Abstract
Background
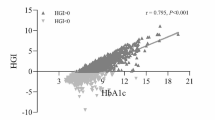
Blood glucose levels are associated with the prognosis of patients with acute coronary syndrome (ACS). Glycated hemoglobin (HbA1c) reflects the average blood glucose level. The purpose of the study was to evaluate HbA1c as a prognostic indicator for ACS.
Methods
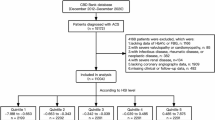
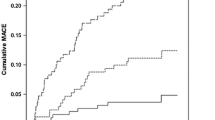
In total, 27,337 ACS patients from the CCC-ACS (Improving Care for Cardiovascular Disease in China - Acute Coronary Syndrome) project were enrolled in this study and divided into three groups according to HbA1c level: Group I, HbA1c level <5.7%; Group II, HbA1c level 5.7–6.4%; Group III, HbA1c level ≥6.5%. The primary outcome was an in-hospital major adverse cardiovascular event (MACE), such as all-cause death, recurrent myocardial infarction, acute or subacute stent thrombosis, heart failure, cardiogenic shock, or cardiac arrest. Baseline data and effectiveness outcome were compared among patients in the three groups.
Results
Group III had the highest MACE incidence (13.4% [Group III] vs. 8.7% [Group I] and 10.5% [Group II], p < 0.001). In the logistic regression, there was a statistically significant difference in HbA1c level between the groups (odds ratio [OR]: 1.110, 95% confidence interval [CI]: 1.008–1.133, p < 0.001). In the receiver operating characteristic curve, the area under the curve for MACE was 0.560 (95% CI: 0.550–0.571, p < 0.001); the cut-off value for the HbA1c level was 6.38%.
Conclusion
The HbA1c level was associated with the risk of MACEs in ACS patients with or without diabetes.
Trial Registration clinicaltrials.gov, NCT02306616. Registered 3 December 2014—Retrospectively registered, https://clinicaltrials.gov/ct2/show/NCT02306616.
Zusammenfassung
Hintergrund
Der Blutzuckerspiegel steht in einem Zusammenhang mit der Prognose von Patienten mit akutem Koronarsyndrom (ACS). Das glykierte Hämoglobin (HbA1c) ist ein Marker für den durchschnittlichen Blutzuckerspiegel. Ziel der vorliegenden Studie war es, HbA1c als prognostischen Indikator des ACS zu untersuchen.
Methoden
In die vorliegende Studie wurden 27.337 ACS-Patienten aus dem CCC-ACS-Projekt (Improving Care for Cardiovascular Disease in China – Acute Coronary Syndrome) einbezogen und nach ihrem HbA1c-Wert in 3 Gruppen eingeteilt: Gruppe I mit einem HbA1c-Wert <5,7 %; Gruppe II mit einem HbA1c-Wert von 5,7–6,4 %; Gruppe III mit einem HbA1c-Wert ≥6,5 %. Primärer Endpunkt war ein schweres kardiovaskuläres unerwünschtes Ereignis im Krankenhaus (MACE), wie Tod aus sämtlichen Ursachen, Rezidiv eines Herzinfarkts, akute oder subakute Stentthrombose, Herzinsuffizienz, kardiogener Schock oder Herzstillstand. Die Ausgangsdaten und das Ergebnis hinsichtlich der Wirksamkeit wurden zwischen den Patienten in den 3 Gruppen verglichen.
Ergebnisse
Die höchste MACE-Inzidenz bestand in Gruppe III (13,4 % [Gruppe III] vs. 8,7 % [Gruppe I] und 10,5 % [Gruppe II]; p < 0,001). Im Rahmen der logistischen Regression gab es zwischen den Gruppen eine statistisch signifikante Differenz beim HbA1c-Wert (Odds Ratio, OR: 1,110; 95 %-Konfidenzintervall, 95 %-KI: 1,008–1,133; p < 0,001). In der Receiver-Operating-Characteristic-Kurve betrug die Fläche unter der Kurve für MACE 0,560 (95 %-KI: 0,550–0,571; p < 0,001); der Grenzwert für den HbA1c-Wert lag bei 6,38 %.
Schlussfolgerung
Der HbA1c-Wert weist einen Zusammenhang mit dem Risiko für MACE bei ACS-Patienten mit oder ohne Diabetes mellitus auf. Studienregistrierung: clinicaltrials.gov, NCT02306616. Registrierung 3. Dezember 2014 – retrospektiv registriert, https://clinicaltrials.gov/ct2/show/NCT02306616.


Similar content being viewed by others
Abbreviations
- ACEI:
-
Angiotensin-converting enzyme inhibitor
- ACS:
-
Acute coronary syndrome
- AMI:
-
Acute myocardial infarction
- ARB:
-
Angiotensin receptor blocker
- AUC:
-
Area under the curve
- CAD:
-
Coronary atherosclerotic disease
- CCC-ACS:
-
Improving Care for Cardiovascular Disease in China—Acute Coronary Syndrome
- CI:
-
Confidence interval
- CVD:
-
Cardiovascular disease
- DM:
-
Diabetes mellitus
- GFR:
-
Glomerular filtration rate
- GRACE:
-
Global Registry of Acute Coronary Events
- HbA1c:
-
Glycated hemoglobin
- LDL‑C:
-
Low-density lipoprotein cholesterol
- MACE:
-
Major adverse cardiovascular event
- NSTE-ACS:
-
Non-ST-elevation ACS
- NSTEMI:
-
Non-ST-elevation myocardial infarction
- OR:
-
Odds ratio
- PCI:
-
Percutaneous coronary intervention
- ROC:
-
Receiver operating characteristic
- SBP:
-
Systolic blood pressure
- SD:
-
Standard deviation
- STEMI:
-
ST-elevation myocardial infarction
- UA:
-
Unstable angina
References
Gunnar RM, Bourdillon PD, Dixon DW et al (1990) ACC/AHA guidelines for the early management of patients with acute myocardial infarction. A report of the American college of cardiology/American heart association task force on assessment of diagnostic and therapeutic cardiovascular procedures (subcommittee to develop guidelines for the early management of patients with acute myocardial infarction). Circulation 82(2):664–707
Fox KA, Dabbous OH, Goldberg RJ et al (2006) Prediction of risk of death and myocardial infarction in the six months after presentation with acute coronary syndrome: prospective multinational observational study (GRACE). BMJ 333(7578):10
Karounos M, Chang AM, Robey JL et al (2007) TIMI risk score: does it work equally well in both males and females? Emerg Med J 24(7):471–474
Timmer JR, Hoekstra M, Nijsten MW et al (2011) Prognostic value of admission glycosylated hemoglobin and glucose in nondiabetic patients with ST-segment-elevation myocardial infarction treated with percutaneous coronary intervention. Circulation 124(6):704–711
Liu Y, Yang YM, Zhu J et al (2012) Haemoglobin A(1c), acute hyperglycaemia and short-term prognosis in patients without diabetes following acute ST-segment elevation myocardial infarction. Diabet Med 29(12):1493–1500
Selvin E, Steffes MW, Zhu H et al (2010) Glycated hemoglobin, diabetes, and cardiovascular risk in nondiabetic adults. N Engl J Med 362(9):800–811
Bjarnason TA, Hafthorsson SO, Kristinsdottir LB et al (2019) The prognostic effect of known and newly detected type 2 diabetes in patients with acute coronary syndrome. Eur Heart J Acute Cardiovasc Care 20:2048872619849925
Chen CL, Yen DH, Lin CS et al (2017) Glycated hemoglobin level is an independent predictor of major adverse cardiac events after nonfatal acute myocardial infarction in nondiabetic patients: a retrospective observational study. Medicine 96(18):6743
Rasoul S, Ottervanger JP, Bilo HJ et al (2007) Glucose dysregulation in nondiabetic patients with ST-elevation myocardial infarction: acute and chronic glucose dysregulation in STEMI. Neth J Med 65(3):95–100
Noguchi K, Sakakibara M, Asakawa N et al (2016) Higher hemoglobin A1c after discharge is an independent predictor of adverse outcomes in patients with acute coronary syndrome—findings from the PACIFIC registry. Circ J 80(7):1607–1614
Tian L, Zhu J, Liu L et al (2013) Hemoglobin A1c and short-term outcomes in patients with acute myocardial infarction undergoing primary angioplasty: an observational multicenter study. Coron Artery Dis 24(1):16–22
Britton KA, Aggarwal V, Chen AY et al (2011) No association between hemoglobin A1c and in-hospital mortality in patients with diabetes and acute myocardial infarction. Am Heart J 161(4):657–663
Chan CY, Li R, Chan JY et al (2011) The value of admission HbA(1c) level in diabetic patients with acute coronary syndrome. Clin Cardiol 34(8):507–512
Hao Y, Liu J, Smith SC Jr et al (2016) Rationale and design of the improving care for cardiovascular disease in China (CCC) project: a national effort to prompt quality enhancement for acute coronary syndrome. Am Heart J 179:107–115
American Diabetes Association (2018) Classification and diagnosis of diabetes: standards of medical care in diabetes-2018. Diabetes Care 41(1):S13–S27
Woodman RJ, Chew GT, Watts GF (2005) Mechanisms, significance and treatment of vascular dysfunction in type 2 diabetes mellitus: focus on lipid-regulating therapy. Drugs 65(1):31–74
Koracevic G, Vasiljevic S, Velickovic-Radovanovic R et al (2014) Stress hyperglycemia in acute myocardial infarction. Vojnosanit Pregl 71(9):858–869
Gabbay KH, Hasty K, Breslow JL et al (1977) Glycosylated hemoglobins and long-term blood glucose control in diabetes mellitus. J Clin Endocrinol Metab 44(5):859–864
Dunn PJ, Cole RA, Soeldner JS et al (1979) Reproducibility of hemoglobin AIc and sensitivity to various degrees of glucose intolerance. Ann Intern Med 91(3):390–396
El-Sherbiny I, Nabil B, Saber T et al (2015) Impact of admission glycosylated hemoglobin A1c on angiographic characteristics and short term clinical outcomes of nondiabetic patients with acute ST-segment elevation myocardial Infarction. Cardiol Res Pract 2015:274892
Liu XJ, Wan ZF, Zhao N et al (2015) Adjustment of the GRACE score by hemoglobinA1c enables a more accurate prediction of long-term major adverse cardiac events in acute coronary syndrome without diabetes undergoing percutaneous coronary intervention. Cardiovasc Diabetol 14:110
Riddle MC, Ambrosius WT, Brillon DJ et al (2010) Epidemiologic relationships between A1C and all-cause mortality during a median 3.4-year follow-up of glycemic treatment in the ACCORD trial. Diabetes Care 33(5):983–990
Suzuki K, Takano H, Kubota Y et al (2016) Plaque characteristics in coronary artery disease patients with impaired glucose tolerance. PLoS ONE 11(12):e167645
De Rosa R, Vasa-Nicotera M, Leistner DM et al (2017) Coronary atherosclerotic plaque characteristics and cardiovascular risk factors—insights from an optical coherence tomography study. Circ J 81(8):1165–1173
Zhang S, Dai J, Jia H et al (2018) Non-culprit plaque characteristics in acute coronary syndrome patients with raised hemoglobinA1c: an intravascular optical coherence tomography study. Cardiovasc Diabetol 17(1):90
Dhar I, Dhar A, Wu L et al (2012) Arginine attenuates methylglyoxal- and high glucose-induced endothelial dysfunction and oxidative stress by an endothelial nitric-oxide synthase-independent mechanism. J Pharmacol Exp Ther 342(1):196–204
Pickup JC, Mattock MB, Chusney GD et al (1997) NIDDM as a disease of the innate immune system: association of acute-phase reactants and interleukin‑6 with metabolic syndrome X. Diabetologia 40(11):1286–1292
Fukuhara M, Matsumura K, Wakisaka M et al (2007) Hyperglycemia promotes microinflammation as evaluated by C‑reactive protein in the very elderly. Intern Med 46(5):207–212
Buraczynska M, Zukowski P, Drop B et al (2016) Effect of G(-174)C polymorphism in interleukin‑6 gene on cardiovascular disease in type 2 diabetes patients. Cytokine 79:7–11
Lemkes BA, Hermanides J, Devries JH et al (2010) Hyperglycemia: a prothrombotic factor? J Thromb Haemost 8(8):1663–1669
Acknowledgements
We acknowledged all participating hospitals for their contributions to the CCC-ACS project (Table S1).
Funding
The Improving Care for Cardiovascular Disease in China CCC-ACS project is a collaborative study of the American Heart Association (AHA) and Chinese Society of Cardiology (CSC). The AHA was funded by Pfizer for the quality improvement initiative through an independent grant for learning and change. This work was also supported by the Cardiacare Sponsored Optimizing Antithrombotic Research Fund (BJUHFCSOARF201801-05) and Liaoning Provincial Key Research and Development Program (2018225001).
Author information
Authors and Affiliations
Consortia
Contributions
YK and XZ conceptualized and designed the study; YK statistically analyzed the data; YK and XZ wrote the manuscript. XZ had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. All authors were involved in the analysis or interpretation of data. All authors read and approved the final manuscript. All authors gave final approval for this version to be published.
Corresponding author
Ethics declarations
Conflict of interest
X. Zhao, Y. Kang, X. Wang, X. Yang, G. Ai, Y. Liu, P. Xu, J. Zhang, C. Gu, Y. Zhang, Y. Hao, D. Zhao, and Y. Han declare that they have no competing interests.
Institutional review board approval was granted for the aggregate dataset for research and quality improvement by the Ethics Committee of Beijing An Zhen Hospital, Capital Medical University. Participating sites were granted a waiver of patient consent under the common rule. Thirty-nine sites received institutional review board approval from their own ethics committees, with the other 111 sites accepting central ethics approval. The study is listed at www.clinicaltrials.gov (NCT02306616).
Additional information
Xin Zhao and Yi Kang contributed equally to the manuscript.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the CCC-ACS project.
Code availability
The statistical analyses were used the IBM SPSS program (Version 23.0).
Caption Electronic Supplementary Material
Rights and permissions
About this article
Cite this article
Zhao, X., Kang, Y., Wang, X. et al. Clinical significance of glycated hemoglobin in acute coronary syndrome patients from the CCC-ACS project. Herz 46 (Suppl 2), 287–294 (2021). https://doi.org/10.1007/s00059-020-04999-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00059-020-04999-9