Abstract
Sick sinus syndrome (SSS) is a set of diseases with abnormal cardiac pacing, which manifests as diverse cardiac arrhythmias, especially bradycardia. The clinical presentation is inconspicuous in the early stage, but with the progression of this disease, patients may present with symptoms and signs of end-organ hypoperfusion. As a common result in the natural history of the disease, SSS coexisting with atrial fibrillation (AF) forms the basis of bradycardia–tachycardia syndrome. Age-related interstitial fibrosis is considered to be the common pathophysiological mechanism between SSS and AF. The combination of these diseases will adversely affect the condition of patients and the efficiency of subsequent treatment. Although the exact mechanism is not clear to date, the extensive structural and electrical remodeling of the atrium are considered to be the important mechanism for the occurrence of AF in patients with SSS. Pacemaker implantation is the first-line treatment for symptomatic patients with SSS and documented bradycardia history. In view of the adverse effects of AF on the treatment of SSS, researchers have focused on evaluating different pacing modes and algorithms to reduce the risk of AF during pacing. Catheter ablation may also be used as an alternative second-line therapy for some patients with SSS and AF.
Zusammenfassung
Das Syndrom des kranken Sinusknotens („sick sinus syndrome“ [SSS]) setzt sich aus einer Reihe von Erkrankungen mit anomaler Schrittmacherfunktion des Herzens zusammen, was sich in Form verschiedener kardialer Arrhythmien zeigt, insbesondere als Bradykardie. Im Frühstadium sind die klinischen Anzeichen unauffällig, aber mit Fortschreiten der Erkrankung können sich bei den Patienten Symptome einer Endorganhypoperfusion einstellen. Als eine häufige Folge des natürlichen Krankheitsverlaufs bildet das SSS bei gleichzeitigem Vorhofflimmern (VF) die Basis für ein Bradykardie-Tachykardie-Syndrom. Eine altersbezogene interstitielle Fibrose gilt als der gemeinsame pathophysiologische Mechanismus zwischen SSS und VF. Die Kombination dieser Erkrankungen hat negative Auswirkungen auf den Zustand der Patienten und auf die Wirksamkeit der nachfolgenden Behandlung. Zwar ist der genaue Mechanismus bisher noch nicht bekannt, aber das ausgedehnte strukturelle und elektrische Remodeling des Vorhofs werden als die entscheidenden Mechanismen für das Auftreten von VF bei Patienten mit SSS betrachtet. Die Schrittmacherimplantation stellt die Therapie der ersten Wahl bei symptomatischen Patienten mit SSS und dokumentierter Bradykardie in der Vorgeschichte dar. Angesichts der günstigen Auswirkungen von VF auf die Behandlung des SSS lag der Schwerpunkt von wissenschaftlichen Untersuchungen auf der Beurteilung verschiedener Schrittmachermodi und –algorithmen, um das Risiko eines VF während der Schrittmacheraktivität zu vermindern. Als alternative Zweitlinientherapie für manche Patienten mit SSS und VF kann auch eine Katheterablation infrage kommen.
Similar content being viewed by others
References
Rogińska N, Bieganowska K (2014) Sick sinus syndrome: a family study. Cardiol Young 24(1):136–139. https://doi.org/10.1017/s1047951113000991
Kristensen L, Nielsen J, Mortensen P, Pedersen O, Pedersen A et al (2004) Incidence of atrial fibrillation and thromboembolism in a randomised trial of atrial versus dual chamber pacing in 177 patients with sick sinus syndrome. Heart 90(6):661–666
Al-Khatib SM, Stevenson WG, Ackerman MJ, Bryant WJ, Callans DJ et al (2017) 2017 AHA/ACC/HRS guideline for management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: executive summary: a report of the American college of cardiology/American heart association task force on clinical practice Guid. Circulation. https://doi.org/10.1161/CIR.0000000000000548
Adán V, Crown LA (2003) Diagnosis and treatment of sick sinus syndrome. Am Fam Physician 67(8):1725–1732
Shiferaw Y, Aistrup G, Wasserstrom J (2017) Mechanism for triggered waves in atrial myocytes. Biophys J 113(3):656–670. https://doi.org/10.1016/j.bpj.2017.06.026
Yang PS, Kim D, Jang E, Yu HT, Joung B (2021) Risk of sick sinus syndrome in patients diagnosed with atrial fibrillation: a population-based cohort. Authorea. https://doi.org/10.22541/au.161555510.06165605/v1
Dobrzynski H, Boyett M, Anderson R (2007) New insights into pacemaker activity: promoting understanding of sick sinus syndrome. Circulation 115(14):1921–1932. https://doi.org/10.1161/circulationaha.106.616011
Kronborg M, Nielsen J (2012) Pacing in sinus node disease to prevent atrial fibrillation. Expert Rev Cardiovasc Ther 10(7):851–858. https://doi.org/10.1586/erc.12.79
Alonso A, Jensen P, Lopez F, Chen L, Psaty B et al (2014) Association of sick sinus syndrome with incident cardiovascular disease and mortality: the Atherosclerosis Risk in Communities study and Cardiovascular Health Study. Plos One 9(10):e109662. https://doi.org/10.1371/journal.pone.0109662
Lamas GA, Lee KL, Sweeney MO (2002) Ventricular pacing or dual-chamber pacing for sinus-node dysfunction. ACC Curr J Rev. https://doi.org/10.1016/S1062-1458(02)00963-7
Nielsen JC, Thomsen PEB, Hojberg S, Moller M, Vesterlund T et al (2011) A comparison of single-lead atrial pacing with dual-chamber pacing in sick sinus syndrome. Eur Heart J 32(6):686–696
Epstein A, Dimarco J, Ellenbogen K, Estes N, Freedman R et al (2008) ACC/AHA/HRS 2008 guidelines for device-based therapy of cardiac rhythm abnormalities: executive summary. Heart Rhythm 5(6):934–955. https://doi.org/10.1016/j.hrthm.2008.04.015
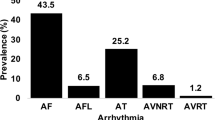
Ciszewski JB, Chwyczko T, Kowalik I, Majda W, Farkowski MM et al (2018) Clinical, echocardiographic, and pacing parameters affecting atrial fibrillation burden in patients with tachycardia-bradycardia syndrome. Kardiol Pol 76(2):338–346. https://doi.org/10.5603/KP.a2017.0207
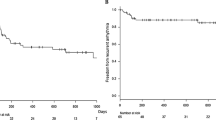
Kim DH, Choi JI, Lee KN, Ahn J, Roh SY et al (2018) Long-term clinical outcomes of catheter ablation in patients with atrial fibrillation predisposing to tachycardia-bradycardia syndrome: a long pause predicts implantation of a permanent pacemaker. BMC Cardiovasc Disord 18(1):106. https://doi.org/10.1186/s12872-018-0834-0
Mangrum JM, DiMarco JP (2000) The evaluation and management of bradycardia. N Engl J Med. https://doi.org/10.1056/NEJM200003093421006
Sanchez-Quintana D, Cabrera JA, Farre J, Climent V, Anderson RH et al (2005) Sinus node revisited in the era of electroanatomical mapping and catheter ablation. Heart 91(2):189–194
Giuseppe BF, Leonelli L et al (2017) P wave and the substrates of arrhythmias originating in the atria. Cardiac Electrophysiology Clinics. https://doi.org/10.1016/j.ccep.2017.05.001
Lin YS, Guo BF, Chen YL, Tsai TH, Chen M‑C (2010) Atrial size independently correlates with the development of paroxysmal atrial fibrillation in patients with sick sinus syndrome. Biomed J 33(6):659–667
Kistler PM, Sanders P, Fynn SP, Stevenson IH, Spence SJ et al (2004) Electrophysiologic and electroanatomic changes in the human atrium associated with age. J Am Coll Cardiol 44(1):109–116
Anyukhovsky EP, Sosunov EA, Alexei P, Gainullin RZ, Jhang JS et al (2002) Cellular electrophysiologic properties of old canine atria provide a substrate for arrhythmogenesis. Cardiovasc Res. https://doi.org/10.1016/S0008-6363(02)00271-7
John RM, Kumar S (2016) Sinus node and atrial arrhythmias. Circulation 133(19):1892–1900
Sparks PB, Jayaprakash S, Vohra JK, Kalman JM (2000) Electrical remodeling of the atria associated with paroxysmal and chronic atrial flutter. Circulation 102(15):1807–1813
Ishikawa T, Ohno S, Murakami T, Yoshida K, Mishima H et al (2017) Sick sinus syndrome with HCN4 mutations shows early onset and frequent association with atrial fibrillation and left ventricular noncompaction. Heart Rhythm 14(5):717–724. https://doi.org/10.1016/j.hrthm.2017.01.020
Jenewein T, Beckmann BM, Rose S, Osterhues HH, Schmidt U et al (2017) Genotype-phenotype dilemma in a case of sudden cardiac death with the E1053K mutation and a deletion in the SCN5A gene. Forensic Sci Int 275:187–194. https://doi.org/10.1016/j.forsciint.2017.02.038
Holm H, Gudbjartsson D, Sulem P, Masson G, Helgadottir H et al (2011) A rare variant in MYH6 is associated with high risk of sick sinus syndrome. Nat Genet 43(4):316–320. https://doi.org/10.1038/ng.781
Monfredi O, Dobrzynski H, Mondal T, Boyett M, Morris G (2010) The anatomy and physiology of the sinoatrial node—a contemporary review. Pacing Clin Electrophysiol 33(11):1392–1406. https://doi.org/10.1111/j.1540-8159.2010.02838.x
Gunes H, Sonmez F, Canga H, Saritas A (2017) An unexpected presentation of sick sinus syndrome: Isolated ventricular asystole. Am J Emerg Med 35(8):1212.e1215–1212.e1216. https://doi.org/10.1016/j.ajem.2017.04.069
Ewy G (2014) Sick sinus syndrome: synopsis. J Am Coll Cardiol 64(6):539–540. https://doi.org/10.1016/j.jacc.2014.05.029
Healey JS, Connolly SJ, Gold MR (2016) Subclinical atrial fibrillation and the risk of stroke. N Engl J Med 374(10):998–998
Amasyali B, Kilic A, Kilit C (2014) Sinus node dysfunction and atrial fibrillation: which one dominates? Int J Cardiol 175(2):379–380
Iwasaki YK, Nishida K, Kato T, Nattel S (2011) Atrial fibrillation pathophysiology: implications for management. Circulation 124(20):2264–2274
Jackson L, Rathakrishnan B, Campbell K, Thomas K, Piccini J et al (2017) Sinus node dysfunction and atrial fibrillation: a reversible phenomenon? Pacing Clin Electrophysiol 40(4):442–450. https://doi.org/10.1111/pace.13030
Elvan A (2001) Sinoatrial remodeling caused by persistent atrial fibrillation: what is the relationship between postcardioversion sinus node dysfunction and increased atrial vulnerability? J Cardiovasc Electrophysiol 12(7):807–808. https://doi.org/10.1046/j.1540-8167.2001.00807.x
Roberts-Thomson KC, Sanders P, Kalman JM (2007) Sinus node disease: an idiopathic right atrial myopathy. Trends Cardiovasc Med 17(6):211–214. https://doi.org/10.1016/j.tcm.2007.06.002
Zhong H, Wang T, Lian G, Xu C, Wang H et al (2018) TRPM7 regulates angiotensin II-induced sinoatrial node fibrosis in sick sinus syndrome rats by mediating Smad signaling. Heart Vessels 33(9):1094–1105. https://doi.org/10.1007/s00380-018-1146-0
Prashanthan S, Joseph BM, Peter MK, Steven JS, Jonathan MK (2004) Electrophysiological and electroanatomic characterization of the atria in sinus node disease evidence of diffuse atrial remodeling. Circulation 109(12):1514–1522. https://doi.org/10.1161/01.CIR.0000121734.47409.AA
Jang SW (2021) Left atrial enlargement and sick sinus syndrome for pacemaker indication were associated with atrial high rate episodes. Korean Circ J 51(3):248–250. https://doi.org/10.4070/kcj.2020.0515
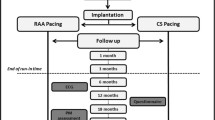
Ramdjan T, van der Does L, Knops P, Res J, de Groot N (2014) Right versus left atrial pacing in patients with sick sinus syndrome and paroxysmal atrial fibrillation (Riverleft study): study protocol for randomized controlled trial. Trials 15:445. https://doi.org/10.1186/1745-6215-15-445
Kochhäuser S, Verma A, Dalvi R, Suszko A, Alipour P et al (2017) Spatial relationships of complex fractionated atrial electrograms and continuous electrical activity to focal electrical sources: implications for substrate ablation in human atrial fibrillation. JACC Clin Electrophysiol 3(11):1220–1228. https://doi.org/10.1016/j.jacep.2017.05.013
Monfredi O, Boyett MR (2015) Sick sinus syndrome and atrial fibrillation in older persons—A view from the sinoatrial nodal myocyte. J Mol Cell Cardiol 83:88–100
Li G, Liu E, Liu T, Wang J, Dai J et al (2011) Atrial electrical remodeling in a canine model of sinus node dysfunction. Int J Cardiol 146(1):32–36. https://doi.org/10.1016/j.ijcard.2009.06.002
Luck J, Engel T (1979) Dispersion of atrial refractoriness in patients with sinus node dysfunction. Circulation 60(2):404–412. https://doi.org/10.1161/01.cir.60.2.404
Guray U, Guray Y, YAlmaz M, Mecit B, Sasmaz H et al (2003) Evaluation of P wave duration and P wave dispersion in adult patients with secundum atrial septal defect during normal sinus rhythm. Int J Cardiol 91(1):75–79. https://doi.org/10.1016/s0167-5273(02)00598-3
Kojodjojo P, Kanagaratnam P, Markides V, Davies D, Peters N (2006) Age-related changes in human left and right atrial conduction. J Cardiovasc Electrophysiol 17(2):120–127. https://doi.org/10.1111/j.1540-8167.2005.00293.x
Letsas KP, Korantzopoulos P, Efremidis M, Weber R, Lioni L et al (2013) Sinus node disease in subjects with type 1 ECG pattern of Brugada syndrome. J Cardiol 61(3):227–231. https://doi.org/10.1016/j.jjcc.2012.12.006
Bocchi F, Marques-Vidal P, Pruvot E, Waeber G, Vollenweider P et al (2020) Clinical and biological determinants of P‑wave duration: cross-sectional data from the population-based CoLaus|PsyCoLaus study. BMJ Open 10(11):e38828. https://doi.org/10.1136/bmjopen-2020-038828
Dinov B, Knopp H, Lobe S, Nedios S, Bode K et al (2016) Patterns of left atrial activation and evaluation of atrial dyssynchrony in patients with atrial fibrillation and normal controls: Factors beyond the left atrial dimensions. Heart Rhythm 13(9):1829–1836. https://doi.org/10.1016/j.hrthm.2016.06.003
Wang M, Tse H, Lee K, Zhang X, Siu C et al (2007) Differential in inter-atrial dyssynchrony and atrial mechanical function in sick sinus syndrome with or without paroxysmal atrial fibrillation. Circulation 116(suppl_16):II_687–II_688. https://doi.org/10.1161/circ.116.suppl_16.II_687-c
Wang M, Lau C, Zhang X, Siu C, Lee K et al (2009) Interatrial mechanical dyssynchrony worsened atrial mechanical function in sinus node disease with or without paroxysmal atrial fibrillation. J Cardiovasc Electrophysiol 20(11):1237–1243. https://doi.org/10.1111/j.1540-8167.2009.01547.x
Ponti RD, Marazzato J, Bagliani G, Leonelli FM, Padeletti L (2018) Sick sinus syndrome. Card Electrophysiol Clin 10(2):183–195. https://doi.org/10.1016/j.ccep.2018.02.002
Andersen H, Thuesen L, Bagger J, Vesterlund T, Thomsen P (1994) Prospective randomised trial of atrial versus ventricular pacing in sick-sinus syndrome. Lancet 344(8936):1523–1528. https://doi.org/10.1016/s0140-6736(94)90347-6
Mattioli A, Vivoli D, Mattioli G (1998) Influence of pacing modalities on the incidence of atrial fibrillation in patients without prior atrial fibrillation. A prospective study. Eur Heart J 19(2):282–286. https://doi.org/10.1053/euhj.1997.0616
Lamas GA, Orav EJ, Stambler BS, Ellenbogen KA, Sgarbossa EB et al (1999) Quality of life and clinical outcomes in elderly patients treated with ventricular pacing as compared with dual-chamber pacing. Surv Anesthesiol 43(1):14
Kim W, Joung B, Shim J, Park J, Hwang E et al (2010) Long-term outcome of single-chamber atrial pacing compared with dual-chamber pacing in patients with sinus-node dysfunction and intact atrioventricular node conduction. Yonsei Med J 51(6):832–837. https://doi.org/10.3349/ymj.2010.51.6.832
Hiroshi M, Yuichi U, Rinya K, Akihiko U, Takashi M et al (2004) Long-term clinical performance of AAI pacing in patients with sick sinus syndrome: a comparison with dual-chamber pacing. Europace 2004(5):5. https://doi.org/10.1016/j.eupc.2004.05.003
Tripp I, Armstrong G, Stewart J, Hood M, Smith W (2005) Atrial pacing should be used more frequently in sinus node disease. Pacing Clin Electrophysiol 28(4):291–294. https://doi.org/10.1111/j.1540-8159.2005.08672.x
Nielsen JC, Kristensen L, Andersen HR, Mortensen PT, Pedersen OL et al (2003) A randomized comparison ofatrial and dual-chamber pacing in177 consecutive patients with sick sinus syndrome: echocardiographic and clinical outcome. J Am Coll Cardiol 42(4):614–623
Pastore G, Marcantoni L, Lanza D, Maines M, Noventa F et al (2021) Occurrence of persistent atrial fibrillation during pacing for sinus node disease: The influence of His bundle pacing versus managed ventricular pacing. J Cardiovasc Electrophysiol 32(1):110–116. https://doi.org/10.1111/jce.14810
Edwards SJ, Karner C, Trevor N, Wakefield V, Salih F (2015) Dual-chamber pacemakers for treating symptomatic bradycardia due to sick sinus syndrome without atrioventricular block: a systematic review and economic evaluation. Health Technol Assess 19(65):1–210. https://doi.org/10.3310/hta19650
DeSilvey D (2008) Minimizing ventricular pacing to reduce atrial fibrillation in sinus node disease. Amer J Geriatric Cardiol 17(1):57–58. https://doi.org/10.1111/j.1076-7460.2007.07671.x
Martin S, Serge B, Javier M, Da CA, Robert H et al (2015) Long-term clinical effects of ventricular pacing reduction with a changeover mode to minimize ventricular pacing in a general pacemaker population. Eur Heart J. https://doi.org/10.1093/eurheartj/ehu336
Botto G, Ricci R, Banzet J, Nielsen J, De Roy L et al (2014) Managed ventricular pacing compared with conventional dual-chamber pacing for elective replacement in chronically paced patients: results of the Prefer for Elective Replacement Managed Ventricular Pacing randomized study. Heart Rhythm 11(6):992–1000. https://doi.org/10.1016/j.hrthm.2014.01.011
Chutani S, Shah A, Kantharia B (2017) Pacing to prevent atrial fibrillation. Curr Opin Cardiol 32(1):22–26. https://doi.org/10.1097/hco.0000000000000355
Boriani G, Tukkie R, Manolis A, Mont L, Santini M et al (2014) Atrial antitachycardia pacing and managed ventricular pacing in bradycardia patients with paroxysmal or persistent atrial tachyarrhythmias: the MINERVA randomized multicentre international trial. Eur Heart J 35(35):2352–2362. https://doi.org/10.1093/eurheartj/ehu165
Calkins H, Hindricks G, Cappato R, Kim Y, Saad E et al (2017) 2017 HRS/EHRA/ECAS/APHRS/SOLAECE expert consensus statement on catheter and surgical ablation of atrial fibrillation: Executive summary. Heart Rhythm 14(10):e445–e494. https://doi.org/10.1016/j.hrthm.2017.07.009
Acknowledgements
The authors would like to acknowledge Prof. Li for support with this review.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
W. Chang and G. Li declare that they have no competing interests.
For this article no studies with human participants or animals were performed by any of the authors. All studies performed were in accordance with the ethical standards indicated in each case.
Rights and permissions
About this article
Cite this article
Chang, W., Li, G. Clinical review of sick sinus syndrome and atrial fibrillation. Herz 47, 244–250 (2022). https://doi.org/10.1007/s00059-021-05046-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00059-021-05046-x
Keywords
- Sick sinus syndrome
- Bradycardia–tachycardia syndrome
- Pacemaker implantation
- Sinus node dysfunction
- Atrial fibrillation