Purpose:
To evaluate the influence of breathing motion in postoperative whole-breast radiotherapy.
Patients and Methods:
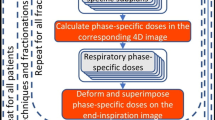
For ten patients with left-sided breast cancer, radiotherapy treatment plans were generated based on conventional three-dimensional computed tomography (3D CT) studies: two techniques (segmented and wedge-based tangential fields) were compared. The influence of breathing motion on the dose to the target and organs at risk (OARs) was evaluated with four-dimensional (4D) dose calculation based on respiration-correlated CTs. Reproducibility of breathing motion was evaluated with electronic portal images (EPID) acquired in cine mode during treatment.
Results:
Differences in dose distributions were small between segmented and wedge techniques based on 3D studies. Because of small motion amplitude of the chest in the 4D CT studies (1.8 mm ± 0.9 mm), target coverage was reduced by < 5% due to breathing motion. Differences between 3D and 4D dose calculation were similar for segmented and wedge techniques. Blurring of the dose distribution in 4D dose calculation resulted in lower doses to the OARs. Analysis of EPID movies proved good reproducibility of breathing motion observed in the 4D CT study.
Conclusion:
Breathing motion was of minor relevance in postoperative radiotherapy treatment of breast cancer for both segmented and wedge tangential field techniques.
Ziel:
Untersuchung zum Einfluss der Atembewegung auf die postoperative Brustbestrahlung.
Patienten und Methodik:
Die Bestrahlungsplanung von Tangentenfeldern basierte auf dreidimensionalen Computertomographie-( 3D-CT-)Studien von zehn Brustkrebspatientinnen: Zwei Bestrahlungstechniken (Keilfilterfelder und Segmenttechnik) wurden verglichen. Der Einfluss der Atembewegung auf die Dosis im Zielvolumen und in den Risikoorganen wurde über die akkumulierte Dosisverteilung bestimmt, die aus atemgetriggerten CTs (4D CT) berechnet wurde. Die Reproduzierbarkeit der Atembewegung wurde mittels Portal Image Movies analysiert.
Ergebnisse:
In den 3D-Studien wurden nur geringe Unterschiede zwischen segment- und keilbasierter Technik beobachtet. Die kleinen Bewegungsamplituden der Thoraxwand in den 4D CTs (1,8 mm ± 0,9 mm) verschlechterten die Zielvolumenerfassung nur wenig. Die Unterschiede zwischen den 3D- und 4D-Dosisverteilungen waren für segment- und keilbasierte Technik ähnlich. Die mittlere Dosis der Risikoorgane verringerte sich aufgrund der Dosisverschmierung. Die Auswertung der Portal Image Movies zeigte eine gute Reproduzierbarkeit der Bewegungsamplitude im Vergleich mit dem 4D CT.
Schlussfolgerung:
Die Atembewegung beeinflusste die postoperative Bestrahlung von Brustkrebspatientinnen sowohl für die keil- als auch die segmentbasierte Tangententechnik in geringem Maße.
Similar content being viewed by others
References
Abo-Madyan Y, Polednik M, Rahn A, et al. Improving dose homogeneity in large breasts by IMRT. Efficacy and dosimetric accuracy of different techniques. Strahlenther Onkol 2008;184:86–92.
Beckham WA, Popescu CC, Patenaude VV, et al. Is multibeam IMRT better than standard treatment for patients with left-sided breast cancer? Int J Radiat Oncol Biol Phys 2007;69:918–24.
Bhatnagar AK, Brandner E, Sonnik D, et al. Intensity modulated radiation therapy (IMRT) reduces the dose to the contralateral breast when compared to conventional tangential fields for primary breast irradiation. Breast Cancer Res Treat 2006;96:41–6.
Brown LM, Chen BE, Pfeiffer RM, et al. Risk of second non-hematological malignancies among 376,825 breast cancer survivors. Breast Cancer Res Treat 2007;106:439–51.
Ding C, Li X, Huq MS, et al. The effect of respiratory cycle and radiation beam-on timing on the dose distribution of free-breathing breast treatment using dynamic IMRT. Med Phys 2007;34:3500–9.
Donovan EM, Yarnold JR, Adams EJ, et al. An investigation into methods of IMRT planning applied to breast radiotherapy. Br J Radiol 2008;81:311–22.
Fein DA, McGee KP, Schultheiss TE, et al. Intra- and interfractional reproducibility of tangential breast fields: a prospective on-line portal imaging study. Int J Radiat Oncol Biol Phys 1996;34:733–40.
Fowble B, Hanlon A, Freedman G, et al. Second cancers after conservative surgery and radiation for stages I–II breast cancer: identifying a subset of women at increased risk. Int J Radiat Oncol Biol Phys 2001;51:679–90.
George R, Keall PJ, Kini VR, et al. Quantifying the effect of intrafraction motion during breast IMRT planning and dose delivery. Med Phys 2003;30:552–62.
Guckenberger M, Krieger T, Richter A, et al. Potential of image-guidance, gating and real-time tracking to improve accuracy in pulmonary stereotactic body radiotherapy. Radiother Oncol 2008;91:288–95.
Guckenberger M, Krieger T, Wilbert J, et al. Four dimensional target volume generation in pulmonary stereotactic body radiotherapy. Int J Radiat Oncol Biol Phys 2007;69:191.
Guckenberger M, Weininger M, Wilbert J, et al. Influence of retrospective sorting on image quality in respiratory correlated computed tomography. Radiother Oncol 2007;85:223–31.
Guckenberger M, Wilbert J, Krieger T, et al. Four-dimensional treatment planning for stereotactic body radiotherapy. Int J Radiat Oncol Biol Phys 2007;69:276–85.
Gulyban A, Kovacs P, Sebestyen Z, et al. Multisegmented tangential breast fields: a rational way to treat breast cancer. Strahlenther Onkol 2008;184:262–9.
Kestin LL, Sharpe MB, Frazier RC, et al. Intensity modulation to improve dose uniformity with tangential breast radiotherapy: initial clinical experience. Int J Radiat Oncol Biol Phys 2000;48:1559–68.
Kinoshita R, Shimizu S, Taguchi H, et al. Three-dimensional intrafractional motion of breast during tangential breast irradiation monitored with high-sampling frequency using a real-time tumor-tracking radiotherapy system. Int J Radiat Oncol Biol Phys 2008;70:931–4.
Liu Q, McDermott P Burmeister J. Effect of respiratory motion on the delivery of breast radiotherapy using SMLC intensity modulation. Med Phys 2007;34:347–51.
Ludwig V, Schwab F, Guckenberger M, et al. Comparison of wedge versus segmented techniques in whole breast irradiation. Effects on dose exposure outside the treatment volume. Strahlenther Onkol 2008;184:307–12.
Meyer J, Baier K, Richter A, et al. Analysis of different algorithms for tracking moving organs by means of megavoltage imaging. 8th Biennial ESTRO Meeting on Physics and Radiation Technology for Clinical Radiotherapy, Lisbon, Portugal, 24.–29.09.2005.
Meyer J, Richter A, Baier K, et al. Tracking moving objects with megavoltage portal imaging: a feasibility study. Med Phys 2006;33:1275–80
Panettieri V, Wennberg B, Gagliardi G, et al. SBRT of lung tumours: Monte Carlo simulation with PENELOPE of dose distributions including respiratory motion and comparison with different treatment planning systems. Phys Med Biol 2007;52:4265–81.
Pignol JP, Olivotto I, Rakovitch E, et al. A multicenter randomized trial of breast intensity-modulated radiation therapy to reduce acute radiation dermatitis. J Clin Oncol 2008;26:2085–92.
Richmond ND, Turner RN, Dawes PJ, et al. Evaluation of the dosimetric consequences of adding a single asymmetric or MLC shaped field to a tangential breast radiotherapy technique. Radiother Oncol 2003;67:165–70.
Robert Koch Institute. Cancer in Germany 2003–2004: incidence and trends, 6th edn. Berlin: Robert Koch Institute, 2008:113.
RTOG. NSABP protocol 0413. A randomized phase III study of conventional whole breast irradiation (WBI) versus partial breast irradiation (PBI) for women with stage 0, I, or II breast cancer - report no. 47. Philadelphia: RTOG, 2006:108.
Sautter-Bihl ML, Budach W, Dunst J, et al. DEGRO practical guidelines for radiotherapy of breast cancer I. Breast-conserving therapy. Strahlenther Onkol 2007;183:661–6.
Sidhu S, Sidhu NP, Lapointe C, et al. The effects of intrafraction motion on dose homogeneity in a breast phantom with physical wedges, enhanced dynamic wedges, and ssIMRT. Int J Radiat Oncol Biol Phys 2006;66:64–75.
Smith RP, Bloch P, Harris EE, et al. Analysis of interfraction and intrafraction variation during tangential breast irradiation with an electronic portal imaging device. Int J Radiat Oncol Biol Phys 2005;62:373–8.
Van Asselen B, Raaijmakers CP, Hofman P, et al. An improved breast irradiation technique using three-dimensional geometrical information and intensity modulation. Radiother Oncol 2001;58:341–7.
Van der Laan HP, Dolsma WV, Maduro JH, et al. Dosimetric consequences of the shift towards computed tomography guided target definition and planning for breast conserving radiotherapy. Radiat Oncol 2008;3:6.
Van Herk M, Remeijer P Lebesque JV. Inclusion of geometric uncertainties in treatment plan evaluation. Int J Radiat Oncol Biol Phys 2002;52:1407–22.
Wolthaus JW, Sonke JJ, van Herk M, et al. Comparison of different strategies to use four-dimensional computed tomography in treatment planning for lung cancer patients. Int J Radiat Oncol Biol Phys 2008;70:1229–38.
Woo TC, Pignol JP, Rakovitch E, et al. Body radiation exposure in breast cancer radiotherapy: impact of breast IMRT and virtual wedge compensation techniques. Int J Radiat Oncol Biol Phys 2006;65:52–8.
Yue NJ, Li X, Beriwal S, et al. The intrafraction motion induced dosimetric impacts in breast 3D radiation treatment: a 4DCT based study. Med Phys 2007;34:2789–800.
Zackrisson B, Arevarn M, Karlsson M. Optimized MLC-beam arrangements for tangential breast irradiation. Radiother Oncol 2000;54:209–12.
Zhang G, Jiang Z, Shepard D, et al. Direct aperture optimization of breast IMRT and the dosimetric impact of respiration motion. Phys Med Biol 2006;51:N357–69.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Richter, A., Sweeney, R., Baier, K. et al. Effect of Breathing Motion in Radiotherapy of Breast Cancer. Strahlenther Onkol 185, 425–430 (2009). https://doi.org/10.1007/s00066-009-1980-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00066-009-1980-1