Background and Purpose:
Hepatocellular carcinoma (HCC) patients with severe cirrhosis are usually treated with supportive care because of their poor prognosis. However, the survival of severe cirrhotic patients has recently improved due to advanced treatments. The aim of this study was to define the role of proton beam therapy for HCC patients with severe cirrhosis.
Patients and Methods:
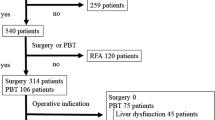
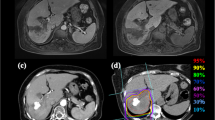
19 HCC patients with Child-Pugh class C cirrhosis received proton beam therapy. The hepatic tumors were solitary in 14 patients and multiple in five, and the tumor size was 25–80 mm (median 40 mm) in maximum diameter. No patient had regional lymph node or distant metastasis. Total doses of 50–84 Gy (median 72 Gy) in ten to 24 fractions (median 16) were delivered to the tumors.
Results:
Of the 19 patients, six, eight and four died of cancer, liver failure and intercurrent diseases, respectively, during the follow-up period of 3–63 months (median 17 months) after treatment. A remaining patient was alive with no evidence of disease 33 months after treatment. All but one of irradiated tumors were controlled during the follow-up period. Ten patients had new intrahepatic tumors outside the irradiated volume. The overall and progression-free survival rates were 53% and 47% at 1 year, respectively, and 42% each at 2 years. Performance status and Child-Pugh score were significant prognostic factors for survival. Therapy-related toxicity of grade 3 or more was not observed.
Conclusion:
Proton beam therapy for HCC patients with severe cirrhosis was tolerable. It may improve survival for patients with relatively good general condition and liver function.
Hintergrund und Ziel:
Patienten mit Leberzellkarzinom (HCC [„hepatocellular carcinoma“]) und schwerer Zirrhose werden aufgrund der schlechten Prognose gewöhnlich konservativ behandelt. Allerdings haben fortschrittliche Therapien in letzter Zeit zu einer Verbesserung der Überlebenszeit von Patienten mit schwerer Zirrhose geführt. Das Ziel der vorliegenden Studie war die Bestimmung der Rolle einer Protonentherapie für HCC-Patienten mit schwerer Zirrhose.
Patienten und Methodik:
19 HCC-Patienten mit Zirrhose der Child-Pugh-Klasse C wurden mit Protonenstrahlen behandelt. 14 Patienten wiesen einzelne und fünf Patienten multiple Lebertumoren auf. Hinsichtlich der Tumorgröße variierte der maximale Durchmesser dabei zwischen 25 und 80 mm (durchschnittlich 40 mm). Keiner der Patienten hatte regionäre Lymphknoten- oder Fernmetastasen in regionären oder entfernten Lymphknoten. Die Gesamtstrahlendosis betrug 50–84 Gy (durchschnittlich 72 Gy) und wurde in zehn bis 24 Fraktionen (durchschnittlich 16 Fraktionen) verabreicht.
Ergebnisse:
Im Nachuntersuchungszeitraum von 3–63 Monaten (durchschnittlich 17 Monate) verstarben sechs der insgesamt 19 Patienten an Krebs, acht an Leberversagen und vier an interkurrierenden Erkrankungen. Ein Patient war 33 Monate nach der Behandlung ohne Krankheitszeichen am Leben. Mit einer Ausnahme wurden alle Tumoren während der Nachuntersuchung mit entsprechenden Kontrollen verglichen. Zehn Patienten hatten intrahepatische Tumoren, die außerhalb des bestrahlten Bereichs lagen. Die Gesamt- und die progressionsfreie Überlebensrate betrugen nach 1 Jahr 53% und 47% und nach 2 Jahren 42%. Der Performance-Status und die Child-Pugh-Bewertung waren wichtige prognostische Faktoren für das Überleben.
Schlussfolgerung:
Die Protonentherapie war für Patienten mit Leberzellkarzinom und schwerer Zirrhose tolerabel. Die Behandlung könnte das Überleben von Patienten mit relativ gutem Allgemeinzustand und guter Leberfunktion verbessern.






Similar content being viewed by others
References
Altman DG. Practical statistics for medical research, 2nd edn. London: Chapman & Hall, 2004.
Ando K, Koike S, Kawachi K, et al. Relative biological effectiveness of the therapeutic proton beam at NIRS and Tsukuba University. Nippon Igaku Hoshasen Gakkai Zasshi 1985;45:531–535.
Blum HE. Treatment of hepatocellular carcinoma. Best Pract Res Clin Gastroenterol 2005;19:129–145.
Chiba T, Tokuuye K, Matsuzaki Y, et al. Proton beam therapy for hepatocellular carcinoma: a retrospective review of 162 patients. Clin Cancer Res 2005;11:3799–3805.
Cox JD, Stetz J, Pajak TF. Toxicity criteria of the Radiation Therapy Oncology Group (RTOG) and the European Organization for Research and Treatment of Cancer (EORTC). Int J Radiat Oncol Biol Phys 1995;31:1341–1346.
Di Carlo V, Ferrari G, Castoldi R, et al. Surgical treatment and prognostic variables of hepatocellular carcinoma in 122 cirrhotics. Hepatogastroenterology 1995;42:222–229.
Di Stasi M, Buscarini L, Livraghi T, et al. Percutaneous ethanol injection in the treatment of hepatocellular carcinoma. A multicenter survey of evaluation practices and complication rates. Scand J Gastroenterol 1997;32:1168–1173.
Ferro D, Saliola M, Quintarelli C, et al. 1-year survey of patients with advanced liver cirrhosis: prognostic value of clinical and laboratory indexes identified by the Cox regression model. Scand J Gastroenterol 1992;27:852–856.
Franco D, Capussotti L, Smadja C, et al. Resection of hepatocellular carcinoma. Results in 72 European patients with cirrhosis. Gastroenterology 1990;98:733–738.
Giorgio A, Tarantino L, Francica G, et al. Percutaneous ethanol injection under sonographic guidance of hepatocellular carcinoma in compensated and decompensated cirrhotic patients. J Ultrasound Med 1992;11:587–595.
Hata M, Tokuuye K, Sugahara S, et al. Proton beam therapy for hepatocellular carcinoma with portal vein tumor thrombus. Cancer 2005;104:794–801.
Höcht S, Stark R, Seiler F, et al. Proton or stereotactic photon irradiation for posterior uveal melanoma? A planning intercomparison. Strahlenther Onkol 2005;181:783–788.
Inada T, Tsuji H, Hayakawa Y, et al. Proton irradiation synchronized with respiratory cycle. Nippon Igaku Hoshasen Gakkai Zasshi 1992;52:1161–1167.
Kaplan EL, Meier P. Nonparametric estimation from incomplete observations. J Am Stat Assoc 1958;53:457–481.
Livraghi T, Bolondi L, Lazzaroni S, et al. Percutaneous ethanol injection in the treatment of hepatocellular carcinoma in cirrhosis. A study on 207 patients. Cancer 1992;69:925–929.
Llovet JM. Updated treatment approach to hepatocellular carcinoma. J Gastroenterol 2005;40:225–235.
Llovet JM, Bustamante J, Castells A, et al. Natural history of untreated nonsurgical hepatocellular carcinoma: rationale for the design and evaluation of therapeutic trials. Hepatology 1999;29:62–67.
Markovič S, Gadžijev E, Štabuc B, et al. Treatment options in Western hepatocellular carcinoma: a prospective study of 224 patients. J Hepatol 1998;29:650–659.
Matsuzaki Y, Osuga T, Saito Y, et al. A new, effective, and safe therapeutic option using proton irradiation for hepatocellular carcinoma. Gastroenterology 1994;106:1032–1041.
Miller AB, Hoogstraten B, Staquet M, et al. Reporting results of cancer treatment. Cancer 1981;47:207–214.
Mock U, Bogner J, Georg D, et al. Comparative treatment planning on localized prostate carcinoma. Strahlenther Onkol 2005;181:448–455.
Ohara K, Okumura T, Akisada M, et al. Irradiation synchronized with respiration gate. Int J Radiat Oncol Biol Phys 1989;17:853–857.
Oken MM, Creech RH, Tormey DC, et al. Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am J Clin Oncol 1982;5:649–655.
Planas R, Ballesté B, Álvarez MA, et al. Natural history of decompensated hepatitis C virus-related cirrhosis. A study of 200 patients. J Hepatol 2004;40:823–830.
Pugh RN, Murray-Lyon IM, Dawson JL, et al. Transection of the oesophagus for bleeding oesophageal varices. Br J Surg 1973;60:646–649.
Rutz HP, Lomax AJ. Donut-shaped high-dose configuration for proton beam radiation therapy. Strahlenther Onkol 2004;181:49–53.
Sobin LH, Wittekind C. TNM classification of malignant tumours, 6th edn. New York: Wiley-Liss, 2002:81–3.
Suit H, Goldberg S, Niemierko A, et al. Proton beams to replace photon beams in radical dose treatments. Acta Oncol 2003;42:800–808.
Tateishi R, Shiina S, Teratani T, et al. Percutaneous radiofrequency ablation for hepatocellular carcinoma. An analysis of 1000 cases. Cancer 2005;103:1201–1209.
Tokuuye K, Akine Y, Kagei K, et al. Proton therapy for head and heck malignancies at Tsukuba. Strahlenther Onkol 2004;180:96–101.
Withers HR, Thames HD Jr, Peters LJ. A new isoeffect curve for change in dose per fraction. Radiother Oncol 1983;1:187–191.
Acknowledgment
The present study was supported in part by a Grant-in-Aid for Cancer Research (15-9) from the Ministry of Health, Labor, and Welfare of the Japanese Government.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hata, M., Tokuuye, K., Sugahara, S. et al. Proton Beam Therapy for Hepatocellular Carcinoma Patients with Severe Cirrhosis. Strahlenther Onkol 182, 713 (2006). https://doi.org/10.1007/s00066-006-1564-2
Received:
Revised:
DOI: https://doi.org/10.1007/s00066-006-1564-2