaughlin PW, Narayana V, Troyer S, Hixson GV, Kessler ML (2005) Use and uncertainties of mutual information for computed tomography/ magnetic resonance (CT/MR) registration post permanent implant of the prostate. Med Phys 32(2):473–482
Fransson A, Andreo P, Potter R (2001) Aspects of MR image distortions in radiotherapy treatment planning. Strahlenther Onkol 177(2):59–73
Karger CP, Hoss A, Bendl R, Canda V, Schad L (2006) Accuracy of device-specific 2D and 3D image distortion correction algorithms for magnetic resonance imaging of the head provided by a manufacturer. Phys Med Biol 51(12):N253–N261
Rudra S, Jiang N, Rosenberg SA, Olsen JR, Parikh PJ, Bassetti MF, Lee P (2017) High dose adaptive MRI guided radiation therapy improves overall survival of inoperable pancreatic cancer. Int J Radiat Oncol Biol Phys 99(2, Suppl.):E184
Acknowledgements
We acknowledge the help of Rolf Bendl and Paul Mercea regarding the development of the hardware required for this trial. We also thank Annette Miltner, Marion Bachmann, Elisabeth Rittinghausen, Armin Runz and René Hertel for their excellent technical support.
Funding
This project was in part funded by a research grant of the German Federal Ministry of Education and Research (BMBF).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
T. Bostel, A. Pfaffenberger, S. Delorme, C. Dreher, G. Echner, P. Haering, C. Lang, M. Splinter, F. Laun, M. Müller, O. Jäkel, J. Debus, P.E. Huber, F. Sterzing and N.H. Nicolay declare that they have no competing interests.
Ethical standards
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Bostel, T., Pfaffenberger, A., Delorme, S. et al. Prospective feasibility analysis of a novel off-line approach for MR-guided radiotherapy. Strahlenther Onkol 194, 425–434 (2018). https://doi.org/10.1007/s00066-017-1258-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00066-017-1258-y