Abstract
Introduction
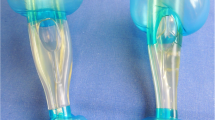
Intubation with a laryngeal tube (LT) is a recommended alternative to endotracheal intubation during advanced life support (ALS). LT insertion is easy; therefore, it may also be an alternative to bag-mask ventilation (BMV) for untrained personnel performing basic life support (BLS). Data from manikin studies support the influence of LT on no-flow-time (NFT) during ALS.
Methods
We performed a prospective, randomized manikin study using a two-rescuer model to compare the effects of ventilation using a LT and BMV on NFT during BLS. Participants were trained in BMV and were inexperienced in the use of a LT.
Results
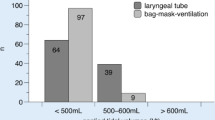
There was no significant difference in total NFT with the use of a LT and BMV (LT: mean 83.1 ± 37.3 s; BMV: mean 78.7 ± 24.5 s; p = 0.313), but we found significant differences in the progression of the scenario: in the BLS-scenario, the proportion of time spent performing chest compressions was higher when BMV was used compared to when a LT was used. The quality of chest compressions and the ventilation rate did not differ significantly between the two groups. The mean tidal volume and mean minute volume were significantly larger with the use of a LT compared with the use of BMV.
Conclusions
In conclusion, in a two-rescuer BLS scenario, NFT is longer with the use of a LT (without prior training) than with the use of BMV (with prior training). The probable reasons for this result are higher tidal volumes with the use of a LT leading to longer interruptions without chest compressions.
Zusammenfassung
Hintergrund
Der Larynx-Tubus (LT) ist eine empfohlene Alternative zur endotrachealen Intubation im Rahmen von erweiterten Reanimationsmaßnahmen (Advanced Life Support, ALS). Die Insertion des Devices ist einfach, daher ist sein Einsatz auch als Alternative zur Beutel-Masken-Beatmung (Beutel-Masken-Ventilation, BMV) für ungeübtes Personal im Rahmen von Basis-Reanimationsmaßnahmen (Basic Life Support, BLS) denkbar. Daten unterstützen zudem einen positiven Einfluss des LT auf die No-Flow-Time (NFT) beim ALS in Manikin-Studien.
Material und Methoden
Wir untersuchten den Einfluss des LT auf die NFT und die Qualität der Beatmung beim BLS im Vergleich zur BMV im Rahmen einer prospektiven, randomisierten Manikin-Studie im Zwei-Helfer-Modell. Die Probanden waren in BMV ausgebildet, jedoch unerfahren in der Anwendung eines LT.
Ergebnisse
Es zeigte sich kein signifikanter Unterschied in der absoluten NFT (LT: 83,1 ± 37,3 s; BMV: 78,7 ± 24,5 s; p = 0,313). Bei Betrachtung der späteren Zeitabschnitte des Reanimationsverlaufs zeigten sich signifikante Unterschiede: der zeitliche Anteil an Herzdruckmassage stieg unter BMV stetig an, während sich dieser bei Anwendung des LT verringerte. Die Qualität der Herzdruckmassage und die Beatmungsfrequenz unterschieden sich nicht signifikant. Die durchschnittlichen Tidalvolumina sowie Atemminutenvolumina zeigten sich deutlich größer bei Beatmung mit dem LT.
Schlussfolgerungen
Die Anwendung des LT durch ungeübtes Personal im Rahmen des BLS im Zwei-Helfer-Modell führt im Vergleich zur geübten BMV zu einer Verlängerung der NFT. Eine wahrscheinliche Erklärung für dieses Ergebnis sind höhere Tidalvolumina, die zu längeren Unterbrechungen ohne Herzdruckmassage führten.


Similar content being viewed by others
References
Martens E, Sinner MF, Siebermair J, Raufhake C, Beckmann BM, Veith S, Duvel D, Steinbeck G, Kaab S (2014) Incidence of sudden cardiac death in Germany: results from an emergency medical service registry in Lower Saxony. Europace 12:1752–1758
Koster RW, Baubin MA, Bossaert LL, Caballero A, Cassan P, Castren M, Granja C, Handley AJ, Monsieurs KG, Perkins GD, Raffay V, Sandroni C (2010) European Resuscitation Council Guidelines for Resuscitation 2010 Section 2. Adult basic life support and use of automated external defibrillators. Resuscitation 81:1277–1292
Nordberg P, Hollenberg J, Herlitz J, Rosenqvist M, Svensson L (2009) Aspects on the increase in bystander CPR in Sweden and its association with outcome. Resuscitation 80:329–333
Deakin CD, Nolan JP, Soar J, Sunde K, Koster RW, Smith GB, Perkins GD (2010) European Resuscitation Council Guidelines for Resuscitation 2010 Section 4. Adult advanced life support. Resuscitation 81:1305–1352
Wik L, Kramer-Johansen J, Myklebust H, Sorebo H, Svensson L, Fellows B, Steen PA (2005) Quality of cardiopulmonary resuscitation during out-of-hospital cardiac arrest. JAMA 293:299–304
Cheskes S, Schmicker RH, Christenson J, Salcido DD, Rea T, Powell J, Edelson DP, Sell R, May S, Menegazzi JJ, Van Ottingham L, Olsufka M, Pennington S, Simonini J, Berg RA, Stiell I, Idris A, Bigham B, Morrison L (2011) Perishock pause: an independent predictor of survival from out-of-hospital shockable cardiac arrest. Circulation 124:58–66
Berg RA, Kern KB, Sanders AB, Otto CW, Hilwig RW, Ewy GA (1993) Bystander cardiopulmonary resuscitation. Is ventilation necessary? Circulation 88:1907–1915
Hallstrom A, Cobb L, Johnson E, Copass M (2000) Cardiopulmonary resuscitation by chest compression alone or with mouth-to-mouth ventilation. N Engl J Med 342:1546–1553
Hüpfl M, Selig HF, Nagele P (2010) Chest-compression-only versus standard cardiopulmonary resuscitation: a meta-analysis. Lancet 376:1552–1557
Iwami T, Kawamura T, Hiraide A, Berg RA, Hayashi Y, Nishiuchi T, Kajino K, Yonemoto N, Yukioka H, Sugimoto H, Kakuchi H, Sase K, Yokoyama H, Nonogi H (2007) Effectiveness of bystander-initiated cardiac-only resuscitation for patients with out-of-hospital cardiac arrest. Circulation 116:2900–2907
Deakin CD, O’Neill JF, Tabor T (2007) Does compression-only cardiopulmonary resuscitation generate adequate passive ventilation during cardiac arrest? Resuscitation 75:53–59
Handley AJ (2009) Compression-only CPR—to teach or not to teach? Resuscitation 80:752–754
Rea TD, Fahrenbruch C, Culley L, Donohoe RT, Hambly C, Innes J, Bloomingdale M, Subido C, Romines S, Eisenberg MS (2010) CPR with chest compression alone or with rescue breathing. N Engl J Med 363:423–433
Svensson L, Bohm K, Castren M, Pettersson H, Engerstrom L, Herlitz J, Rosenqvist M (2010) Compression-only CPR or standard CPR in out-of-hospital cardiac arrest. N Engl J Med 363:434–442
Lee HM, Cho KH, Choi YH, Yoon SY, Choi YH (2008) Can you deliver accurate tidal volume by manual resuscitator? Emerg Med J 25:632–634
Lockey D, Lossius HM (2014) Pre-hospital airway management: the data grows rapidly but controversy remains. Resuscitation 85:849–850
Soar J, Nolan JP (2013) Airway management in cardiopulmonary resuscitation. Curr Opin Crit Care 19:181–187
Wiese CH, Semmel T, Muller JU, Bahr J, Ocker H, Graf BM (2009) The use of the laryngeal tube disposable (LT-D) by paramedics during out-of-hospital resuscitation-an observational study concerning ERC guidelines 2005. Resuscitation 80:194–198
Schwarzkopf K (2012) Supraglottic airway devices. Med Klin Intensivmed Notfmed 107:531–536
Ostermayer DG, Gausche-Hill M (2014) Supraglottic airways: the history and current state of prehospital airway adjuncts. Prehosp Emerg Care 18:106–115
Honold J, Hodrius J, Schwietz T, Bushoven P, Zeiher AM, Fichtlscherer S, Seeger FH (2015) [Aspiration and pneumonia risk after preclinical invasive resuscitation: endotracheal intubation and supraglottic airway management with the laryngeal tube S]. Med Klin Intensivmed Notfmed (in press). doi:10.1007/s00063–015-0018-y
Castle N, Owen R, Hann M, Naidoo R, Reeves D (2010) Assessment of the speed and ease of insertion of three supraglottic airway devices by paramedics: a manikin study. Emerg Med J 27:860–863
Jänig C, Nitsche T, Kwiecien R, Dietze T, Lischke H (2012) Atemwegssicherung: Nur etwas für Experten? Notfall Rettungsmed 15:218–224
Huter L, Schwarzkopf K, Rodiger J, Preussler NP, Schreiber T (2009) Students insert the laryngeal tube quicker and more often successful than the esophageal-tracheal combitube in a manikin. Resuscitation 80:930–934
Jokela J, Nurmi J, Genzwuerker HV, Castren M (2009) Laryngeal tube and intubating laryngeal mask insertion in a manikin by first-responder trainees after a short video-clip demonstration. Prehosp Disaster Med 24:63–66
Lankimaki S, Alahuhta S, Kurola J (2013) Feasibility of a laryngeal tube for airway management during cardiac arrest by first responders. Resuscitation 84:446–449
Asai T, Kawachi S (2004) Use of the laryngeal tube by paramedic staff. Anaesthesia 59(4):408–409
Voscopoulos C, Barker T, Listwa T, Nelson S, Pozner C, Liu X, Zane R, Antoine JA (2013) A comparison of the speed, success rate, and retention of rescue airway devices placed by first-responder emergency medical technicians: a high-fidelity human patient simulation study. J Emerg Med 44:784–789
Ruetzler K, Roessler B, Potura L, Priemayr A, Robak O, Schuster E, Frass M (2011) Performance and skill retention of intubation by paramedics using seven different airway devices—a manikin study. Resuscitation 82:593–597
Mitchell MS, Lee White M, King WD, Wang HE (2012) Paramedic King Laryngeal Tube airway insertion versus endotracheal intubation in simulated pediatric respiratory arrest. Prehosp Emerg Care 16:284–288
Asai T, Hidaka I, Kawachi S (2002) Efficacy of the laryngeal tube by inexperienced personnel. Resuscitation 55:171–175
Kurola J, Paakkonen H, Kettunen T, Laakso JP, Gorski J, Silfvast T (2011) Feasibility of written instructions in airway management training of laryngeal tube. Scand J Trauma Resusc Emerg Med 19:56
Wiese CH, Bartels U, Bergmann A, Bergmann I, Bahr J, Graf BM (2008) Using a laryngeal tube during cardiac arrest reduces “no flow time” in a manikin study: a comparison between laryngeal tube and endotracheal tube. Wien Klin Wochenschr 120:217–223
Wiese CH, Bahr J, Bergmann A, Bergmann I, Bartels U, Graf BM (2008) [Reduction in no flow time using a laryngeal tube: comparison to bag-mask ventilation]. Anaesthesist 57:589–596
Jensen JL, Walker M, LeRoux Y, Carter A (2013) Chest compression fraction in simulated cardiac arrest management by primary care paramedics: King laryngeal tube airway versus basic airway management. Prehosp Emerg Care 17:285–290
Kurola J, Harve H, Kettunen T, Laakso JP, Gorski J, Paakkonen H, Silfvast T (2004) Airway management in cardiac arrest—comparison of the laryngeal tube, tracheal intubation and bag-valve mask ventilation in emergency medical training. Resuscitation 61:149–153
Genzwuerker HV, Finteis T, Slabschi D, Groeschel J, Ellinger K (2001) Assessment of the use of the laryngeal tube for cardiopulmonary resuscitation in a manikin. Resuscitation 51:291–296
Herff H, Bowden K, Paal P, Mitterlechner T, von Goedecke A, Lindner KH, Wenzel V (2009) Effect of decreased inspiratory times on tidal volume. Bench model simulating cardiopulmonary resuscitation. Anaesthesist 58:686–690
Mahony PH, Griffiths RF, Larsen P, Powell D (2008) Retention of knowledge and skills in first aid and resuscitation by airline cabin crew. Resuscitation 76:413–418
Schalte G, Stoppe C, Aktas M, Coburn M, Rex S, Schwarz M, Rossaint R, Zoremba N (2011) Laypersons can successfully place supraglottic airways with 3 min of training. A comparison of four different devices in the manikin. Scand J Trauma Resusc Emerg Med 19:60
Trabold B, Schmidt C, Schneider B, Akyol D, Gutsche M (2008) Application of three airway devices during emergency medical training by health care providers—a manikin study. Am J Emerg Med 26:783–788
Kette F, Reffo I, Giordani G, Buzzi F, Borean V, Cimarosti R, Codiglia A, Hattinger C, Mongiat A, Tararan S (2005) The use of laryngeal tube by nurses in out-of-hospital emergencies: preliminary experience. Resuscitation 66:21–25
Hubble MW, Wilfong DA, Brown LH, Hertelendy A, Benner RW (2010) A meta-analysis of prehospital airway control techniques part II: alternative airway devices and cricothyrotomy success rates. Prehosp Emerg Care 14:515–530
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
J. Schröder, M. Bucher, and O. Meyer state that there are no conflicts of interest.
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975 (in its most recently amended version). Informed consent was obtained from all patients included in the study.
Additional information
Redaktion
M. Buerke, Siegen
Rights and permissions
About this article
Cite this article
Schröder, J., Bucher, M. & Meyer, O. Effect of the laryngeal tube on the no-flow-time in a simulated two rescuer basic life support setting with inexperienced users. Med Klin Intensivmed Notfmed 111, 493–500 (2016). https://doi.org/10.1007/s00063-015-0088-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00063-015-0088-x
Keywords
- No-flow-time
- Cardiopulmonary resuscitation (CPR)
- Basic life support (BLS)
- Laryngeal
- Tube (LT)
- Manikin study