Abstract
Purpose
Assuming thromboembolic events to be the origin of silent strokes during cerebral digital subtraction angio-graphy (DSA), antiplatelet therapy with acetylsalicylic acid (ASA) should significantly reduce the risk for DSA-related silent stroke. The aim of this retrospective analysis was to assess whether ASA does prevent DSA-related silent stroke in terms of high signal intensity lesions in diffusion-weighted magnetic resonance imaging (DW-MRI).
Methods
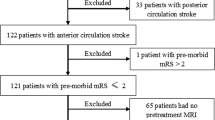
All patients underwent a baseline DW-MRI 24 h before DSA and a follow-up DW-MRI 3–24 h after DSA. Patients were considered to have an acute (silent) infarction caused by DSA if there was at least one hyperintense lesion of at least 1 mm in diameter and no neurological deficits.
Results
Out of 52 patients in the ASA group 11 (21.2%) had high signal lesions on DW-MRI and 20 out of 123 (16.3%) in the non-ASA group. No significant relationship between the ASA and non-ASA group and the post-angiographic appearance of high signal intensity lesions in DW-MRI could be found (Wilcoxon 2-sample test: p-value 0.9).
Conclusions
The use of oral antiplatelet therapy by ASA (100 mg/day) in cerebrovascular patients did not prevent DSA-related high signal intensity lesions in DW-MRI in this study. Despite a potential bias of this retrospective analysis the findings challenge the current theory of thromboembolisms being the predominant origin of silent stroke. The findings therefore support alternative hypotheseses of the etiology of silent strokes, such as air embolism and mobilized embolic material by the catheter at the vessel wall.

Similar content being viewed by others
References
Kaufmann TJ, Huston J 3rd, Mandrekar JN, Schleck CD, Thielen KR, Kallmes DF. Complications of diagnostic cerebral angiography: evaluation of 19,826 consecutive patients. Radiology. 2007;3:812–9.
Chuah KC, Stuckey SL, Berman IG. Silent embolism in diagnostic cerebral angiography: detection with diffusion-weighted imaging. Australas Radiol. 2004;2:133–8.
Kato K, Tomura N, Takahashi S, Sakuma I, Watarai J. Ischemic lesions related to cerebral angiography: evaluation by diffusion-weighted MR imaging. Neuroradiology. 2003;1:39–43.
Koch C, Kucinski T, Eckert B, Wittkugel O, Rother J, Zeumer H. Endovascular therapy of high-degree stenoses of the neck vessels-stent-supported percutaneous angioplasty of the carotid artery without cerebral protection. Rofo. 2002;12:1506–10.
Britt PM, Heiserman JE, Snider RM, Shill HA, Bird CR, Wallace RC. Incidence of postangiographic abnormalities revealed by diffusion-weighted MR imaging. AJNR Am J Neuroradiol. 2000;1:55–9.
Beauchamp NJ, Ulug AM, Passe TJ, van Zijl PC. MR diffusion imaging in stroke: review and controversies. Radiographics. 1998;5:1269–83.
Bendszus M, Koltzenburg M, Burger R, Warmuth-Metz M, Hofmann E, Solymosi L. Silent embolism in diagnostic cerebral angiography and neurointerventional procedures: a prospective study. Lancet. 1999;9190:1594–7.
Derdeyn CP. Diffusion-weighted imaging as a surrogate marker for stroke as a complication of cerebrovascular procedures and devices. AJNR Am J Neuroradiol. 2001;7:1234–5.
Hauth EAM, Jansen C, Drescher R, Schwartz M, Forsting M, Jaeger HJ, Mathias KD. MR and clinical follow-up of diffusion-weighted cerebral lesions after carotid artery stenting. AJNR Am J Neuroradiol. 2005;9:2336–41.
Jaeger HJ, Mathias KD, Hauth E, Drescher R, Gissler HM, Hennigs S, Christmann A. Cerebral ischemia detected with diffusion-weighted MR imaging after stent implantation in the carotid artery. AJNR Am J Neuroradiol. 2002;2:200–7.
Nitkunan A, Barrick TR, Charlton RA, Clark CA, Markus HS. Multimodal MRI in cerebral small vessel disease: its relationship with cognition and sensitivity to change over time. Stroke. 2008;7:1999–2005.
Bendszus M, Koltzenburg M, Bartsch AJ, Goldbrunner R, Gunthner-Lengsfeld T, Weilbach FX, Roosen K, Toyka KV, Solymosi L. Heparin and air filters reduce embolic events caused by intra-arterial cerebral angiography: a prospective, randomized trial. Circulation. 2004;15:2210–15.
Ginsberg LE, Stump DA, King JC, Deal DD, Moody DM. Air embolus risk with glass versus plastic syringes: in vitro study and implications for neuroangiography. Radiology. 1994;3:813–6.
Moody DM, Bell MA, Challa VR, Johnston WE, Prough DS. Brain microemboli during cardiac surgery or aortography. Ann Neurol. 1990;4:477–86.
Rordorf G, Bellon RJ, Budzik RF, Farkas J, Reinking GF, Pergolizzi RS, Ezzeddine M, Norbash AM, Gilberto Gonzalez R, Putman CM. Silent thromboembolic events associated with the treatment of unruptured cerebral aneurysms by use of Guglielmi detachable coils: prospective study applying diffusion-weighted imaging. AJNR Am J Neuroradiol. 2001;1:5–10.
Theron JG, Payelle GG, Coskun O, Huet HF, Guimaraens L. Carotid artery stenosis: treatment with protected balloon angioplasty and stent placement. Radiology. 1996;3:627–36.
Fiehler J, Ries T. Prevention and treatment of thromboembolism during endovascular aneurysm therapy. Clin Neuroradiol. 2009;1:73–81.
Debrun GM, Vinuela FV, Fox AJ. Aspirin and systemic heparinization in diagnostic and interventional neuroradiology. AJR Am J Roentgenol. 1982;1:139–42.
Willard JE, Lange RA, Hillis LD. The use of aspirin in ischemic heart disease. N Engl J Med. 1992;3:175–81.
Ries T, Buhk JH, Kucinski T, Goebell E, Grzyska U, Zeumer H, Fiehler J. Intravenous administration of acetylsalicylic acid during endovascular treatment of cerebral aneurysms reduces the rate of thromboembolic events. Stroke. 2006;7:1816–21.
Junghans U, Siebler M. Cerebral microembolism is blocked by tirofiban, a selective nonpeptide platelet glycoprotein IIb/IIIa receptor antagonist. Circulation. 2003;21:2717–21.
Feinberg WM, Seeger JF, Carmody RF, Anderson DC, Hart RG, Pearce LA. Epidemiologic features of asymptomatic cerebral infarction in patients with nonvalvular atrial fibrillation. Arch Intern Med. 1990;11:2340–44.
Hara M, Ooie T, Yufu K, Tsunematsu Y, Kusakabe T, Ooga M, Saikawa T, Sakata T. Silent cortical strokes associated with atrial fibrillation. Clin Cardiol. 1995;10:573–4.
Djaiani G, Fedorko L, Borger M, Mikulis D, Carroll J, Cheng D, Karkouti K, Beattie S, Karski J. Mild to moderate atheromatous disease of the thoracic aorta and new ischemic brain lesions after conventional coronary artery bypass graft surgery. Stroke. 2004;9:356–8.
Hougaku H, Matsumoto M, Handa N, Maeda H, Itoh T, Tsukamoto Y, Kamada T. Asymptomatic carotid lesions and silent cerebral infarction. Stroke. 1994;3:566–70.
Norris JW, Zhu CZ. Silent stroke and carotid stenosis. Stroke. 1992;4:483–5.
Bryan RN, Cai J, Burke G, Hutchinson RG, Liao D, Toole JF, Dagher AP, Cooper L. Prevalence and anatomic characteristics of infarct-like lesions on MR images of middle-aged adults: the atherosclerosis risk in communities study. AJNR Am J Neuroradiol. 1999;7:1273–80.
Bryan RN, Wells SW, Miller TJ, Elster AD, Jungreis CA, Poirier VC, Lind BK, Manolio TA. Infarct-like lesions in the brain: prevalence and anatomic characteristics at MR imaging of the elderly—data from the Cardiovascular Health Study. Radiology. 1997;1:47–54.
Fisher M, Sandler R, Weiner JM. Delayed cerebral ischemia following arteriography. Stroke. 1985;3:431–4.
Notsu Y, Nabika T, Park H-Y, Masuda J, Kobayashi S. Evaluation of genetic risk factors for silent brain infarction. Stroke. 1999;9:1881–6.
Gawel M, Burkett M, Rose FC. Platelet activation following cerebral angiography. Acta Neurol Scand. 1980;4:240–3.
Huckman MS, Shenk GI, Neems RL, Tinor T. Transfemoral cerebral arteriography versus direct percutaneous carotid and brachial arteriography: a comparison of complication rates. Radiology. 1979;1:93–7.
Kirino T. Ischemic tolerance. J Cereb Blood Flow Metab. 2002;11:1283–96.
Flach HZ, Ouhlous M, Hendriks JM, Van Sambeek MR, Veenland JF, Koudstaal PJ, Van Dijk LC, Van Der Lugt A. Cerebral ischemia after carotid intervention. J Endovasc Ther. 2004;3:251–7.
Garcia-Sanchez S, Millan-Torne M, Capellades-Font J, Muchart J, Callejas PJ, Vila-Moriente N. Ischemic brain lesions following carotid revascularisation procedures: a comparative study using diffusion-weighted magnetic resonance imaging. Rev Neurol. 2004;11:1013–7.
Poppert H, Wolf O, Resch M, Theiss W, Schmidt-Thieme T, Graefin von Einsiedel H, Heider P, Martinoff S, Sander D. Differences in number, size and location of intracranial microembolic lesions after surgical versus endovascular treatment without protection device of carotid artery stenosis. J Neurol. 2004;10:1198–203.
Roh HG, Byun HS, Ryoo JW, Na DG, Moon WJ, Lee BB, Kim DI. Prospective analysis of cerebral infarction after carotid endarterectomy and carotid artery stent placement by using diffusion-weighted imaging. AJNR Am J Neuroradiol. 2005;2:376–84.
Conflict of Interest Statement
Disclosures: All authors state that there is no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Brockmann, C., Seker, F., Weiss, C. et al. Acetylsalicylic Acid Does Not Prevent Digital Subtraction Angiography-Related High Signal Intensity Lesions in Diffusion-Weighted Imaging in Cerebrovascular Patients. Clin Neuroradiol 22, 15–20 (2012). https://doi.org/10.1007/s00062-011-0076-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00062-011-0076-3