Abstract
Background
Acute kidney injury (AKI) is a common and severe complication in patients in the intensive care unit with a significant impact on patient’s mortality and morbidity. Therefore renal protective therapy is very important in these severely ill patients.
Aim
Several renal protective strategies have been postulated during recent decades, which came from pathophysiologic concepts and have been contradicted or changed during the last few years. So lessons had to be learned in AKI, leading to new, in many cases completely reversed preventive and therapeutic concepts which may also be important for protection in other organs.
Recent findings
Most important for renal protection is the early identification of patients at risk for AKI or with acute kidney damage before renal function further deteriorates. A stage-based management of AKI comprises more general measures like discontinuation of the nephrotoxic agent but most importantly early hemodynamic stabilization. Recent research has contradicted that AKI is renal ischemia caused by vasoconstriction with consecutive tubular necrosis. In septic AKI, renal blood flow is even increased. Intrarenal vasodilation together with microcirculatory changes and redistribution of blood flow lead to a drop in glomerular filtration by functional changes. Accordingly it had to be learned that not vasodilators but vasoconstrictors are beneficial in AKI. A mean arterial blood pressure target of >65 mm Hg is often recommended but exact targets are not known, and patients with pre-existing hypertension even need higher perfusion pressure. Also the concept that fluid therapy is always beneficial for the kidney in shock states had to be revised. A volume restrictive therapy with only balanced crystalloids is also becoming more important in AKI. Still no specific pharmacological therapy for renal protection is available. Inflammation and mitochondrial dysfunction appear to play a significant role in AKI. Anti-inflammatory strategies are under investigation and may become more important for AKI prevention and therapy in the future. (This article is freely available.)
Zusammenfassung
Hintergrund
Das akute Nierenversagen („acute kidney injury“, AKI) ist eines der häufigsten Organversagen auf Intensivstationen mit signifikanten Folgen für Mortalität und Morbidität der Patienten. Einer Prävention dieses Organversagens kommt damit eine wichtige Bedeutung in der Behandlung schwer kranker Patienten zu.
Ziel
Zahlreiche nierenprotektive Strategien wurden in den letzten Jahrzehnten postuliert, die aber in vielen Fällen auf inzwischen widerlegten oder veränderten pathophysiologischen Vorstellungen beruhten. So konnte in den letzten Jahren vieles über das Organversagen AKI gelernt werden, was zu neuen, oft ganz gegensätzlichen Präventions- und Therapieansätzen geführt hat. Ziel der Übersicht ist es, einige dieser veränderten Vorstellungen am Organ Niere darzustellen. Dies kann aber durchaus auch Bedeutung für die Prävention anderer Organversagen haben.
Aktuelle Ergebnisse
Wichtigstes Ziel jeder nierenprotektiven Therapie muss es sein, Patienten mit hohem Risiko für ein AKI oder Auftreten einer Nierenschädigung frühzeitig zu erkennen, um eine weitere Verschlechterung der Nierenfunktion zu vermeiden. Ein stadienbasiertes Management einer Nierenschädigung besteht in der raschen Umsetzung allgemeiner Behandlungsmaßnahmen, wie dem Absetzen nephrotoxischer Medikamente, aber v. a. in einer raschen hämodynamischen Stabilisierung. Bestand früher die Vorstellung, dass ein AKI durch renale Ischämie mit konsekutiver Tubulusnekrose verursacht wird, wissen wir heute, dass ein AKI bei septischem Schock sogar mit einem erhöhten renalen Blutfluss einhergeht. Eine ausgeprägte Vasodilatation mit Umverteilung des Blutflusses führt v. a. über funktionelle Änderungen zu einem Abfall der glomerulären Filtration. Entsprechend sind es nicht Vasodilatatoren, sondern Vasokonstriktoren, die bei AKI eher günstig sind. Oft wird ein arterieller Mitteldruck von >65 mm Hg empfohlen, aber genaue Ziele sind nicht bekannt und Patienten mit vorbestehender arterieller Hypertonie benötigen eher höhere Perfusionsdrücke. Auch die Vorstellung, dass Volumen für die Niere immer gut wäre, musste revidiert werden. Eine volumenrestriktive Therapie mit ausschließlich balanciertem, kristalloidem Volumenersatz bekommt auch bei AKI eine immer größere Bedeutung. Eine gesicherte spezifische pharmakologische Therapie für eine wirksame Nierenprotektion besteht derzeit nicht. Inflammation und mitochondriale Dysfunktion scheinen aber bei AKI ebenfalls eine entscheidende Rolle zu spielen. Entsprechend werden antiinflammatorische Therapieansätze als zukünftige Chance in der Organprotektion gesehen.
Similar content being viewed by others
Introduction
One in five adults develops acute kidney injury (AKI) during a hospital stay worldwide and AKI affects up to 50% of critically ill patients [1,2,3]. The most frequent causes of AKI in the critically ill are sepsis, hypovolemia, nephrotoxic agents, and major surgery [4]. Mortality remains high between 20 and 60% depending on the underlying disease [4, 5]. Even survivors of only mild or short episodes of AKI are predisposed to a greater risk of developing chronic and end-stage renal disease or severe cardiovascular complications in later life. These facts underline the importance of AKI as one of the major organ failures during sepsis and critical illness. Currently there is no specific pharmacologic intervention available to treat AKI. Therefore, preventive strategies to avoid AKI whenever possible are crucial. To develop such strategies early recognition of AKI but also understanding the underlying pathophysiology of septic AKI is most important. However, during recent decades there have been some misconceptions in the underlying mechanisms leading to AKI. Lessons had to be learned, which might be of importance to develop new preventive or even therapeutic strategies not only in AKI, but also in other organ failure. The aim of this article is to focus on some of these changing concepts in prevention and therapy of AKI.
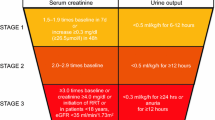
Definition, early detection, and identification of “high-risk” patients
For decades the diagnosis of AKI has been based on a rise in serum creatinine (S-Crea) and/or a fall in urine output (UO), but many different definitions concerning these two parameters had been used. As a major improvement, the KDIGO guidelines combined these different definitions to one uniform definition [1]. However, by relying on S‑Crea and UO changes the KDIGO definition is still limited by a timely and also accurate diagnosis. Moreover, it not only neglects subclinical forms of kidney dysfunction and damage, but is also not able to identify patients at high risk for AKI. Electronic automated alert systems were developed to warn healthcare providers as soon as a rise in S‑Crea is detected [6]. In addition, a variety of renal biomarkers have been identified to recognize functional changes and even damage to the kidneys prior to an S‑Crea rise or drop in UO [7, 8]. However, up to now no clear outcome benefit has been demonstrated for measuring these markers or for early alert systems [9]. Thus, they have not found their way into clinical practice yet. Very recently there has been promising work on modelling adverse events from electronic health records suggesting that the incorporation of machine learning algorithms may enable early risk prediction for AKI [10, 11]. But evidence that these predictive alerts can improve outcome is again still lacking. To be effective these alerts must empower clinicians to apply preventive strategies before a clinical decline occurred.
Preventive measures for AKI
The clinical management of patients with “high risk” or already established AKI has shown wide variability. So with the introduction of the “KDIGO AKI care bundles” a more uniform standard of care has been established ([1]; Fig. 1).
The KDIGO “AKI bundles” for prevention and management of AKI. GFR glomerular filtration rate. Adapted from [1]
According to these bundles the majority of the proposed measures should be considered already in “high risk” for AKI. This underlines the critical need for identifying high-risk patients early. Since there is no effective pharmacological treatment to reverse AKI, the mainstay of management consists of prevention of further damage by ensuring volume status and organ perfusion with hemodynamic resuscitation in addition to avoiding further nephrotoxic insults. However, the optimal targets of hemodynamic resuscitation are not known and there have been a couple of common beliefs on pathophysiological mechanisms in septic AKI which have been contradicted by recent studies.
Septic AKI is not global renal ischemia
Initial post-mortem and biopsy findings some decades ago found acute tubular necrosis (ATN) as the predominant histopathology in AKI. So in analogy with other shock forms, as cardiogenic or hemorrhagic shock, it was thought that septic AKI is predominantly the consequence of intrarenal vasoconstriction and global renal ischemia leading to ATN [12]. In addition, former studies found intrarenal vasoconstriction and a decline in renal blood flow (RBF) as the underlying explanation for such renal ischemia. However, RBF is difficult to measure in humans and newer data in patients or also animals with hyperdynamic shock states like septic shock found that global RBF is preserved or even increased [13]. So the renal circulation seems to participate in the systemic vasodilatation seen during severe sepsis/septic shock and global RBF does not diminish, but AKI still can develop [14]. Importantly, the normal mean pressure gradient driving glomerular filtration (GFR) is only approximately 10 mm Hg, demanding close autoregulation of glomerular capillary pressure by modification of the relative resistances in the afferent and efferent glomerular arterioles to maintain GFR (Fig. 2). In hyperdynamic septic shock, cardiac output is increased in the context of systemic vasodilation and hypotension. In these circumstances, systemic vasodilation will affect the kidney. Because baseline efferent tone is higher than afferent tone, this causes preferential efferent vasodilation and the development of a high-flow, low-pressure renal circulation in which GFR becomes uncoupled from the increase in RBF (Fig. 2). Despite high RBF, glomerular filtration pressure may be too low to drive effective ultrafiltration. In this context, histological assessment of postmortem kidneys from nonsurvivors of septic AKI shows heterogeneous, inflammatory tubular and microvascular injury, but an absence of ATN or severe tubular cell apoptosis in most cases. These findings suggest that defects of septic AKI may be functional rather than structural in nature and therefore potentially reversible. Vasopressors rather than vasodilators may be helpful to correct systemic but also intraglomerular pressures and consequently GFR and renal function. Moreover, microcirculatory dysfunction and redistribution of intrarenal perfusion away from the medulla to increased renal cortical tissue perfusion may be another explanation for increased tubular stress and ischemia, which may affect nephron integrity [15]. In addition, inflammation and bio-adaptive responses to injury, including mitochondrial dysfunction, downregulated cell metabolism and cell-cycle arrest are other proposed mechanisms leading to severe functional impairment despite preserved renal hemodynamics and histology [16].
Glomerular hemodynamics under normal conditions (left): glomerular filtration pressure and glomerular filtration rate (GFR) can be maintained by slight afferent vasodilation and slight efferent vasocontriction independently from mean arterial pressure (renal autoregulation). In hyperdynamic septic shock renal perfusion may be increased by efferent vasodilation by reducing overall renal vascular resistance but results in reduced glomerular filtration pressure. Adapted from [13]
Vasopressor therapy—cornerstone of AKI prevention and therapy
Since the former misconception that intrarenal vasoconstriction predominates septic AKI renal vasodilators have been proposed for AKI prevention and therapy for many years. But all clinical trials on vasodilators (e.g., renal-dose dopamine, fenoldapam, atrial natriuretic peptide, levosimendan) failed to show any benefit. Moreover vasodilators may cause hypotension by counteracting compensatory vasoconstriction, thus, unmasking occult hypovolemia and leading to further deterioration of kidney function. In contrast, vasopressors have been shown to improve kidney function and several clinical studies with both norepinephrine and vasopressin have shown improvement, not deterioration, of kidney function with increased MAP in patients with sepsis [17, 18]. Norepinephrine is the first-choice vasopressor recommended to restore mean arterial pressure (MAP) to at least 65 mm Hg [19]. Vasopressin is recommended as a rescue vasopressor for patients who are not responsive to norepinephrine and/or for reducing the dose of norepinephrine [18]. Since vasopressin and also angiotensin II may have a stronger pressor effect on postglomerular arterioles than norepinephrine, both substances have been proposed to have advantages in AKI. A recent meta-analysis on a patient basis showed a significant reduction for the need of renal replacement therapy in septic shock with vasopressin in comparison to norepinephrine [20]. For angiotensin II a faster recovery of renal function and a decreased mortality have been shown in a subgroup of the ATHOS‑3 study [21]. Further studies are needed to confirm these preliminary observations.
Individual MAP goals
In AKI guidelines usually a MAP goal ≥65 mm Hg is recommended [17, 18]. However, the exact MAP and perfusion targets to prevent AKI in individual patients are not known. In patients with pre-existing arterial hypertension higher blood pressure levels to above 80 mm Hg appear to be associated with less AKI and RRT (renal replacement therapy) need in one study [22]. This finding in septic shock patients may be important not only for AKI prevention but also for other organ failure prevention and underlines the need for more individualized pressure and perfusion targets as well as organ failure prevention strategies.
Fluid therapy—not always beneficial for the kidneys
Sepsis and hypovolemia are significant risk factors for the development of AKI. Early fluid administration is a cornerstone of therapy not only in septic shock states but is also an effective measure in preventing AKI through restoration of circulating volume and improving impaired renal perfusion [18]. Since prerenal AKI states typically respond rapidly to intravenous fluid therapy it was thought to be helpful in almost all other forms of AKI. Fluid therapy seems to be a logical option to increase stroke volume, cardiac output and RBF, renal oxygen supply and perhaps GFR. However, at least in septic or post-operative AKI multiple studies confirmed an independent association between a positive fluid balance and mortality [23, 24]. As pointed out, RBF is already high in septic AKI and fluid administration can lead to an increased workload to the kidneys because of increased filtration of sodium chloride leading to increased reabsorption by tubular cells with an increased O2 and ATP demand. Furthermore aggressive fluid therapy in septic shock will cause fluid overload and severe interstitial edema and increased parenchymal pressure in almost all organ tissues, also in the kidneys [13, 25]. Increased central venous pressure reduces the transrenal pressure gradient for RBF, therefore, decreasing kidney perfusion [26]. In addition, increased interstitial and tubular pressure induced by interstitial edema formation may reduce or even abolish the net glomerular filtration pressure gradient [27]. Increased preglomerular resistance in response to tubular injury further reduces RBF and glomerular filtration pressure. Hyperchloremia, as caused by chloride-rich infusion solutions, might contribute to preglomerular vasoconstriction by a pathophysiological activation of the tubular–glomerular feedback mechanism. In severe form of fluid overload intra-abdominal hypertension may develop which restricts venous drainage and extrinsically compresses the kidney (Fig. 3).
Renal consequences of fluid overload. Mean glomerular capillary pressure is approximately 45 mm Hg. Minus the counterdirected intracapsular and colloidosmotic pressure net glomerular filtration pressure is approximately 10 mm Hg. In septic states capillary pressure is already reduced. Fluid overload with increased renal venous pressure and increased vascular permeability leads to intrarenal edema formation and increased intracapsular pressure. Consequently glomerular filtration pressure and glomerular filtration rate (GFR) will be reduced. In the same way increased intra-abdominal pressure will cause functional deterioration of GFR. Adapted from [27]
Thus fluid overload seems to be associated with major adverse kidney events in critically ill patients with AKI requiring continuous renal replacement therapy [28]. Based on these pathophysiological considerations there are no studies showing that aggressive fluid therapy or a positive fluid balance are beneficial to kidney function in settings other than major body fluid losses and severe volume depletion. In contrast, observational data indicated an increased risk of AKI with increasing central venous pressure and a positive fluid balance in adjusted analyses of ICU patients [26]. Recently the randomized CLASSIC trial suggested that additional fluid may not increase urinary output [29]. In this trial patients with septic shock were randomized to either a protocol with restrictive fluid resuscitation or a protocol with standard care. In the fluid restriction group significantly fewer patients had worsening of AKI than in the standard care group. Also in the three-armed PROCESS trial, the group of septic patients who received the highest amount of fluids (standard care group) had also the highest risk of new onset AKI compared to the other two groups (EGDT [early goal directed therapy] and usual care group) [30]. Very recently the RIFTS trial demonstrated that a restrictive resuscitation strategy can successfully reduce the amount of i.v. fluid administered to patients with severe sepsis and septic shock compared with usual care. Although limited by sample size, the trial observed no increase in mortality and organ failure including AKI with the restrictive fluid strategy [31]. Since fluid overload is strongly associated with adverse outcomes it should be carefully guided with the employment of early vasopressor support. However, the optimal balance between vasopressor support and fluid resuscitation remains to be better determined. But minimizing the necessary fluid intake during the initial resuscitation phase seems to be of great importance because the later process of fluid removal will necessarily induce intravascular hypovolemia with falls in cardiac output and the consequent risk of recurrent renal or other organ injury. Recently, it has been shown that among critically ill patients with fluid overload and receiving CRRT (continous renal replacement therapy) with a high ultrafiltration intensity compared with a lower intensity was associated with lower survival [32].
Balanced crystalloids—best choice for the kidneys
There has been a long lasting debate which type of i.v. fluids should be administered in septic shock but also in AKI. Most of the answers we have today came from the renal side effects of certain fluids. Large trials and systematic reviews demonstrated increased rates of AKI and use of RRT and even increased mortality with hydroxyethyl starch (HES) in critically ill patients, including those with sepsis [17]. So there is high evidence that HES is not recommended in sepsis or AKI [27]. For the use of gelatins a similar recommendation appears warranted for patients with AKI; however the evidence base for this statement is much lower. Albumin, on the other hand, seems to be safe in AKI patients, but whether there is an advantage compared to crystalloids remains to be proven [33]. Crystalloids are the accepted first-line i.v. fluid in sepsis and AKI and high quality studies have recently demonstrated that low chloride, balanced crystalloids (e.g., Ringer’s) are associated with a lower AKI risk than chloride-rich 0.9% saline [34, 35]. Besides the induction of hyperchloremic acidosis, chloride-rich solutions can lead to progressive intrarenal, preglomerular vasoconstriction with the consequence of a decrease in GFR.
Inflammation and mitochondrial dysfunction
There is still no specific treatment for AKI. Since septic AKI with significant functional impairment can occur despite preserved global and renal hemodynamics and histology other mechanisms are postulated to be of major importance in the development of AKI. As a “unifying theory” it has been conceptualized that sepsis-induced AKI may represent the early clinical and biochemical manifestation of an adaptive response of tubular cells to an injurious, inflammatory danger signal [36]. During sepsis, inflammatory mediators and damage or pathogen-associated molecular patterns (DAMPs/PAMPs) will not only activate the immune system but also mediate host cellular injury. The interplay of inflammation and microvascular dysfunction and oxidative stress may amplify these signals with the consequence of mitochondrial dysfunction within tubular cells leading to a complete metabolic downregulation and reprioritization which favors individual cell survival processes, such as maintenance of membrane potential and cell cycle arrest, at the expense of kidney function [16, 36]. Thus, future targets for prevention and therapy of AKI may represent a better protection of the microvasculature and the endothelium, an improved balance in energy utilization and especially a modulation of inflammation.
Recently, alkaline phosphatase (AP), an endogenous enzyme that exerts detoxifying effects through dephosphorylation of various PAMPs, including bacterial endotoxin and proinflammatory mediators such as extracellular ATP, has been proposed as a specific therapy for AKI. The STOP-AKI trial, a randomized, double-blind, placebo-controlled dose-finding study determined the optimal dose but also effects on kidney function of a human recombinant AP in critically ill patients with septic AKI [37]. However, this study was not able to demonstrate a significant improvement in short-term kidney function (7 days) as the primary outcome, but a beneficial effect on kidney function after 28 days was discussed. In addition, AP beneficially affected “major adverse kidney events” (MAKE) at 60 and 90 days, mainly driven by a difference in survival. However, mortality was not a prespecified endpoint in this small study. Further research in a larger clinical trial is needed to determine effects of AP not only on kidney function but on the septic process and organ failure prevention in general. Perhaps lessons learned from AKI may be beneficial even for mortality in septic patients.
Conclusion
For preventing organ failure the following lessons can be learned from acute kidney injury:
Early diagnosis and recognition of high risk patients is crucial.
Prevention includes more general measures like removing toxins and optimizing hemodynamics.
Organ failure is often functional despite maintained organ perfusion and cellular integrity.
Vasopressor therapy and maintenance of mean arterial pressure is organ protective. Pressure goals remain to be better defined, but should be individualized.
Rapid fluid therapy is important but overhydration may worsen organ function.
Balanced crystalloids are best choice for fluid resuscitation.
Inflammatory processes and mitochondrial dysfunction are new targets for development of novel therapeutic strategies.
References
Kidney Disease: Improving Global Outcomes (KDIGO) Acute Kidney Injury Work Group (2012) KDIGO clinical practice guideline for acute kidney injury. Kidney Int Suppl 2:1–138
Susantitaphong P, Cruz DN, Cerda J et al (2013) World incidence of AKI: a metaanalysis. Clin J Am Soc Nephrol 8:1482–1493
Mehta RL, Cerdá J, Burdmann EA et al (2015) International society of nephrology’s 0by25 initiative for acute kidney injury (zero preventable deaths by 2025): a human rights case for nephrology. Lancet 385:2616–2643
Uchino S, Kellum JA, Bellomo R et al (2005) Acute renal failure in critically ill patients: a multinational, multicenter study. JAMA 294:813–818
Nisula S, Kaukonen K‑M, Vaara ST et al (2013) Incidence, risk factors and 90-day mortality of patients with acute kidney injury in Finnish intensive care units: the FINNAKI study. Intensive Care Med 39:420–428
Colpaert K, Hoste EA, Steurbaut K et al (2012) Impact of real-time electronic alerting of acute kidney injury on therapeutic intervention and progression of RIFLE class. Crit Care Med 40:1164–1170
Pickering JW, Endre ZH (2016) Bench to bedside: the next steps for biomarkers in acute kidney injury. Am J Physiol Renal Physiol 311:F717–F721
Joannidis M, Forni LG, Haase M et al (2019) Use of cell cycle arrest biomarkers in conjunction with classical markers of ccute kidney injury. Crit Care Med 47:e820–e826
Wilson FR, Shashaty M, Testani J et al (2015) Automated, electronic alerts for acute kidney injury: a single-blind, parallel-group, randomized controlled trial. Lancet 385:1966–1974
Koyner JL, Carey KA, Edelson DP, Churpek MM (2018) The development of a machine learning inpatient acute kidney injury prediction model. Crit Care Med 46:1070–1077
Tomasev N, Glorot X, Rae JW et al (2019) A clinically applicable approach to continuous prediction of future acute kidney injury. Nature 572:116–119
Schrier RW, Wang W (2004) Acute renal failure and sepsis. N Engl J Med 351:159–169
Prowle JR, Bellomo R (2015) Sepsis-associated acute kidney injury: macrohemodynamic and microhemodynamic alterations in the renal circulation. Semin Nephrol 35:64–74
Langenberg C, Wan L, Egi M et al (2007) Renal blood flow and function during recovery from experimental septic acute kidney injury. Intensive Care Med 33:1614–1618
Ma S, Evans RG, Iguchi N et al (2019) Sepsis-induced acute kidney injury: a disease of the microcirculation. Microcirculation 26:e12483
Arulkumaran N, Pollen S, Greco E et al (2018) Renal tubular cell mitochondrial dysfunction occurs despite perserved renal oxygen delivery in experimental septic acute kidney injury. Crit Care Med 46:e318–e325
Rhodes A, Evans LE, Alhazzani W et al (2017) Surviving sepsis campaign: international guidelines for management of sepsis and septic shock: 2016. Intensive Care Med 43:304–377
Joannidis M, Druml W, Forni LG et al (2017) Prevention of acute kidney injury and protection of renal function in the intensive care unit: update 2017. Intensive Care Med 43:730–749
De Backer D, Biston P, Devriendt J et al (2010) Comparison of dopamine versus norepinephrine in the treatment of shock. N Engl J Med 362:779–789
Nagendran M, Russell JA, Walley KR et al (2019) Vasopressin in septic shock: an individual patient data meta-analysis of randomised controlled trials. Intensive Care Med 45:844–8552019
Tumlin JA, Murugan R, Deane AM et al (2018) Outcomes in patients with vasodilatory shock and renal replacement therapy treated with intravenous angiotensin II. Crit Care Med 46:949–957
Asfar P, Meziani F, Hamel J‑F et al (2014) High versus low blood-pressure target in patients with septic shock. N Engl J Med 370:1583–1593
National Heart, Lung, and Blood Institute Acute Respiratory Distress Syndrome (ARDS) Clinical Trials Network (2006) Comparison of two fluid management strategies in acute lung injury. N Engl J Med 354:2564–2575
Grams ME, Estrella MM, Coresh J et al (2011) Fluid balance, diuretic use, and mortality in acute kidney injury. Clin J Am Soc Nephrol 6:966–973
Prowle JR, Kirwan CJ, Bellomo R (2014) Fluid management for the prevention and attenuation of acute kidney injury. Nat Rev Nephrol 10:37–47
Chen KP, Cavender S, Lee J et al (2016) Peripheral edema, central venous pressure, and risk of AKI in critical illness. Clin J Am Soc Nephrol 11:602–608
Perner A, Prowle JR, Joannidis M et al (2017) Fluid management in acute kidney injury. Intensive Care Med 43:807–815
Woodward CW, Lambert J, Ortiz-Soriano V et al (2019) Fluid overload is associated with major adverse kidney events in critically ill patients with acute kidney injury requiring continuous renal replacement therapy. Crit Care Med 47:e753–e760
Hjortrup PB, Haase N, Bundgaard H et al (2016) Restricting volumes of resuscitation fluid in adults with septic shock after initial management: the CLASSIC randomized, parallel-group, multicenter feasibility trial. Intensive Care Med 42:1695–1705
Kellum JA, Chawla LS, Keener C et al (2016) The effects of alternative resuscitation strategies on acute kidney injury in patients with septic shock. Am J Respir Crit Care Med 193:281–287
Corl KA, Prodromou M, Merchant RC et al (2019) The restrictive iv fluid trial in severe sepsis and septic shock (RIFTS): a randomized pilot study. Crit Care Med 47:951–959
Murugan R, Kerti SJ, Chang CH et al (2019) Association of net ultrafiltration rate with mortality among critically ill adults with acute kidney injury receiving continuous venovenous hemodiafiltration—a secondary analysis of the randomized evaluation of normal vs augmented level (RENAL) of renal replacement therapy trial. JAMA Netw Open 2:e195418
Caironi P, Tognoni G, Masson S et al (2014) Albumin replacement in patients with severe sepsis or septic shock. N Engl J Med 370:1412–1421
Semler MW, Self WH, Wanderer JP et al (2018) Balanced crystalloids versus saline in critically ill adults. N Engl J Med 378:829–839
Self WH, Semler MW, Wanderer JP et al (2018) Balanced crystalloids versus saline in noncritically ill adults. N Engl J Med 378:819–828
Gomez H, Ince C, De Backer D et al (2014) A unified theory of sepsis-induced acute kidney injury: inflammation, microcirculatory dysfunction, bioenergetics, and the tubular cell adaptation to injury. Shock 41:3–11
Pickkers P, Mehta RL, Murray PT et al (2018) Effect of human recombinant alkaline phosphatase on 7‑day creatinine clearance in patients with sepsis-associated acute kidney injury: a randomized clinical trial. JAMA 320:1998–2009
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
S. John declares that he has no competing interests.
For this article no studies with human participants or animals were performed by the author. All studies performed were in accordance with the ethical standards indicated in each case.
The supplement containing this article is not sponsored by industry.
Additional information
Redaktion
M. Bauer, Jena
M. Singer, London
Rights and permissions
About this article
Cite this article
John, S. Lessons learned from kidney dysfunction. Med Klin Intensivmed Notfmed 115 (Suppl 1), 21–27 (2020). https://doi.org/10.1007/s00063-020-00659-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00063-020-00659-2