Abstract
Objectives
There is limited knowledge regarding the specific interrelationships between urgent coronary artery bypass graft (U-CABG) surgery and postoperative acute kidney injury (AKI). We aimed to (1) analyze the impact of urgent CABG (U-CABG) on the incidence and severity of postoperative AKI, (2) estimate the influence of AKI after U‑CABG or elective CABG (E-CABG) on mortality and (3) identify risk factors for AKI depending on the urgency of operation.
Results
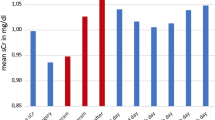
U‑CABG patients showed a higher incidence of AKI (49.8% vs. E‑CABG: 39.7%; p = 0.026), especially for higher AKI stages 2 + 3. In-hospital mortality was higher in U‑CABG patients (12.6%) compared to E‑CABG patients (2.3%; p < 0.001). The impact of AKI on mortality did not differ, but showed a strong coherency between higher AKI stages (2 + 3) and mortality (stage 1: OR 2.409, 95% CI 1.017–5.706; p = 0.046 vs. stage 2 + 3: OR 5.577; 95% CI 2.033–15.3; p = 0.001). Univariate logistic regression analysis revealed that preoperative renal impairment, peripheral vascular disease and transfusion of more than two red blood cell concentrates were predictors for postoperative AKI in both groups.
Conclusions
U‑CABG is a risk factor for postoperative AKI and even “mild” AKI leads to a significantly higher mortality. Hence, the prevention of modifiable risk factors might reduce the incidence of postoperative AKI and thus improve outcome.
Zusammenfassung
Hintergrund
Patienten mit dringlicher Indikation zur operativen Myokardrevaskularisation („urgent CABG“; U‑CABG) stellen aufgrund der zugrunde liegenden Pathophysiologie und des erhöhten perioperativen Risikos eine besondere Patientenklientel dar. Bezüglich der Charakterisierung einer auftretenden postoperativen Nierenfunktionseinschränkung in dieser Patientenpopulation ist wenig bekannt. Ziel der Vorliegenden Analyse war die Charakterisierung der Inzidenz und des Schweregrads einer postoperativen Nierenfunktionseinschränkung nach dringlicher aortokoronarer Bypassoperation.
Ergebnisse
Im Vergleich zu Patienten nach einer elektiven operativen Myokardrevaskularisation (elektiver CABG; E‑CABG) zeigten U‑CABG-Patienten eine signifikant höhere Inzidenz einer postoperativen akuten Nierenschädigung („acute kidney injury“, AKI) mit 49,8 % gegenüber 39,7 % nach E‑CABG (p = 0,026). Der Einfluss eines AKI auf die postoperative Mortalität war in den verglichenen Gruppen nicht unterschiedlich. Es zeigte sich allerdings ein deutlicher Zusammenhang zwischen höheren AKI-Stadien und einer erhöhten Mortalität (Stadium 1: OR 2,409, 95 %-KI 1,017–5,706; p = 0,046 vs. Stadium 2 und 3: OR 5,577; 95 %-KI 2,033–15,3; p = 0,001). In der univariaten logistischen Regressionsanalyse waren eine präoperative Nierenfunktionseinschränkung, das Vorhandensein einer peripheren arteriellen Verschlusskrankheit und die Transfusion von mehr als 2 Erythrozytenkonzentraten Risikofaktoren für das Auftreten eines postoperativen AKI.
Schlussfolgerung
Patienten mit dringlicher Indikation zur operativen Myokardrevaskularisation zeigen ein erhöhtes Risiko für das Auftreten einer postoperativen Nierenfunktionsstörung, die wiederum mit einem erhöhten Mortalitätsrisiko assoziiert ist. Hinsichtlich einer möglichen Prävention kommt insbesondere den modifizierbaren Risikofaktoren eine besondere Bedeutung zu.


Similar content being viewed by others
References
Bahar I, Akgul A, Ozatik MA et al (2005) Acute renal failure following open heart surgery: risk factors and prognosis. Perfusion 20:317–322
Brown JR, Cochran RP, Dacey LJ et al (2006) Perioperative increases in serum creatinine are predictive of increased 90-day mortality after coronary artery bypass graft surgery. Circulation 114:I409–I413
Brown JR, Cochran RP, Leavitt BJ et al (2007) Multivariable prediction of renal insufficiency developing after cardiac surgery. Circulation 116:I139–143
Brown JR, Cochran RP, MacKenzie TA et al (2008) Long-term survival after cardiac surgery is predicted by estimated glomerular filtration rate. Ann Thorac Surg 86:4–11
Chertow GM, Levy EM, Hammermeister KE et al (1998) Independent association between acute renal failure and mortality following cardiac surgery. Am J Med 104:343–348
Corredor C, Thomson R, Al-Subaie N (2016) Long-term consequences of acute kidney injury after cardiac surgery: a systematic review and meta-analysis. J Cardiothorac Vasc Anesth 30:69–75
Dardashti A, Ederoth P, Algotsson L et al (2014) Incidence, dynamics, and prognostic value of acute kidney injury for death after cardiac surgery. J Thorac Cardiovasc Surg 147:800–807
Doddakula K, Al-Sarraf N, Gately K et al (2007) Predictors of acute renal failure requiring renal replacement therapy post cardiac surgery in patients with preoperatively normal renal function. Interact CardioVasc Thorac Surg 6:314–318
Gallagher S, Jones DA, Lovell MJ et al (2014) The impact of acute kidney injury on midterm outcomes after coronary artery bypass graft surgery: a matched propensity score analysis. J Thorac Cardiovasc Surg 147:989–995
Hansen MK, Gammelager H, Mikkelsen MM et al (2013) Post-operative acute kidney injury and five-year risk of death, myocardial infarction, and stroke among elective cardiac surgical patients: a cohort study. Crit Care 17:R292
Hillis GS, Croal BL, Buchan KG et al (2006) Renal function and outcome from coronary artery bypass grafting: impact on mortality after a 2.3-year follow-up. Circulation 113:1056–1062
Hobson CE, Yavas S, Segal MS et al (2009) Acute kidney injury is associated with increased long-term mortality after cardiothoracic surgery. Circulation 119:2444–2453
Ji Q, Mei Y, Wang X et al (2012) Effect of elapsed time from coronary angiography until off-pump coronary artery bypass surgery on postoperative renal function. Circ J 76:2356–2362
Joannidis M, Klein SJ, John S et al (2018) Prävention der akuten Nierenschädigung beim kritisch kranken Patienten: Empfehlungen der Sektionen Niere der DGIIN, ÖGIAIN und DIVI [Prevention of acute kidney injury in critically ill patients: recommendations from the renal section of the DGIIN, ÖGIAIN and DIVI]. Med Klin Intensivmed Notfmed 113(5):358–369
Karkouti K, Wijeysundera DN, Beattie WS et al (2007) Variability and predictability of large-volume red blood cell transfusion in cardiac surgery: a multicenter study. Transfusion 47:2081–2088
Khwaja A (2012) KDIGO clinical practice guidelines for acute kidney injury. Nephron Clin Pract 120:c179–c184
Landoni G, Bove T, Crivellari M et al (2007) Acute renal failure after isolated CABG surgery: six years of experience. Minerva Anestesiol 73:559–565
Li SY, Chen JY, Yang WC et al (2011) Acute kidney injury network classification predicts in-hospital and long-term mortality in patients undergoing elective coronary artery bypass grafting surgery. Eur J Cardiothorac Surg 39:323–328
Liotta M, Olsson D, Sartipy U et al (2014) Minimal changes in postoperative creatinine values and early and late mortality and cardiovascular events after coronary artery bypass grafting. Am J Cardiol 113:70–75
Lopez-Delgado JC, Esteve F, Torrado H et al (2013) Influence of acute kidney injury on short- and long-term outcomes in patients undergoing cardiac surgery: risk factors and prognostic value of a modified RIFLE classification. Crit Care 17:R293
Meersch M, Schmidt C, Hoffmeier A et al (2017) Prevention of cardiac surgery-associated AKI by implementing the KDIGO guidelines in high risk patients identified by biomarkers: the PrevAKI randomized controlled trial. Intensive Care Med 43:1551–1561
Ranucci M, Aloisio T, Cazzaniga A, Di Dedda U, Gallazzi C, Pistuddi V (2018) Validation of renal-risk models for the prediction of non-renal replacement therapy cardiac surgery-associated acute kidney injury. Int J Cardiol 272:49–53
Ryden L, Ahnve S, Bell M et al (2014) Acute kidney injury after coronary artery bypass grafting and long-term risk of myocardial infarction and death. Int J Cardiol 172:190–195
Vives M, Hernandez A, Parramon F et al (2019) Acute kidney injury after cardiac surgery: prevalence, impact and management challenges. Int J Nephrol Renovasc Dis 12:153–166
Warren J, Mehran R, Baber U et al (2016) Incidence and impact of acute kidney injury in patients with acute coronary syndromes treated with coronary artery bypass grafting: insights from the Harmonizing Outcomes With Revascularization and Stents in Acute Myocardial Infarction (HORIZONS-AMI) and Acute Catheterization and Urgent Intervention Triage Strategy (ACUITY) trials. Am Heart J 171:40–47
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
M. Scherner, C. Weber, H. Schmidt, K. Kuhr, S. Hamacher, A. Sabashnikov, K. Eghbalzadeh, N. Mader, T. Wahlers and J. Wippermann declare that they have no competing interests.
This study was approved by our Institutional Review Board. Individual informed consent was waived due to retrospective analysis of existing patient data. All studies mentioned were in accordance with the ethical standards indicated in each case.
Additional information
Redaktion
M. Buerke, Siegen
M. Scherner and C. Weber contributed equally to this work.
Rights and permissions
About this article
Cite this article
Scherner, M., Weber, C., Schmidt, H. et al. Impact of urgent coronary artery bypass grafting on acute kidney injury. Med Klin Intensivmed Notfmed 117, 152–158 (2022). https://doi.org/10.1007/s00063-020-00769-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00063-020-00769-x