Abstract
Purpose
The utility of preoperative embolization (PE) of intracranial meningiomas is unclear and controversial. The aim of this study was to investigate the effect of PE on meningioma surgical resection by completing a meta-analysis of matched cohort studies.
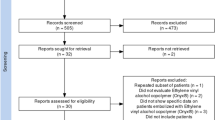
Methods
A systematic review and meta-analysis of matched cohort studies was completed to evaluate the effect of PE on meningioma resection and outcomes. Outcome measures included: intraoperative blood loss, major surgical complications, total surgical complications including minor ones, total major complications including major surgical and embolization complications, total overall complications, and postoperative functional independence defined as modified Rankin Score (mRS) of 0–2. Pooled odds ratios (OR) were determined via a fixed effects model.
Results
A total of 6 matched cohort studies were identified with 219 embolized and 215 non-embolized meningiomas. There was no significant difference in intraoperative blood loss between the two groups (P = 0.87); however, the embolization group had a significantly lower odds ratio of major surgically related complications (OR: 0.37, 95% confidence interval, CI: 0.21–0.67, P = 0.0009, I2 = 0%), but no difference in minor surgical complications (P = 0.86). While there was a significantly lower odds ratio of total overall surgical and PE-related complications in PE cases (OR: 0.64, CI: 0.41–1.0, P = 0.05, I2 = 66%), there was no difference in total combined major complications between the groups (OR: 0.57, CI: 0.27–1.18, P = 0.13, I2 = 33%). Lastly, PE was associated with a higher odds ratio of functional independence on postoperative follow-up (OR: 2.3, CI: 1.06–5.02, P = 0.04, I2 = 0%).
Conclusion
For certain meningiomas, PE facilitates lower overall complications, lower major surgical complications, and improved functional independence. Further research is required to identify the particular subset of meningiomas that benefit from PE.






Similar content being viewed by others
References
Manaka H, Sakata K, Tatezuki J, Shinohara T, Shimohigoshi W, Yamamoto T. Safety and efficacy of preoperative embolization in patients with meningioma. J Neurol Surg B Skull Base. 2018;79(Suppl 4):s328–33. https://doi.org/10.1055/s-0038-1667043.
Chen L, Li DH, Lu YH, Hao B, Cao YQ. Preoperative embolization versus direct surgery of meningiomas: a meta-analysis. World Neurosurg. 2019;128:62–8. https://doi.org/10.1016/j.wneu.2019.02.223.
Bendszus M, Klein R, Burger R, Warmuth-Metz M, Hofmann E, Solymosi L. Efficacy of trisacryl gelatin microspheres versus polyvinyl alcohol particles in the preoperative embolization of meningiomas. AJNR Am J Neuroradiol. 2000;21(2):255–61.
Bendszus M, Rao G, Burger R, Schaller C, Scheinemann K, Warmuth-Metz M, Hofmann E, Schramm J, Roosen K, Solymosi L. Is there a benefit of preoperative meningioma embolization? Neurosurgery. 2000;47(6):1306–11. discussion 1311–2.
Wirsching HG, Richter JK, Sahm F, Morel C, Krayenbuehl N, Rushing EJ, von Deimling A, Valavanis A, Weller M. Post-operative cardiovascular complications and time to recurrence in meningioma patients treated with versus without pre-operative embolization: a retrospective cohort study of 741 patients. J Neurooncol. 2018;140(3):659–67. https://doi.org/10.1007/s11060-018-2996-0.
Iacobucci M, Danieli L, Visconti E, Maresca M, Anile C, Colosimo C, Pedicelli A. Preoperative embolization of meningiomas with polyvinyl alcohol particles: The benefits are not outweighed by risks. Diagn Interv Imaging. 2017;98(4):307–14. https://doi.org/10.1016/j.diii.2016.08.006.
Jumah F, AbuRmilah A, Raju B, Jaber S, Adeeb N, Narayan V, Sun H, Cuellar H, Gupta G, Nanda A. Does preoperative embolization improve outcomes of meningioma resection? A systematic review and meta-analysis. Neurosurg Rev. 2021;44(6):3151–63. https://doi.org/10.1007/s10143-021-01519-z.
Yin Y, Li Y, Jiang Z, Zhang C, Ge H, Chen Z, Hu R, Chen Y, Li X, Li F, Feng H. Clinical Outcomes and Complications of Preoperative Embolization for Intracranial Giant Meningioma Tumorectomy: A Retrospective, Observational, Matched Cohort Study. Front Oncol. 2022;12:852327. https://doi.org/10.3389/fonc.2022.852327.
Akimoto T, Ohtake M, Miyake S, Suzuki R, Iida Y, Shimohigoshi W, Higashijima T, Nakamura T, Shimizu N, Kawasaki T, Sakata K, Yamamoto T. Preoperative tumor embolization prolongs time to recurrence of meningiomas: a retrospective propensity-matched analysis. J Neurointerv Surg. 2022; https://doi.org/10.1136/neurintsurg-2022-019080. Epub ahead of print.
Przybylowski CJ, Zhao X, Baranoski JF, Borba Moreira L, Gandhi S, Chapple KM, Almefty KK, Sanai N, Ducruet AF, Albuquerque FC, Little AS, Nakaji P. Preoperative embolization versus no embolization for WHO grade I intracranial meningioma: a retrospective matched cohort study. J Neurosurg. 2020;134(3):693–700. https://doi.org/10.3171/2020.1.JNS19788.
Banks JL, Marotta CA. Outcomes validity and reliability of the modified Rankin scale: implications for stroke clinical trials: a literature review and synthesis. Stroke. 2007;38(3):1091–6. https://doi.org/10.1161/01.STR.0000258355.23810.c6.
Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA (editors). Cochrane Handbook for Systematic Reviews of Interventions. 2nd Edition. Chichester (UK): John Wiley & Sons; 2019.
Al-Mufti F, Gandhi CD, Couldwell WT, Rybkin I, Abou-Al-Shaar H, Dodson V, Amin AG, Wainwright JV, Cohen E, Schmidt MH, Cole C, Bowers CA. Preoperative meningioma embolization reduces perioperative blood loss: a multi-center retrospective matched case-control study. Br J Neurosurg. 2021;27:1–4. https://doi.org/10.1080/02688697.2021.1979191.
Oka H, Kurata A, Kawano N, Saegusa H, Kobayashi I, Ohmomo T, Miyasaka Y, Fujii K. Preoperative superselective embolization of skull-base meningiomas: indications and limitations. J Neurooncol. 1998;40(1):67–71. https://doi.org/10.1023/a:1006196420398.
Dean BL, Flom RA, Wallace RC, Khayata MH, Obuchowski NA, Hodak JA, Zabramski JM, Spetzler RF. Efficacy of endovascular treatment of meningiomas: evaluation with matched samples. AJNR Am J Neuroradiol. 1994;15(9):1675–80.
Raper DM, Starke RM, Henderson F Jr, Ding D, Simon S, Evans AJ, Jane JA Sr, Liu KC. Preoperative embolization of intracranial meningiomas: efficacy, technical considerations, and complications. AJNR Am J Neuroradiol. 2014;35(9):1798–804. https://doi.org/10.3174/ajnr.A3919.
Barros G, Feroze AH, Sen R, Kelly CM, Barber J, Hallam DK, Ghodke B, Osbun JW, Kim LJ, Levitt MR. Predictors of preoperative endovascular embolization of meningiomas: subanalysis of anatomic location and arterial supply. J Neurointerv Surg. 2020;12(2):204–8. https://doi.org/10.1136/neurintsurg-2019-015129.
Borg A, Ekanayake J, Mair R, Smedley T, Brew S, Kitchen N, Samandouras G, Robertson F. Preoperative particle and glue embolization of meningiomas: indications, results, and lessons learned from 117 consecutive patients. Neurosurgery. 2013;73(2 Suppl Operative):244–51. https://doi.org/10.1227/NEU.0000000000000187. discussion ons252.
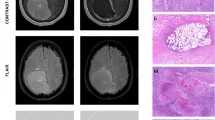
ElBeheiry AA, Fayed AA, Alkassas AH, Emara DM. Can magnetic resonance imaging predict preoperative consistency and vascularity of intracranial meningioma? Egypt J Radiol Nucl Med. 2022;53(1):1–5.
Nania A, Granata F, Vinci S, Pitrone A, Barresi V, Morabito R, Settineri N, Tomasello F, Alafaci C, Longo M. Necrosis score, surgical time, and transfused blood volume in patients treated with preoperative embolization of intracranial meningiomas. Analysis of a single-centre experience and a review of literature. Clin Neuroradiol. 2014;24(1):29–36. https://doi.org/10.1007/s00062-013-0215-0.
Ilyas A, Przybylowski C, Chen CJ, Ding D, Foreman PM, Buell TJ, Taylor DG, Kalani MY, Park MS. Preoperative embolization of skull base meningiomas: A systematic review. J Clin Neurosci. 2019;59:259–64. https://doi.org/10.1016/j.jocn.2018.06.022.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
D. Schartz, T. Furst, N. Ellens, G.S. Kohli, R. Rahmani, S.M.K. Akkipeddi, T. Schmidt, T. Bhalla, T. Mattingly and M.T. Bender declare that they have no competing interests. The authors have no relevant financial or non-financial interests to disclose.
Ethical standards
The authors certify that this manuscript conforms to the International Committee of Medical Journal Editors (ICMJE) recommendations for conduct, reporting, editing, and publication of scholarly work in medical journals and is hereby ethically sound.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Schartz, D., Furst, T., Ellens, N. et al. Preoperative Embolization of Meningiomas Facilitates Reduced Surgical Complications and Improved Clinical Outcomes. Clin Neuroradiol 33, 755–762 (2023). https://doi.org/10.1007/s00062-023-01272-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00062-023-01272-4