Abstract
Purpose:
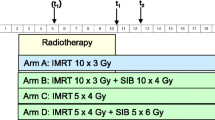
To perform aggressive radiotherapy for vertebral metastases. Using very steep dose gradients from intensity-modulated radiotherapy (IMRT), a protocol based on the concept of partial volume dose to the spinal cord was evaluated.
Patients and Methods:
50 patients with vertebral metastases were treated using IMRT. In previously unirradiated cases, where a prescribed dose of 80 Gy (BED10) was delivered, the constraint to the spinal cord should be less than 100 Gy (BED2). For previously irradiated cases, on the other hand, the dose is the same as in the previously unirradiated case; however, constraints for the spinal cord are a cumulative BED2 of less than 150 Gy, BED2 of less than 100 Gy in each instance, and a treatment gap of more than 6 months. There were 6 patients considered for a partial volume dose to the spinal cord. They all received higher BED2, ranging from 51–157 Gy of D1cc.
Results:
Among the 24 patients who survived longer than 1 year, there was 1 case of transient radiation myelitis. There were no other cases of spinal cord sequelae.
Conclusion:
Based on the present results, we recommend a BED2 of 100 Gy or less at D1cc as a constraint for the spinal cord in previously unirradiated cases, and a cumulative BED2 of 150 Gy or less at D1cc in previously irradiated cases, when the interval was not shorter than 6 months and the BED2 for each session was 100 Gy or less. The prescribed BED10 of 80 Gy could be safely delivered to the vertebral lesions.
Zusammenfassung
Hintergrund und Ziel:
Aggressive Strahlentherapie bei vertebralen Metastasen. Unter Einsatz sehr steiler Dosisgradienten intensitätsmodulierter Strahlentherapie (IMRT) Evaluierung eines Therapieprotokolls basierend auf dem Konzept der partiellen Volumendosierung am Rückenmark.
Patienten und Methodik:
Wir behandelten mit IMRT 50 Patienten mit Wirbelsäulenmetastasen. In Fällen ohne vorangegangene Strahlentherapie, bei denen eine verordnete Dosis von 80 Gy BED10 appliziert wurde, sollte die Belastung des Rückenmarks weniger als 100 Gy BED2 betragen. In Fällen mit vorheriger Strahlentherapie wurde die gleiche Dosis appliziert, wobei allerdings die Belastung des Rückenmarks kumulativ unter 150 Gy BED2 und in der Einzelapplikation bei weniger als 100 Gy BED2 lag, außerdem die Behandlungspause mehr als 6 Monate betrug. Für die partielle Volumendosierung am Rückenmark kamen 6 Patienten in Frage. Alle erhielten die höhere BED2 von mehr als 51 Gy bis zu 157 Gy D1cc.
Ergebnisse:
Unter 24 Patienten, die länger als ein Jahr überlebten, gab es einen Fall vorübergehender Strahlenmyelitis. Es wurden keine weiteren Fälle von Bestrahlungsfolgen am Rückenmark beobachtet.
Schlussfolgerung:
Auf Basis der vorliegenden Ergebnissen würden wir eine BED2 von 100 Gy oder weniger bei D1cc am Rückenmark in Fällen ohne vorangegangene Strahlentherapie empfehlen und in Fällen mit vorheriger Strahlentherapie eine kumulative BED2 von 150 Gy oder weniger bei D1cc, wenn das Behandlungsintervall nicht kürzer als 6 Monate war und die Dosis der Einzelapplikation bei einer BED2 von 100 Gy oder weniger lag. Die verordnete Dosis einer BED10 von 80 Gy bei Wirbelsäulenläsionen ließ sich sicher applizieren.
Similar content being viewed by others
References
Baba Y, Ohkubo K, Hamada K, et al. Percutaneous vertebroplasty for osteolytic metastasis: a case report. Nippon Acta Radiologica 1997;57:880–2.
Bentzen SM, Constine LS, Deasy JO, et al. Quantitative analysis of normal tissue effects in the clinic (QUANTEC): an introduction to the scientific issues. Int J Radiat Oncol Biol Phys 2010;76:S3–S9.
Chow E, Danjoux C, Wong R, et al. Palliation of bone metastases: a survey of patterns of practice among Canadian radiation oncologists. Radiother Oncol. 2000;56(3):305–14.
Emami B, Lyman J, Brown A, et al. Tolerance of normal tissue to therapeutic irradiation. Int J Radiat Oncol Biol Phys 1991;15:109–22.
Freundt K, Meyners T, Bajrovic A, et al. Radiotherapy for oligometastatic disease in patients with spinal cord compression (MSCC) from relatively radioresistant tumors. Strahlenther Onkol. 2010;186:218–23.
JASTRO Database Committee, Teshima T, Numasaki H, et al. Japanese structure survey of Radiation Oncology on 2007 (first report). J Jpn Soc Ther Radiol Oncol 2009;21:113–25.
Lammering G, De Ruysscher D, van Baardwijk A, et al. The use of FDG-PET to target tumors by radiotherapy. Strahlenther Onkol 2010;186:471–81.
Marks LB, Yorke ED, Jackson A, et al. Use of normal tissue complication probability models in the clinic. Int J Radiat Oncol Biol Phys 2010;76:S10–S19.
Masala S, Roselli M, Massari F, et al. Radiofrequency heat ablation and vertebroplasty in the treatment of neoplastic vertebral body fractures. Anticancer 2004;24:3129–33.
Meisner J, Meyer A, Polivka B, et al. Outcome of moderately dosed radiosurgery for limited brain metastases. Report of a single-center experience. Strahlenther Onkol 2010;186:76–81.
Nieder C, Grosu AL, Andratschke NH, et al. Update of human spinal cord reirradiation tolerance based on additional data from 38 patients. Int J Radiat Oncol Biol Phys 2006;66:1446–9.
Porter AT, McEwan AJB, Powe JE, et al. Results of a randomized phase-III trial to evaluate the efficacy of strontium-89 adjuvant to local field external beam irradiation in the management of endocrine resistant metastatic prostate cancer. Int J Radiat Oncol Biol Phys 1993;25:805–13.
Rades D, Dahm-Daphi J, Rudat V, et al. Is short-course radiotherapy with high doses per fraction the appropriate regimen for metastatic spinal cord compression in colorectal cancer patients? Strahlenther Onkol 2006;182:708–12.
Robinson RG. Strontium-89 precursor targeted therapy for pain relief of blastic metastatic disease. Cancer 1993;72(11 Suppl):3433–5.
Rubin P, Casarett GW. A direction for clinical radiation pathology. Front Radiation Ther Onc 1972;6:1–16.
Ryu S, Jin JY, Jin R, et al. Partial volume tolerance of the spinal cord and complications of single-dose radiosurgery. Cancer 2007;109:628–36.
Salazar OM, Sandhu T, da Motta NW, et al. Fractionated half-body irradiation (HBI) for the rapid palliation of widespread, symptomatic, metastatic bone disease: a randomized phase III trial of the International Atomic Energy Agency (IAEA), Int J Radiat Oncol Biol Phys 2001;50:765–75.
Souchon R, Wenz F, Sedlmayer F, et al. DEGRO practice guidelines for palliative radiotherapy of metastatic breast cancer: bone metastases and metastatic spinal cord compression (MSCC). Strahlenther Onkol 2009;185: 417–24.
Steenland E, Leer JW, van Houwelingen H, et al. The effect of a single fraction compared to multiple fractions on painful bone metastases: a global analysis of the Dutch Bone Metastasis study. Radiother Oncol 1999;52: 101–9.
Tong D, Gillick L, Hendrickson FR. The palliation of symptomatic osseous metastases: final results of the study by the Radiation Therapy Oncology Group. Cancer 1982;50:893–9.
van den Hout WB, van der Linden YM, Steenland E, et al. Single- versus multiple-fraction radiotherapy in patients with painful bone metastases: cost-utility analysis based on a randomized trial. J Natl Cancer Inst. 2003;95:222–9.
Author information
Authors and Affiliations
Corresponding author
Additional information
*This paper was presented at the 15th Workshop of German–Japanese Radiological Affiliation in Tokyo, Japan, on 23 May 2010.
Rights and permissions
About this article
Cite this article
Inoue, T., Oh, RJ. & Shiomi, H. New Approach for Treatment of Vertebral Metastases Using Intensity-Modulated Radiotherapy*. Strahlenther Onkol 187, 108–113 (2011). https://doi.org/10.1007/s00066-010-2187-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00066-010-2187-1