Abstract
Aim
The aim of this study was to investigate whether a safe escalation of the dose to the pleural cavity and PET/CT-positive areas in patients with unresectable malignant pleural mesothelioma (MPM) is possible using helical tomotherapy (HT).
Material and methods
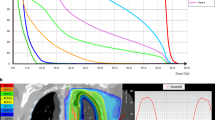
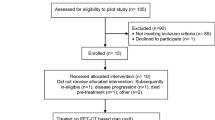
We selected 12 patients with MPM. Three planning strategies were investigated. In the first strategy (standard treatment), treated comprised a prescribed median dose to the planning target volume (PTV) boost (PTV1) of 64.5 Gy (range: 56 Gy/28 fractions to 66 Gy/30 fractions) and 51 Gy (range: 50.4 Gy/28 fractions to 54 Gy/30 fractions) to the pleura PTV (PTV2). Thereafter, for each patient, two dose escalation plans were generated prescribing 62.5 and 70 Gy (2.5 and 2.8 Gy/fraction, respectively) to the PTV1 and 56 Gy (2.24 Gy/fraction) to the PTV2, in 25 fractions. Dose–volume histogram (DVH) constraints and normal tissue complication probability (NTCP) calculations were used to evaluate the differences between the plans.
Results
For all plans, the 95 % PTVs received at least 95 % of the prescribed dose. For all patients, it was possible to perform the dose escalation in accordance with the Quantitative Analysis of Normal Tissue Effects in the Clinic (QUANTEC) constraints for organs at risk (OARs). The average contralateral lung dose was < 8 Gy. NTCP values for OARs did not increase significantly compared with the standard treatment (p > 0.05), except for the ipsilateral lung. For all plans, the lung volume ratio was strongly correlated with the V20, V30, and V40 DVHs of the lung (p < 0.0003) and with the lung mean dose (p < 0.0001).
Conclusion
The results of this study suggest that by using HT it is possible to safely escalate the dose delivery to at least 62.5 Gy in PET-positive areas while treating the pleural cavity to 56 Gy in 25 fractions without significantly increasing the dose to the surrounding normal organs.
Zusammenfassung
Ziel
Ziel war es, zu untersuchen, ob mit der helikalen Tomotherapie (HT) eine sichere Dosiseskalation auf die Pleurahöhle und PET/CT-positive Bereiche bei Patienten mit inoperablem malignem Pleuramesotheliom (MPM) möglich ist.
Material und Methoden
Zwölf Patienten mit MPM wurden ausgewählt und drei Planungsstrategien untersucht. Bei der ersten Strategie (Standardbehandlung) wurden die Patienten im einem PTV-Boost (PTV1, Planungszielvolumen) mit einer medianen Dosis von 64,5 Gy (Dosisbereich von 56 Gy/28 Fraktionen bis 66 Gy/30 Fraktionen) und 51 Gy im Pleura-PTV (PTV2) behandelt. Danach wurden für jeden Patienten zwei Dosiseskalationspläne mit der Verschreibung von 62,5 und 70 Gy (jeweils 2,5 und 2,8 Gy/Fraktion) im PTV1 und 56 Gy (2,24 Gy/Fraktion) im PTV2 in 25 Fraktionen generiert. Dosis-Volumen-Histogramme und die Wahrscheinlichkeit für Komplikationen am Normalgewebe (NTCP) wurden verwendet, um Unterschiede zwischen den Plänen zu bewerten.
Ergebnisse
Alle Pläne der 95 %-PTV erzielten zumindest 95 % der verschriebenen Dosis. Bei allen Patienten war es möglich, die Dosiseskalation durchzuführen, ohne die Toleranzdosisgrenzen für Risikoorgane (OARs) nach QUANTEC (Quantitative Analysis of Normal Tissue Effects in the Clinic) zu verletzen. Die durchschnittliche kontralaterale Lungendosis war < 8 Gy. Die NTCP-Werte der OARs erhöhten sich nicht bedeutsam und respektierten die Standardbehandlung (p > 0,05), mit Ausnahme der ipsilateralen Lunge. Bei allen Plänen war das Lungenvolumen stark mit den V20-, V30-, V40-Dosis-Volumen-Histogrammen (DVH; p < 0,0003) der Lunge und mit der mittleren Lungendosis (p < 0,0001) korreliert.
Schlussfolgerungen
Die Ergebnisse dieser Studie zeigen, dass unter Verwendung der HT die Dosiseskalation bis mindestens 62,5 Gy auf PET-positive Flächen gefahrlos möglich ist, während die Pleurahöhle mit bis zu 56 Gy in 25 Fraktionen behandelt werden kann, ohne die Dosis auf die umgebenden normalen Organe bedeutsam zu erhöhen.


Similar content being viewed by others
References
Fact sheet N343 World Health Organisation (2010) Asbestos: elimination of asbestos-related diseases. http://www.who.int/mediacentre/factsheets/fs343/en/index.html
Marinaccio A, Montanaro F, Mastrantonio M, Uccelli R, Altavista P, Nesti M, Costantini AS, Gorini G (2005) Predictions of mortality from pleural mesothelioma in Italy: a model based on asbestos consumption gures supports results from age-period-cohort models. Int J Cancer 114:142–147
Muers MF, Stephens RJ, Fisher P, Darlison L, Higgs CM, Lowry E et al (2008) Active symptom control with or without chemotherapy in the treatment of patients with malignant pleural mesothelioma (MS01): a multicentre randomised trial. Lancet 371:1685–1694
Gupta V, Mychalczak B, Krug L et al (2005) Hemithoracic radiation therapy after pleurectomy/decortications for malignant pleural mesothelioma. Int J Radiat Oncol Biol Phys 63:1045–1052
Boutin C, Rey F, Viallat JR (1995) Prevention of malignant seeding after invasive diagnostic procedures in patients with pleural mesothelioma. A randomized trial of local radiotherapy. Chest 108:754–758
Nakas A, Trousse DS, Martin-Ucar AE et al (2008) Open lung-sparing surgery for malignant pleural mesothelioma: the benefits of a radical approach within multimodality therapy. Eur J Card Thorac Surg 34:886–891
Batirel H, Metintas M, Caglar HB, Yildizeli B, Lacin T, Bostanci K, Akgul A, Evman S, Yuksel M (2008) Trimodality treatment of malignant pleural mesothelioma. J Thorac Oncol 3:499–504
Pagan V, Ceron L, Paccagnella A, Pizzi G (2006) 5-year prospective results of trimodality treatment for malignant pleural mesothelioma. J Cardiovasc Surg (Torino) 47:595–601
Stevens C, Rice D, Forster K et al (2005) Extrapleural pneumonectomy followed by IMRT: Results of a Phase I/II study. J Clin Oncol 23:7178
Sharif S, Zahid I, Routledge T, Scarci M (2011) Does positron emission tomography offer prognostic information in malignant pleural mesothelioma? Interact Cardiovasc Thorac Surg 12:806–811
Klabatsa A, Chicklore S, Barrington FS et al (2014) The association of 18F-FDG PET/CT parameters with survival in malignant pleural mesothelioma. Eur J Nucl Med Mol Imaging 41:276–282
Ung YC, Yu E, Falkson C et al (2006) The role of radiation therapy in malignant pleural mesothelioma: a systematic review. Radiother Oncol 80:13–18
Carmichael J, Degraff WG, Gamson J et al (1989) Radiation sensitivity of human lung cancer cell lines. Eur J Cancer Clin Oncol 25:3527–3534
(2010) Quantitative Analysis of Normal Tissue Effects in the Clinic (QUANTEC). Int J Radiat Oncol Biol Phys 76:S3–S9
Rice DC, Stevens CW, Correa AM et al (2007) Outcomes after extrapleural pneumonectomy and intensity-modulated radiation therapy for malignant pleural mesothelioma. Ann Thorac Surg 84:1685–1693
Allen AM, Czerminska M, Janne PA et al (2006) Fatal pneumonitis associated with intensity-modulated radiation therapy for mesothelioma. Int J Radiat Oncol Biol Phys 65:640–645
Kristensen CA, Nottrup TJ, Berthelsen AK et al (2009) Pulmonary toxicity following IMRT after extrapleural pneumonectomy for malignant pleural mesothelioma. Radiother Oncol 92:96–99
Patel P, Yoo S, Broadwater G et al (2012) Effect of increasing experience on dosimetric and clinical outcomes in the management of malignant pleural mesothelioma with intensity-modulated radiation therapy. Int J Radiation Oncol Biol Phys 83(1):362–368
McAleer M.F, Tsao A, Liao Z (2009) Radiotherapy in malignant pleural mesothelioma. Int J Radiation Oncology Biol Phys 75(2):326–337
Treasure T, Lang-Lazdunski L, Waller D et al (2011) Extra-pleural pneumonectomy versus no extra-pleural pneumonectomy for patients with malignant pleural mesothelioma: clinical outcomes of the Mesothelioma and Radical Surgery (MARS) randomised feasibility study. Lancet Oncol 12:763–772
Munter MW, Nill S, Thilmann C et al (2003) Stereotactic intensity modulated radiation therapy (IMRT) and inverse treatment planning for advanced pleural mesothelioma. Feasibility and initial results. Strahelenther Onkol 179:535–541
Fodor A, Fiorino C, Dell’Oca I et al (2011) PET-guided dose escalation tomotherapy in malignant pleural mesothelioma. Strahlenther Onkol 187:736–743
Abakay A, Komek H, Abakay O et al (2013) Relationship between 18 FDG PET-CT findings and the survival of 177 patients with malignant pleural mesothelioma. Eur Rev Med Pharmacol Sci 17:1233–1241
Baldini EH, Recht A, Strauss GM et al (1997) Patterns of failure after trimodality therapy for malignant pleural mesothelioma. Ann Thorac Surg 63:334–338
Stahel R, Weder W, Riesterer O et al (2014) Neoadjuvant chemotherapy and extrapleural pneumonectomy of malignant pleural mesothelioma (MPM) with or without hemithoracic radiotherapy: final results of the randomized multicenter phase II trial SAKK17/04. ESMO 2014 late breaking abstract
NCCN Guidelines Version 1 (2014) Malignant pleural mesothelioma
Yajnik S, Rosenzweig KE, Mychalczak B et al (2003) Hemithoracic radiation after extrapleural pneumonectomy for malignant pleural mesothelioma. Int J Radiat Oncol Biol Phys 56:1319–1326
Miles EF, Larrier NA, Kelsey CR et al (2008) Intensity-modulated radiotherapy for resected mesothelioma: the Duke experience. Int J Radiat Oncol Biol Phys 71:1143–1150
Sterzing F, Sroka-Perez G, Schubert K et al (2008) Evaluating target coverage and normal tissue sparing in the adjuvant radiotherapy of malignant pleural mesothelioma: helical tomotherapy compared with step-and-shoot IMRT. Radiother Oncol 86:251–257
Acknowledgements
This work was supported by “TOMO 2”—5 × Mille 2009 Ministero della Salute—FPRC onlus.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
A. Maggio, C. Cutaia, A. Di Dia, S. Bresciani, A. Miranti, M. Poli, E. Del Mastro, E. Garibaldi, P. Gabriele and M. Stasi state that there are no conflicts of interest.
All studies on humans described in the present manuscript were carried out with the approval of the responsible ethics committee and in accordance with national law and the Helsinki Declaration of 1975 (in its current, revised form). Informed consent was obtained from all patients included in studies.
Rights and permissions
About this article
Cite this article
Maggio, A., Cutaia, C., Di Dia, A. et al. Tomotherapy PET-guided dose escalation. Strahlenther Onkol 192, 102–108 (2016). https://doi.org/10.1007/s00066-015-0901-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00066-015-0901-8