Abstract
Background
Although current guidelines recommend routine use of oral colchicine as a first-line adjunct therapy to aspirin/nonsteroidal anti-inflammatory drugs (NSAIDs) for acute and recurrent pericarditis, there are insufficient data to recommend routine use of colchicine for the initial management of myopericarditis.
Methods
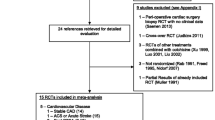
The records of 194 patients who were admitted for myopericarditis were investigated retrospectively. Patients receiving oral colchicine (n = 33) as an adjunct to aspirin/NSAIDs comprised the study group and patients who received conventional therapy (n = 31) formed the control group. Plasma C‑reactive protein (CRP) levels, cardiac biomarkers, and several electrocardiographic parameters of atrial activation were evaluated before the start of treatment and at the 6‑month follow-up.
Results
Assessments before and after treatment with regard to cardiac biomarkers and plasma CRP levels showed improvements in both groups (p > 0.05). There were statistically significant improvements in P wave indices including P wave duration, PR interval length, P wave dispersion, P terminal force, and isoelectric interval in the colchicine therapy group compared with the control group (p < 0.01).
Conclusion
Routine use of colchicine for the initial management of myopericarditis as a first-line adjunct therapy to aspirin/NSAIDs in patients with myopericarditis has favorable effects on electrocardiographic indices of atrial activation parameters.
Zusammenfassung
Hintergrund
Zwar wird in aktuellen Leitlinien die Standardanwendung von Colchicin oral als Ergänzung zur Erstlinientherapie mit Acetylsalicylsäure/nichsteroidalen Antirheumatika (NSAR) bei akuter und rezidivierende Perikarditis empfohlen, aber es stehen nur unzureichend Daten zur Verfügung, um den Routineeinsatz von Colchicin für die initiale Behandlung der Myoperikarditis zu empfehlen.
Methoden
Die Krankenunterlagen von 194 Patienten, die wegen Myoperikarditis stationär aufgenommen worden waren, wurden retrospektiv untersucht. Patienten, die Colchicin oral als Ergänzung zu Acetylsalicylsäure/NSAR erhielten (n = 33), bildeten die Studiengruppe, und Patienten, die konventionell therapiert wurden (n = 31), bildeten die Kontrollgruppe. C‑reaktives Protein (CRP) im Plasma, kardiale Biomarker und verschiedene elektrokardiographische Parameter der Vorhofaktivierung wurden vor Beginn der Behandlung und bei der Nachuntersuchung nach 6 Monaten untersucht.
Ergebnisse
Die Untersuchungen in Bezug auf kardiale Biomarker und CRP im Plasma vor und nach Behandlung ergaben Verbesserungen in beiden Gruppen (p > 0,05). Statistisch signifikante Verbesserungen zeigten sich in der Gruppe mit Colchicintherapie im Vergleich zur Kontrollgruppe (p < 0,01) bei den P‑Wellen-Indizes einschließlich der P‑Wellen-Länge, der Länge des PR-Intervalls, der P‑Wellen-Dispersion, des negativen Anteils der P‑Welle in V1 und des isoelektrischen Intervalls.
Schlussfolgerung
Die Routineanwendung von Colchicin für die initiale Behandlung der Myoperikarditis als Ergänzung der Erstlinientherapie mit Acetylsalicylsäure/NSAR bei Patienten mit Myoperikarditis hat günstige Auswirkungen auf elektrokardiographische Indizes von Parametern der Vorhofaktivierung.


Similar content being viewed by others
References
Caforio AL, Pankuweit S, Arbustini E et al (2013) Current state of knowledge on aetiology, diagnosis, management, and therapy of myocarditis: a position statement of the European society of cardiology working group on myocardial and pericardial diseases. Eur Heart J 34:2636–2648. https://doi.org/10.1093/eurheartj/eht210
Vos T, Barber RM, Bell BG et al (2015) Global burden of disease study 2013 collaborators, global regional, and national incidence, prevelance and years lived with disability for 301 acute and chronic disease and injuries in 188 countries, 1990–2013 a systematic analysis for the global burden of disease study 2013. Lancet 386:743–800. https://doi.org/10.1016/S0140-6736(15)60692-4
Adler Y, Charron P, Imazio M et al (2015) 2015 ESC guidelines for the diagnosis and management of pericardial diseases: the task force for the diagnosis and management of pericardial diseases of the European society of cardiology (ESC) endorsed by: the European association for cardio-thoracic surgery (EACTS). Eur Heart J 36:2921–2964. https://doi.org/10.1093/eurheartj/ehv318
Imazio M, Cooper LT (2013) Management of myopericarditis. Expert Rev Cardiovasc Ther 11:193–201. https://doi.org/10.1586/erc.12.184
Imazio M (2014) Pericarditis with troponin elevation: is it true pericarditis and a reason for concern? J Cardiovasc Med (Hagerstown) 15:73–77. https://doi.org/10.2459/JCM.0b013e328365aa52
Imazio M, Trinchero R (2008) Myopericarditis: etiology, management, and prognosis. Int J Cardiol 127:17–26. https://doi.org/10.1016/j.ijcard.2007.10.053
Imazio M, Brucato A, Trinchero R, Spodick D, Adler Y (2009) Individualized therapy for pericarditis. Expert Rev Cardiovasc Ther 7:965–975. https://doi.org/10.1586/erc.09.82
Imazio M, Cecchi E, Demichelis B et al (2008) Myopericarditis versus viral or idiopathic acute pericarditis. Heart 94:498–501. https://doi.org/10.1136/hrt.2006.104067
Magnani JW, Williamson MA, Ellinor PT, Monahan KM, Benjamin EJ (2009) P wave indices: current status and future directions in epidemiology, clinical, and research applications. Circ Arrhythm Electrophysiol 2:72–79. https://doi.org/10.1161/CIRCEP.108.806828
Kligfield P, Gettes SL, Bailey JJ et al (2007) Recommendations for the standardization and interpretation of the electrocardiogram; part I: the electrocardiogram and its technology: a scientific statement from the American heart association electrocardiography and arrhythmias committee, council on clinical cardiology; the American college of cardiology foundation; and the heart rhythm society: endorsed by the international society for computerized electrocardiology. Circulation 115:1306–1324. https://doi.org/10.1161/CIRCULATIONAHA.106.180200
Imazio M, Brucato A, Ferrazzi P et al (2011) Colchicine reduces postoperative atrial fibrillation: results of the colchicine for the prevention of the postpericardiotomy syndrome (COPPS) atrial fibrillation substudy. Circulation 124:2290–2295. https://doi.org/10.1161/CIRCULATIONAHA.111.026153
Molad Y (2002) Update on colchicine and its mechanism of action. Curr Rheumatol Rep 4:252–256. https://doi.org/10.1007/s11926-002-0073-2
Van Wagoner DR (2011) Colchicine for the prevention of postoperative atrial fibrillation: a new indication for a very old drug? Circulation 124:2281–2282. https://doi.org/10.1161/CIRCULATIONAHA.111.057075
Head BP, Patel HH, Roth DM et al (2006) Microtubules and actin microfilaments regulate lipid raft/caveolae localization of adenylyl cyclase signaling components. J Biol Chem 281:26391–26399. https://doi.org/10.1074/jbc.M602577200
Malan D, Gallo MP, Bedendi I, Biasin C, Levi RC, Alloatti G (2003) Microtubules mobility affects the modulation of L‑type I (Ca) by muscarinic and beta-adrenergic agonists in guinea-pig cardiac myocytes. J Mol Cell Cardiol 35:195–206. https://doi.org/10.1016/s0022-2828(02)00312-7
Nicolas CS, Park KH, El Harchi A et al (2008) IKs response to protein kinase A‑dependent KCNQ1 phosphorylation requires direct interaction with microtubules. Cardiovasc Res 79:427–435. https://doi.org/10.1093/cvr/cvn085
Parker KK, Taylor LK, Atkinson JB, Hansen DE, Wikswo JP (2001) The effects of tubulin-binding agents on stretch-induced ventricular arrhythmias. Eur J Pharmacol 417:131–140. https://doi.org/10.1016/s0014-2999(01)00856-1
Lawani SO, Demerath EW, Lopez FL et al (2014) Birth weight and the risk of atrial fibrillation in whites and African Americans: the atherosclerosis risk in communities (ARIC) study. BMC Cardiovasc Disord 14:69. https://doi.org/10.1186/1471-2261-14-69
Buxton AE, Josephson ME (1981) The role of P wave duration as a predictor of postoperative atrial arrhythmias. Chest 80:68–73. https://doi.org/10.1378/chest.80.1.68
Dilaveris PE, Gialafos EJ, Sideris SK et al (1998) Simple electrocardiographic markers for the prediction of paroxysmal idiopathic atrial fibrillation. Am Heart J 135:733–738. https://doi.org/10.1016/s0002-8703(98)70030-4
Rosiak M, Bolinska H, Ruta J (2002) P wave dispersion and P wave duration on SAECG in predicting atrial fibrillation in patients with acute myocardial infarction. Ann Noninvasive Electrocardiol 7:363–368. https://doi.org/10.1111/j.1542-474x.2002.tb00186.x
Salah A, Zhou S, Liu Q, Yan H (2013) P wave indices to predict atrial fibrillation recurrences post pulmonary vein isolation. Arq Bras Cardiol 101:519–527. https://doi.org/10.5935/abc.20130214
Martín GA, Jiménez CJ, Hernández J, Martín GA, Martín HF, Luengoa CM (2012) P wave morphology and recurrence after cardioversion of lone atrial fibrillation. Rev Esp Cardiol 65(3):289–290. https://doi.org/10.1016/j.recesp.2011.04.023
Kohsaka S, Sciacca RR, Sugioka K, Sacco RL, Homma S, Di Tullio MR (2005) Electrocardiographic left atrial abnormalities and risk of ischemic stroke. Stroke 36:2481–2483. https://doi.org/10.1161/01.STR.0000185682.09981.26
Okin PM, Kamel H, Kjeldsen SE, Devereux RB (2016) Electrocardiographic left atrial abnormalities and risk of incident stroke in hypertensive patients with electrocardiographic left ventricular hypertrophy. J Hypertens 34:1831–1837. https://doi.org/10.1097/HJH.0000000000000989
Imazio M, Lazaros G, Picardi E et al (2015) Incidence and prognostic significance of new onset atrial fibrillation/flutter in acute pericarditis. Heart 101:1463–1467. https://doi.org/10.1136/heartjnl-2014-307398
Author information
Authors and Affiliations
Contributions
Concept – M.D., M.Z.; Design – M.D., M.Z., Y.A. Supervision – Y.A., M.Z.; Resource – M.D., M.Z.; Materials – M.D., M.Z.; Data Collection and/or Processing – M.D., M.Z.; Analysis and/or Interpretation – M.Z., Y.A.; Literature Search – M.D.,Y.A.; Writing – M.D., Y.A.; Critical Reviews – Y.A.
Corresponding author
Ethics declarations
Conflict of interest
M. Duran, Y. Alsancak and M. Ziyrek declare that they have no competing interests.
The study was approved by the local ethics committee (University of Health Sciences, Konya Educational and Research Hospital, Konya, Turkey; 13.09.2019/93/2048 ID number). The investigation conforms to the principles outlined in the Declaration of Helsinki.
Rights and permissions
About this article
Cite this article
Duran, M., Alsancak, Y. & Ziyrek, M. Effects of oral colchicine administration as first-line adjunct therapy in myopericarditis. Herz 47, 166–174 (2022). https://doi.org/10.1007/s00059-021-05040-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00059-021-05040-3
Keywords
- Acetylsalicylic acid
- Cardiac biomarkers
- Myopericarditis
- Nonsteroidal anti-inflammatory agent
- P wave indices