Abstract
Purpose
Radiotherapy (RT) in combination with chemoimmunotherapy is highly efficient in the treatment of diffuse large B‑cell lymphoma (DLBCL). This retrospective analysis evaluated the efficacy of the treatment volume and the dose concept of involved-site RT (ISRT).
Patients and methods
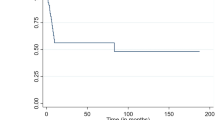
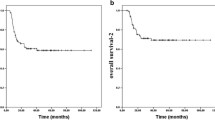
We identified 60 histologically confirmed stage I–IV DLBCL patients treated with multimodal cytotoxic chemoimmunotherapy and followed by consolidative ISRT from 2005–2015. Progression-free survival (PFS) and overall survival (OS) were estimated by Kaplan–Meier method. Univariate analyses were performed by log-rank test and Mann–Whitney U‑test.
Results
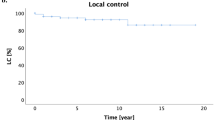
After initial chemoimmunotherapy (mostly R‑CHOP; rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisolone), 19 (36%) patients achieved complete response (CR), 34 (64%) partial response (PR) or less. Excluded were 7 (12%) patients with progressive disease after chemoimmunotherapy. All patients underwent ISRT with a dose of 40 Gy. After a median follow-up of 44 months, 79% of the patients remained disease free, while 21% presented with failure, progressive systemic disease, or death. All patients who achieved CR after chemoimmunotherapy remained in CR. Of the patients achieving PR after chemotherapy only 2 failed at the initial site within the ISRT volume. No marginal relapse was observed. Ann Arbor clinical stage I/II showed significantly improved PFS compared to stage III/IV (93% vs 65%; p ≤ 0.021). International Prognostic Index (IPI) score of 0 or 1 compared to 2–5 has been associated with significantly increased PFS (100% vs 70%; p ≤ 0.031). Postchemoimmunotherapy status of CR compared to PR was associated with significantly increased PFS (100% vs 68%; p ≤ 0.004) and OS (100% vs 82%; p ≤ 0.026). Only 3 of 53 patients developed grade II late side effects, whereas grade III or IV side effects have not been observed.
Conclusion
These data suggest that a reduction of the RT treatment volume from involved-field (IF) to involved-site (IS) is sufficient because no marginal failures occurred. The concept of IS will likely reduce the risk for late sequelae of RT.
Zusammenfassung
Einleitung
Die konsolidierende Radiotherapie (RT) in Kombination mit einer Chemoimmuntherapie stellt eine hocheffiziente Therapiemethode in der Behandlung des diffusen großzelligen B‑Zell-Lymphoms (DLBCL) dar. Die vorliegende retrospektive Analyse evaluiert die Effektivität und Sicherheit des Volumen- und Dosiskonzepts der „Involved-site“-Radiotherapie (ISRT).
Patienten und Methoden
Wir identifizierten 60 Patienten mit histologisch gesichertem DLBCL im Stadium I–IV, die zwischen Januar 2005 und Dezember 2015 mit einer Chemoimmuntherapie und konsolidierender ISRT behandelt wurden. Progressionsfreies (PFS) und Gesamtüberleben (OS) wurden mittels Kaplan-Meier-Methode dargestellt und univariate Analysen mittels Log-rank-Test und Mann-Whitney-U-Test erhoben.
Ergebnisse
Nach einer initialen Chemoimmuntherapie (überwiegend R‑CHOP; Rituximab, Cyclophosphamid, Doxorubicin, Vincristin und Prednisolon) erzielten 19 Patienten (36 %) eine komplette (CR) und 34 (64 %) eine partielle Remission (PR) oder weniger. Ausgeschlossen wurden 7 Patienten (12 %) mit einem Progress nach Chemoimmuntherapie. Alle Patienten erhielten eine ISRT mit 40 Gy Gesamtdosis. Nach einer medianen Nachbeobachtungszeit von 44 Monaten waren 79 % der Patienten erkrankungsfrei, während 21 % ein Rezidiv oder einen systemischen Progress erlitten oder verstarben. Alle Patienten mit CR nach Chemoimmuntherapie blieben nach konsolidierender ISRT in CR. Bei 2 Patienten mit PR nach Chemoimmuntherapie trat ein Rezidiv an Stelle der initialen Läsion innerhalb des IS-Planungszielvolumens (PTV) auf. Feldrandrezidive wurden nicht beobachtet. Ein signifikant verbessertes PFS zeigten ein Ann-Arbor-Stadium I/II im Vergleich zu Stadium III/IV (93 % vs. 65 %; p ≤ 0,021) sowie ein internationaler prognostischer Index (IPI) von 0 oder 1 verglichen mit 2–5 (100 % vs. 70 %; p ≤ 0,031). Der Post-Chemoimmuntherapie-Status einer CR war verglichen mit dem einer PR mit einem signifikant erhöhten PFS (100 % vs. 68 %; p ≤ 0,004) und OS (100 % vs. 82 %; p ≤ 0,026) assoziiert. Radiogene Spätfolgen Grad 2 entwickelten 3 von 53 Patienten, Grad 3 und 4 traten nicht auf.
Schlussfolgerung
Die Daten zeigen, dass eine PTV-Reduktion von „involved-field“ (IF) zu IS suffizient ist, weil keine Feldrandrezidive beobachtet wurden. Das ISRT-Konzept reduziert darüber hinaus das Risiko radiogener Spätfolgen.




Similar content being viewed by others
References
Bush RS, Gospodarowicz M, Sturgeon J, Alison R (1977) Radiation therapy of localized non-Hodgkin’s lymphoma. Cancer Treat Rep 61(6):1129–1136
Kaplan HS, Rosenberg SA (1966) The treatment of Hodgkin’s disease. Med Clin North Am 50(6):1591–1610
Lohr F, Georg D, Cozzi L et al (2014) Novel radiotherapy techniques for involved-field and involved-node treatment of mediastinal Hodgkin lymphoma: When should they be considered and which questions remain open? Strahlenther Onkol 190(10):864–866. doi:10.1007/s00066-014-0719-9 (868–871)
Kriz J, Spickermann M, Lehrich P et al (2015) Breath-hold technique in conventional APPA or intensity-modulated radiotherapy for Hodgkin’s lymphoma: comparison of ILROG IS-RT and the GHSG IF-RT. Strahlenther Onkol 191(9):717–725. doi:10.1007/s00066-015-0839-x
Girinsky T, van der Maazen R, Specht L et al (2006) Involved-node radiotherapy (INRT) in patients with early Hodgkin lymphoma: concepts and guidelines. Radiother Oncol 79(3):270–277. doi:10.1016/j.radonc.2006.05.015
Girinsky T, Ghalibafian M, Bonniaud G et al (2007) Is FDG-PET scan in patients with early stage Hodgkin lymphoma of any value in the implementation of the involved-node radiotherapy concept and dose painting? Radiother Oncol 85(2):178–186. doi:10.1016/j.radonc.2007.07.003
Girinsky T, Ghalibafian M (2007) Radiotherapy of hodgkin lymphoma: indications, new fields, and techniques. Semin Radiat Oncol 17(3):206–222. doi:10.1016/j.semradonc.2007.02.007
Girinsky T, Specht L, Ghalibafian M et al (2008) The conundrum of Hodgkin lymphoma nodes: to be or not to be included in the involved node radiation fields. The EORTC-GELA lymphoma group guidelines. Radiother Oncol 88(2):202–210. doi:10.1016/j.radonc.2008.05.012
Girinsky T, Aupérin A, Ribrag V et al (2014) Role of FDG-PET in the implementation of involved-node radiation therapy for Hodgkin lymphoma patients. Int J Radiat Oncol Biol Phys 89(5):1047–1052. doi:10.1016/j.ijrobp.2014.04.026
Illidge T, Specht L, Yahalom J et al (2014) Modern radiation therapy for nodal non-Hodgkin lymphoma-target definition and dose guidelines from the International Lymphoma Radiation Oncology Group. Int J Radiat Oncol Biol Phys 89(1):49–58. doi:10.1016/j.ijrobp.2014.01.006
NCCN (2017) Clinical practice guidelines in oncology. https://www.nccn.org/professionals/physician_gls/f_guidelines.asp. Accessed 25 Feb 2017
Kriz J, Baues C, Engenhart-Cabillic R et al (2017) New quality assurance program integrating “modern radiotherapy” within the German Hodgkin Study Group. Strahlenther Onkol 193(2):100–108. doi:10.1007/s00066-016-1048-y
Shi Z, Das S, Okwan-Duodu D et al (2013) Patterns of failure in advanced stage diffuse large B‑cell lymphoma patients after complete response to R‑CHOP immunochemotherapy and the emerging role of consolidative radiation therapy. Int J Radiat Oncol Biol Phys 86(3):569–577. doi:10.1016/j.ijrobp.2013.02.007
Dorth JA, Prosnitz LR, Broadwater G et al (2012) Impact of consolidation radiation therapy in stage III–IV diffuse large B‑cell lymphoma with negative post-chemotherapy radiologic imaging. Int J Radiat Oncol Biol Phys 84(3):762–767. doi:10.1016/j.ijrobp.2011.12.067
Ng AK, Dabaja BS, Hoppe RT, Illidge T, Yahalom J (2016) Re-examining the role of radiation therapy for diffuse large B‑cell lymphoma in the modern era. J Clin Oncol 34(13):1443–1447. doi:10.1200/jco.2015.64.9418
ClinicalTrials.gov (2016) Rituximab and combination chemotherapy with or without radiation therapy in treating patients with B‑cell non-Hodgkin’s Lymphoma – full text view. https://clinicaltrials.gov/ct2/show/study/NCT00278408?term=unfolder&rank=1. Accessed 28 Nov 2016
Carbone PP, Kaplan HS, Musshoff K, Smithers DW, Tubiana M (1971) Report of the committee on Hodgkin’s disease staging classification. Cancer Res 31(11):1860–1861
Cheson BD, Pfistner B, Juweid ME et al (2007) Revised response criteria for malignant lymphoma. J Clin Oncol 25(5):579–586. doi:10.1200/jco.2006.09.2403
Juweid ME, Stroobants S, Hoekstra OS et al (2007) Use of positron emission tomography for response assessment of lymphoma: consensus of the Imaging Subcommittee of International Harmonization Project in Lymphoma. J Clin Oncol 25(5):571–578. doi:10.1200/jco.2006.08.2305
CTEP (2016) Protocol development. http://ctep.cancer.gov/protocolDevelopment/electronic_applications/ctc.htm. Accessed 25 July 2016
Horning SJ, Weller E, Kim K et al (2004) Chemotherapy with or without radiotherapy in limited-stage diffuse aggressive non-Hodgkin’s lymphoma: Eastern Cooperative Oncology Group study 1484. J Clin Oncol 22(15):3032–3038. doi:10.1200/jco.2004.06.088
Miller TP, Dahlberg S, Cassady JR et al (1998) Chemotherapy alone compared with chemotherapy plus radiotherapy for localized intermediate- and high-grade non-Hodgkin’s lymphoma. N Engl J Med 339(1):21–26. doi:10.1056/nejm199807023390104
Phan J, Mazloom A, Medeiros LJ et al (2010) Benefit of consolidative radiation therapy in patients with diffuse large B‑cell lymphoma treated with R‑CHOP chemotherapy. J Clin Oncol 28(27):4170–4176. doi:10.1200/jco.2009.27.3441
Marcheselli L, Marcheselli R, Bari A et al (2011) Radiation therapy improves treatment outcome in patients with diffuse large B‑cell lymphoma. Leuk Lymphoma 52(10):1867–1872. doi:10.3109/10428194.2011.585526
Hu C, Deng C, Zou W, Zhang G, Wang J (2015) The role of consolidative radiotherapy after a complete response to chemotherapy in the treatment of diffuse large B‑cell lymphoma in the rituximab era: results from a systematic review with a meta-analysis. Acta Haematol 134(2):111–118. doi:10.1159/000370096
Kaplan HS (1980) Hodgkin’s disease: unfolding concepts concerning its nature, management and prognosis. Cancer 45(10):2439–2474
Fuks Z, Kaplan HS (1973) Recurrence rates following radiation therapy of nodular and diffuse malignant lymphomas. Radiology 108(3):675–684. doi:10.1148/108.3.675
Nickson JJ (1966) Hodgkin’s disease clinical trial. Cancer Res 26(6):1279–1283
Yahalom J, Mauch P (2002) The involved field is back: issues in delineating the radiation field in Hodgkin’s disease. Ann Oncol 1:79–83
Eich HT, Müller R‑P, Engenhart-Cabillic R et al (2008) Involved-node radiotherapy in early-stage Hodgkin’s lymphoma. Definition and guidelines of the German Hodgkin Study Group (GHSG). Strahlenther Onkol 184(8):406–410
Hoskin PJ, Díez P, Williams M, Lucraft H, Bayne M (2013) Participants of the lymphoma radiotherapy group. Recommendations for the use of radiotherapy in nodal lymphoma. Clin Oncol 25(1):49–58. doi:10.1016/j.clon.2012.07.011
Campbell BA, Connors JM, Gascoyne RD, Morris WJ, Pickles T, Sehn LH (2012) Limited-stage diffuse large B‑cell lymphoma treated with abbreviated systemic therapy and consolidation radiotherapy: involved-field versus involved-node radiotherapy. Cancer 118(17):4156–4165. doi:10.1002/cncr.26687
Verhappen MH, Poortmans PMP, Raaijmakers E, Raemaekers JMM (2013) Reduction of the treated volume to involved node radiation therapy as part of combined modality treatment for early stage aggressive non-Hodgkin’s lymphoma. Radiother Oncol 109(1):133–139. doi:10.1016/j.radonc.2013.07.013
Yu JI, Nam H, Ahn YC, Kim WS, Park K, Kim SJ (2010) Involved-lesion radiation therapy after chemotherapy in limited-stage head-and-neck diffuse large B cell lymphoma. Int J Radiat Oncol Biol Phys 78(2):507–512. doi:10.1016/j.ijrobp.2009.07.1706
Kwon J, Kim IH, Kim BH, Kim TM, Heo DS (2015) Additional survival benefit of involved-lesion radiation therapy after R‑CHOP chemotherapy in limited stage diffuse large B‑cell lymphoma. Int J Radiat Oncol Biol Phys 92(1):91–98. doi:10.1016/j.ijrobp.2014.12.042
Elstrom R, Guan L, Baker G et al (2003) Utility of FDG-PET scanning in lymphoma by WHO classification. Blood 101(10):3875–3876. doi:10.1182/blood-2002-09-2778
Isohashi K, Tatsumi M, Higuchi I et al (2008) 18F-FDG-PET in patients with malignant lymphoma having long-term follow-up: staging and restaging, and evaluation of treatment response and recurrence. Ann Nucl Med 22(9):795–802. doi:10.1007/s12149-008-0186-4
Lowry L, Smith P, Qian W et al (2011) Reduced dose radiotherapy for local control in non-Hodgkin lymphoma: a randomised phase III trial. Radiother Oncol 100(1):86–92. doi:10.1016/j.radonc.2011.05.013
Avilés A, Delgado S, Nambo MJ, Alatriste S, Díaz-Maqueo JC (1994) Adjuvant radiotherapy to sites of previous bulky disease in patients stage IV diffuse large cell lymphoma. Int J Radiat Oncol Biol Phys 30(4):799–803
Pfreundschuh M, Schubert J, Ziepert M et al (2008) Six versus eight cycles of bi-weekly CHOP-14 with or without rituximab in elderly patients with aggressive CD20+ B‑cell lymphomas: a randomised controlled trial (RICOVER-60). Lancet Oncol 9(2):105–116. doi:10.1016/s1470-2045(08)70002-0
Song M‑K, Chung J‑S, Sung-Yong O et al (2010) Clinical impact of bulky mass in the patient with primary extranodal diffuse large B cell lymphoma treated with R‑CHOP therapy. Ann Hematol 89(10):985–991. doi:10.1007/s00277-010-0964-7
Held G, Murawski N, Ziepert M et al (2014) Role of radiotherapy to bulky disease in elderly patients with aggressive B‑cell lymphoma. J Clin Oncol 32(11):1112–1118. doi:10.1200/jco.2013.51.4505
Jegadeesh N, Rajpara R, Esiashvili N et al (2015) Predictors of local recurrence after rituximab-based chemotherapy alone in stage III and IV diffuse large B‑cell lymphoma: guiding decisions for consolidative radiation. Int J Radiat Oncol Biol Phys 92(1):107–112. doi:10.1016/j.ijrobp.2015.01.025
Wilder RB, Tucker SL, Ha CS et al (2001) Dose-response analysis for radiotherapy delivered to patients with intermediate-grade and large-cell immunoblastic lymphomas that have completely responded to CHOP-based induction chemotherapy. Int J Radiat Oncol Biol Phys 49(1):17–22
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
E. Holzhäuser, M. Berlin, D. Wollschläger, T. Bezold, A. Mayer, G. Heß and H. Schmidberger declare that they have no competing interests.
Ethical standards
This article does not contain any studies with human participants or animals performed by any of the authors.
Rights and permissions
About this article
Cite this article
Holzhäuser, E., Berlin, M., Wollschläger, D. et al. Patterns of failure of diffuse large B‑cell lymphoma patients after involved-site radiotherapy. Strahlenther Onkol 193, 1014–1023 (2017). https://doi.org/10.1007/s00066-017-1186-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00066-017-1186-x