Abstract
Background
Permanent low-dose-rate brachytherapy (BT) with iodine 125 is an established curative treatment for localized prostate cancer. After treatment, prostate-specific antigen (PSA) kinetics may show a transient rise (PSA bounce). Our aim was to investigate the association of PSA bounce with biochemical control.
Patients and methods
Patients treated with BT in Switzerland were registered in a prospective database. Only patients with a follow-up of at least 2 years were included in our analysis. Clinical follow-up and PSA measurements were assessed after 1.5, 3, 6, and 12 months, and annually thereafter. If PSA increased, additional follow-up visits were scheduled. Cases of PSA bounce were defined as a rise of at least 0.2 ng/ml above the initial PSA nadir with a subsequent decline to or below the initial nadir without treatment. Biochemical failure was defined as a rise to nadir + 2 ng/ml.
Results
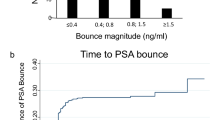
Between March 2001 and November 2010, 713 patients with prostate cancer undergoing BT with at least 2 years of follow-up were registered. Median follow-up time was 41 months. Biochemical failure occurred in 28 patients (3.9 %). PSA bounce occurred in 173 (24.3 %) patients; only three (1.7 %) patients with PSA bounce developed biochemical failure, in contrast to 25 (4.6 %) patients without previous bounce (p < 0.05). The median time to bounce was 12 months, the median time to biochemical failure was 30 months. The median bounce increase was 0.78 ng/ml. Twenty-eight patients with bounce (16.5 %) had a transient PSA rise of + 2 ng/ml above the nadir.
Conclusion
In most cases, an early increase in PSA after BT indicates PSA bounce and is associated with a lower risk of biochemical failure.
Zusammenfassung
Hintergrund
Die permanente Low-dose-rate-Brachytherapie (BT) mit 125I ist ein etabliertes kuratives Verfahren bei lokalisiertem Prostatakarzinom. Posttherapeutisch können die PSA-Konzentrationen einen vorübergehenden Anstieg zeigen (Bounce-Phänomen). Untersucht werden sollte ein möglicher Zusammenhang mit der biochemischen Kontrolle.
Methoden
Patienten, die eine BT in der Schweiz bekommen hatten, wurden in einer prospektiven Datenbank erfasst. Nur Patienten mit mindestens 2 Jahren Nachsorge wurden in die Studie eingeschlossen. Klinische Verlaufskontrollen mit PSA-Messungen erfolgten nach 1, 5, 3, 6 und 12 Monaten sowie anschließend jährlich. Bei einer PSA-Erhöhung wurden weitere Termine vereinbart. Der PSA-Bounce wurde definiert als ein Anstieg des PSA-Wertes um mindestens 0,2 ng/ml über den initialen PSA-Nadir mit anschließendem Absinken auf diesen Wert oder tiefer ohne Therapie. Biochemisches Versagen wurde definiert als Nadir+2ng/ml.
Ergebnis
Eingeschlossen wurden 713 Patienten, die zwischen 03/2001 und 11/2010 eine BT und mindestens 2 Jahre (mediane Nachsorgedauer 41 Monate) Nachsorge erhalten hatten. Ein biochemisches Versagen zeigte sich bei 28 Patienten (3,9 %). Bei 173 (24,3 %) Patienten konnte ein Bounce beobachtet werden, nur 3 (1,7 %) entwickelten anschließend ein biochemisches Versagen. Dagegen entwickelten 25 (4,6 %) Patienten ohne Bounce ein biochemisches Rezidiv (p < 0,05). Die mediane Zeit bis zum Bounce betrug 12 Monate, die mediane Zeit bis zum biochemischen Versagen 30. Der mediane PSA-Anstieg beim Bounce war 0,78 ng/ml. Achtundzwanzig Patienten (16,5%) mit einem Bounce hatten einen temporären PSA-Anstieg von + 2 ng/ml über den Nadir.
Fazit
In den meisten Fällen war ein früher PSA-Anstieg nach BT mit einem Bounce verbunden; dieser ist mit einem niedrigeren Risiko für ein biochemisches Rezidiv assoziiert.


Similar content being viewed by others
References
Badakhshi H, Graf R, Budach V, Wust P (2015) Permanent interstitial low-dose-rate brachytherapy for patients with low risk prostate cancer. Strahlenther Onkol 191:303–309
Yoshida K, Yamazaki H, Takenaka T, Kotsuma T, Yoshida M, Masui K, Yoshioka Y, Narumi Y, Oka T, Tanaka E (2014) High-dose-rate interstitial brachytherapy in combination with androgen deprivation therapy for prostate cancer. Strahlenther Onkol 190:1015–1020
Panje CM, dal Pra A, Zilli T, Zwahlen D, Papachristofilou A, Herrera FG, Matzinger O, Plasswilm L, Putora PM (2015) Consensus and differences in primary radiotherapy for localized and locally advanced prostate cancer in Switzerland. Strahlenther Onkol May 19. Epub ahead of print DOI 10.1007/s00066-015-0849-8
Schiffmann J, Lesmana H, Tennstedt P, Beyer B, Boehm K, Platz V, Tilki D, Salomon G, Petersen C, Krüll A, Graefen M, Schwarz R (2015) Additional androgen deprivation makes the difference: Biochemical recurrence-free survival in prostate cancer patients after HDR brachytherapy and external beam radiotherapy. Strahlenther Onkol 191:330–337
Kim Y-J, Cho KH, Pyo HR, Lee KH, Moon SH, Kim TH, Shin KH, Kim J-Y, Kim Y-k, Lee SB (2015) Radical prostatectomy versus external beam radiotherapy for localized prostate cancer. Strahlenther Onkol 191:321–329
Sensabaugh G, Crim D (1978) Isolation and characterization of a semen-specific protein from human seminal plasma: a potential new marker for semen identification. J Forensic Sci 23:106–115
Heidenreich A, Bellmunt J, Bolla M, Joniau S, Mason M, Matveev V, Mottet N, Schmid H-P, van der Kwast T, Wiegel T (2011) EAU guidelines on prostate cancer. Part 1: screening, diagnosis, and treatment of clinically localised disease. Eur Urol 59:61–71
Critz FA, Williams WH, Benton JB, Levinson AK, Holladay CT, Holladay DA (2000) Prostate specific antigen bounce after radioactive seed implantation followed by external beam radiation for prostate cancer. J Urol 163:1085–1089
Pinkawa M, Piroth MD, Holy R, Fischedick K, Schaar S, Borchers H, Heidenreich A, Eble MJ (2010) Prostate-specific antigen kinetics following external-beam radiotherapy and temporary (Ir-192) or permanent (I-125) brachytherapy for prostate cancer. Radiother Oncol 96:25–29
Ciezki JP, Reddy CA, Garcia J, Angermeier K, Ulchaker J, Mahadevan A, Chehade N, Altman A, Klein EA (2006) PSA kinetics after prostate brachytherapy: PSA bounce phenomenon and its implications for PSA doubling time. Int J Radiat Oncol Biol Phys 64:512–517
Patel C, Elshaikh MA, Angermeier K, Ulchaker J, Klein EA, Chehade N, Wilkinson DA, Reddy CA, Ciezki JP (2004) PSA bounce predicts early success in patients with permanent iodine-125 prostate implant. Urology 63:110–113
Hinnen KA, Monninkhof EM, Battermann JJ, van Roermund JG, Frank SJ, van Vulpen M (2012) Prostate specific antigen bounce is related to overall survival in prostate brachytherapy. Int J Radiat Oncol Biol Phys 82:883–888
Ko EC, Stone NN, Stock RG (2012) PSA nadir of < 0.5 ng/mL following brachytherapy for early-stage prostate adenocarcinoma is associated with freedom from prostate-specific antigen failure. Int J Radiat Oncol Biol Phys 83:600–607
Gaztañaga M, Crook J (2013) Interpreting a rising prostate‐specific antigen after brachytherapy for prostate cancer. Int J Urol 20:142–147
D’Amico AV, Whittington R, Malkowicz SB, Schultz D, Blank K, Broderick GA, Tomaszewski JE, Renshaw AA, Kaplan I, Beard CJ (1998) Biochemical outcome after radical prostatectomy, external beam radiation therapy, or interstitial radiation therapy for clinically localized prostate cancer. JAMA 280:969–974
Putora PM, Plasswilm L, Seelentag W, Schiefer J, Markart P, Schmid H-P, Engeler D (2013) Re-implantation after insufficient primary 125-i permanent prostate brachytherapy. Radiat Oncol 8:194
Rosser CJ, Kamat AM, Wang X, Do K-A, Sanchez-Ortiz RF, Kuban DA, Lee AK, Cheung R, Chichakli R, Pisters LL (2005) Is patient age a factor in the occurrence of prostate-specific antigen bounce phenomenon after external beam radiotherapy for prostate cancer? Urology 66:327–331
Tanaka N, Asakawa I, Fujimoto K, Anai S, Hirayama A, Hasegawa M, Konishi N, Hirao Y (2012) Minimal percentage of dose received by 90 % of the urethra (% UD90) is the most significant predictor of PSA bounce in patients who underwent low-dose-rate brachytherapy (LDR-brachytherapy) for prostate cancer. BMC Urol 12:28
Crook J, Gillan C, Yeung I, Austen L, McLean M, Lockwood G (2007) PSA kinetics and PSA bounce following permanent seed prostate brachytherapy. Int J Radiat Oncol Biol Phys 69:426–433
Cavanagh W, Blasko J, Grimm P, Sylvester J (2000) Transient elevation of serum prostate-specific antigen following (125) I/(103) Pd brachytherapy for localized prostate cancer. Semin Urolo Oncol 2:160–165
Morita M, Lederer J, Fukagai T, Shimada M, Yoshida H (2004) PSA bounce phenomenon after transperineal interstitial permanent prostate brachytherapy for localized prostate cancer. Nihon Hinyokika Gakkai Zasshi 95:609–615
Guarneri A, Botticella A, Ragona R, Filippi AR, Munoz F, Casetta G, Gontero P, Tizzani A, Ricardi U (2013) Prostate-specific antigen kinetics after I125-brachytherapy for prostate adenocarcinoma. World J Urol 31:411–415
Acknowledgments
The authors thank Alistair Reeves for editing the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
D.S. Engeler, C. Schwab, A.F. Thöni, W. Hochreiter, L. Prikler, S. Suter, P. Stucki, J. Schiefer, L. Plasswilm, H-P. Schmid, and P.M. Putora state that there are no conflicts of interest.
All studies on humans described in the present manuscript were carried out with the approval of the responsible ethics committee and in accordance with national law and the Helsinki Declaration of 1975 (in its current, revised form). Informed consent was obtained from all patients included in studies.
Rights and permissions
About this article
Cite this article
Engeler, D., Schwab, C., Thöni, A. et al. PSA bounce after 125I-brachytherapy for prostate cancer as a favorable prognosticator. Strahlenther Onkol 191, 787–791 (2015). https://doi.org/10.1007/s00066-015-0860-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00066-015-0860-0