Abstract
Purpose
To quantify the influence of melanin content on magnetic susceptibility of cerebral melanoma metastases.
Methods
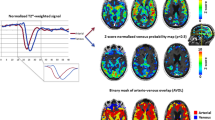
Patients with non-hemorrhagic metastases were included based on the absence of susceptibility blooming artifacts. Susceptibility maps were calculated from 3D gradient echo data, using Laplacian-based phase unwrapping, sophisticated harmonic artefact reduction for phase data (V-SHARP) with varying spherical kernel sizes for background field removal and the iLSQR algorithm for the inversion of phase data. Susceptibility maps were referenced to cerebrospinal fluid. Non-hemorrhagic metastases were identified on contrast-enhanced T1-weighted images and susceptibility weighted images. Metastases masks were drawn on T1-weighted post-contrast images and used to compute mean susceptibility values of each metastasis.
Results
A total of 33 non-hemorrhagic melanoma brain metastases in 20 patients were quantitatively evaluated. Metastases without and with hyperintense signal on T1-weighted images, which corresponds to the melanin content, showed median susceptibility values of −0.028 ppm and −0.020 ppm, respectively. The susceptibility differences between metastases without and with T1-weighted hyperintense signal was not statistically significant (p ≥ 0.05).
Conclusion
Non-hemorrhagic cerebral melanoma metastases showed weak diamagnetic susceptibility values and susceptibility did not significantly correlate to T1-weighted signals. Therefore, melanin does not seem to be a major contributor to susceptibility in cerebral melanoma metastases.





Similar content being viewed by others
References:
Barnholtz-Sloan JS, Sloan AE, Davis FG, Vigneau FD, Lai P, Sawaya RE. Incidence proportions of brain metastases in patients diagnosed (1973 to 2001) in the Metropolitan Detroit Cancer Surveillance System. J Clin Oncol. 2004;22:2865–72.
Brożyna AA, Jóźwicki W, Roszkowski K, Filipiak J, Slominski AT. Melanin content in melanoma metastases affects the outcome of radiotherapy. Oncotarget. 2016;7:17844–53.
Fearnley JM, Lees AJ. Ageing and Parkinson’s disease: substantia nigra regional selectivity. Brain. 1991;114:2283–301.
Escott EJ. A variety of appearances of malignant melanoma in the head: a review. Radiographics. 2001;21:625–39.
Woodruff WW Jr., Djang WT, McLendon RE, Heinz ER, Voorhees DR. Intracerebral malignant melanoma: high-field-strength MR imaging. Radiology. 1987;165:209–13.
Atlas SW, Grossman RI, Gomori JM, Guerry D, Hackney DB, Goldberg HI, Zimmerman RA, Bilaniuk LT. MR imaging of intracranial metastatic melanoma. J Comput Assist Tomogr. 1987;11:577–82.
Isiklar I, Leeds NE, Fuller GN, Kumar AJ. Intracranial metastatic melanoma: correlation between MR imaging characteristics and melanin content. AJR Am J Roentgenol. 1995;165:1503–12.
Enochs WS, Hyslop WB, Bennett HF, Brown RD 3rd, Koenig SH, Swartz HM. Sources of the increased longitudinal relaxation rates observed in melanotic melanoma. An in vitro study of synthetic melanins. Invest Radiol. 1989;24:794–804.
Gramsch C, Göricke SL, Behrens F, Zimmer L, Schadendorf D, Krasny A, Forsting M, Schlamann MU. Isolated cerebral susceptibility artefacts in patients with malignant melanoma: metastasis or not? Eur Radiol. 2013;23:2622–7.
Parizel PM, Makkat S, Van Miert E, Van Goethem JW, van den Hauwe L, De Schepper AM. Intracranial hemorrhage: principles of CT and MRI interpretation. Eur Radiol. 2001;11:1770–83.
Haacke EM, Liu S, Buch S, Zheng W, Wu D, Ye Y. Quantitative susceptibility mapping: current status and future directions. Magn Reson Imaging. 2015;33:1–25.
Chen W, Gauthier SA, Gupta A, Comunale J, Liu T, Wang S, Pei M, Pitt D, Wang Y. Quantitative susceptibility mapping of multiple sclerosis lesions at various ages. Radiology. 2014;271:183–92.
Liu T, Eskreis-Winkler S, Schweitzer AD, Chen W, Kaplitt MG, Tsiouris AJ, Wang Y. Improved subthalamic nucleus depiction with quantitative susceptibility mapping. Radiology. 2013;269:216–23.
Wharton S, Bowtell R. Effects of white matter microstructure on phase and susceptibility maps. Magn Reson Med. 2015;73:1258–69.
Langkammer C, Schweser F, Krebs N, Deistung A, Goessler W, Scheurer E, Sommer K, Reishofer G, Yen K, Fazekas F, Ropele S, Reichenbach JR. Quantitative susceptibility mapping (QSM) as a means to measure brain iron? A post mortem validation study. Neuroimage. 2012;62:1593–9.
Deistung A, Schweser F, Wiestler B, Abello M, Roethke M, Sahm F, Wick W, Nagel AM, Heiland S, Schlemmer HP, Bendszus M, Reichenbach JR, Radbruch A. Quantitative susceptibility mapping differentiates between blood depositions and calcifications in patients with Glioblastoma. PLoS One. 2013;8:e57924. https://doi.org/10.1371/journal.pone.0057924
Liu S, Mok K, Neelavalli J, Cheng YC, Tang J, Ye Y, Haacke EM. Improved MR Venography using quantitative susceptibility-weighted imaging. J Magn Reson Imaging. 2014;40:698–708.
Prock T, Collins DJ, Dzik-Jurasz ASK, Leach MO. An algorithm for the optimum combination of data from arbitrary magnetic resonance phased array probes. Phys Med Biol. 2002;47:N39–46.
Smith SM. Fast robust automated brain extraction. Hum Brain Mapp. 2002;17:143–55.
Li W, Avram AV, Wu B, Xiao X, Liu CL. Integrated Laplacian-based phase unwrapping and background phase removal for quantitative susceptibility mapping. NMR Biomed. 2014;27:219–27.
Wu B, Li W, Guidon A, Liu CL. Whole brain susceptibility mapping using compressed sensing. Magn Reson Med. 2012;67:137–47.
Li W, Wu B, Liu CL. Quantitative susceptibility mapping of human brain reflects spatial variation in tissue composition. Neuroimage. 2011;55:1645–56.
Li W, Wang N, Yu F, Han H, Cao W, Romero R, Tantiwongkosi B, Duong TQ, Liu C. A method for estimating and removing streaking artifacts in quantitative susceptibility mapping. Neuroimage. 2015;108:111–22.
Straub S, Schneider TM, Emmerich J, Freitag MT, Ziener CH, Schlemmer HP, Ladd ME, Laun FB. Suitable reference tissues for quantitative susceptibility mapping of the brain. Magn Reson Med. 2017;78:204–14.
Patenaude B, Smith SM, Kennedy DN, Jenkinson M. A Bayesian model of shape and appearance for subcortical brain segmentation. Neuroimage. 2011;56:907–22.
Deistung A, Schäfer A, Schweser F, Biedermann U, Turner R, Reichenbach JR. Toward in vivo histology: a comparison of quantitative susceptibility mapping (QSM) with magnitude-, phase-, and R2*-imaging at ultra-high magnetic field strength. Neuroimage. 2013;65:299–314.
Nolden M, Zelzer S, Seitel A, Wald D, Müller M, Franz AM, Maleike D, Fangerau M, Baumhauer M, Maier-Hein L, Maier-Hein KH, Meinzer HP, Wolf I. The Medical Imaging Interaction Toolkit: challenges and advances. Int J Comput Assist Radiol Surg. 2013;8:607–20.
Ellingson BM, Zaw T, Cloughesy TF, Naeini KM, Lalezari S, Mong S, Lai A, Nghiemphu PL, Pope WB. Comparison between intensity normalization techniques for dynamic susceptibility contrast (DSC)-MRI estimates of cerebral blood volume (CBV) in human gliomas. J Magn Reson Imaging. 2012;35:1472–7.
Pizzichetta MA, Talamini R, Stanganelli I, Puddu P, Bono R, Argenziano G, Veronesi A, Trevisan G, Rabinovitz H, Soyer HP. Amelanotic/hypomelanotic melanoma: clinical and dermoscopic features. Brit J Dermatol. 2004;150:1117–24.
Franceschi AM, Moschos SJ, Anders CK, Glaubiger S, Collichio FA, Lee CB, Castillo M, Lee YZ. Use of Susceptibility-Weighted Imaging (SWI) in the Detection of Brain Hemorrhagic Metastases from Breast Cancer and Melanoma. J Comput Assist Tomogr. 2016;40:803–5.
Gaviani P, Mullins ME, Braga TA, Hedley-Whyte ET, Halpern EF, Schaefer PS, Henson JW. Improved detection of metastatic melanoma by T2(*)-weighted imaging. AJNR Am J Neuroradiol. 2006;27:605–8.
Langkammer C, Krebs N, Goessler W, Scheurer E, Yen K, Fazekas F, Ropele S. Susceptibility induced gray-white matter MRI contrast in the human brain. Neuroimage. 2012;59:1413–9.
Wharton S, Bowtell R. Fiber orientation-dependent white matter contrast in gradient echo MRI. Proc Natl Acad Sci USA. 2012;109:18559–64.
Drayer B, Burger P, Darwin R, Riederer S, Herfkens R, Johnson GA. MRI of Brain Iron. AJR Am J Roentgenol. 1986;147:103–10.
Riley PA. Melanin. Int J Biochem Cell Biol. 1997;29:1235–9.
Ito S, Jimbow K. Quantitative-analysis of Eumelanin and Pheomelanin in hair and melanomas. J Investig Dermatol. 1983;80:268–72.
Bush WD, Garguilo J, Zucca FA, Albertini A, Zecca L, Edwards GS, Nemanich RJ, Simon JD. The surface oxidation potential of human neuromelanin reveals a spherical architecture with a pheomelanin core and a eumelanin surface. Proc Natl Acad Sci USA. 2006;103:14785–9.
Enochs WS, Nilges MJ, Swartz HM. Purified human Neuromelanin, synthetic Dopamine melanin as a potential model pigment, and the normal human Substantia-Nigra—characterization by electron-Paramagnetic-resonance spectroscopy. J Neurochem. 1993;61:68–79.
Zecca L, Gallorini M, Schünemann V, Trautwein AX, Gerlach M, Riederer P, Vezzoni P, Tampellini D. Iron, neuromelanin and ferritin content in the substantia nigra of normal subjects at different ages: consequences for iron storage and neurodegenerative processes. J Neurochem. 2001;76:1766–73.
Trujillo P, Summers PE, Ferrari E, Zucca FA, Sturini M, Mainardi LT, Cerutti S, Smith AK, Smith SA, Zecca L, Costa A. Contrast mechanisms associated with Neuromelanin-MRI. Magn Reson Med. 2017;78:1790–800.
Li Y, Xie Y, Wang Z, Zang N, Carniato F, Huang Y, Andolina CM, Parent LR, Ditri TB, Walter ED, Botta M, Rinehart JD, Gianneschi NC. Structure and function of iron-loaded synthetic melanin. ACS Nano. 2016;10:10186–94.
Enochs WS, Petherick P, Bogdanova A, Mohr U, Weissleder R. Paramagnetic metal scavenging by melanin: MR imaging. Radiology. 1997;204:417–23.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
S. Straub, F.B. Laun, M.T. Freitag, C. Kölsche, A. von Deimling, M. Denoix, M. Bendszus, H.-P. Schlemmer, M.E. Ladd and T.M. Schneider declare that they have no competing interests.
Rights and permissions
About this article
Cite this article
Straub, S., Laun, F.B., Freitag, M.T. et al. Assessment of Melanin Content and its Influence on Susceptibility Contrast in Melanoma Metastases. Clin Neuroradiol 30, 607–614 (2020). https://doi.org/10.1007/s00062-019-00816-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00062-019-00816-x