Abstract
Background
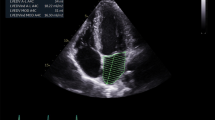
Diastolic dysfunction (DD) in transthoracic echocardiography (TTE), which is a poorly understood entity due to its limited treatment, is frequently encountered in daily clinical practice of cardiology. An electrocardiographic (ECG) index to predict echocardiographic DD has not been elucidated yet. We aim to exhibit an electrocardiographic diastolic index (EDI) to predict TTE DD with high sensitivity and specificity.
Materials and methods
In this retrospective investigation, we tested the DD predictive value of EDI [aVL R amplitude × (V1S amplitude + V5R amplitude)/D1 P amplitude] on 204 consecutive adult patients without known coronary artery disease. Patients were divided into tertiles according to their EDI starting from the lowest one. The power of the EDI was also compared with the subunits of its formula by a receiver operating curve (ROC) analysis.
Results
After adjustment for confounding baseline variables, EDI in tertile 3 was associated with 24.2-fold hazard ratio of DD (odds ratio 25.2, 95% confidence interval [CI] 11.2–51.1, p < 0.001). The Spearman correlation analysis revealed moderate correlation between E/e′ and EDI. A ROC analysis showed that the optimal cut-off value of the EDI to predict DD was 8.53 mV with 70% sensitivity and 70% specificity (area under the curve 0.78; 95% CI 0.71–0.84; p < 0.001).
Conclusion
The electrocardiographic diastolic index (EDI), which is an inexpensive, feasible, and easy to use formula, appears to have a considerable role to predict diastolic dysfunction (DD) in adult patients.
Zusammenfassung
Hintergrund
Die diastolische Dysfunktion (DD) in der transthorakalen Echokardiographie (TTE), die aufgrund ihrer begrenzten Behandlungsmöglichkeiten nur unzureichend verstanden wird, ist in der täglichen klinischen Praxis der Kardiologie häufig anzutreffen. Ein elektrokardiographischer (EKG) Index zur Vorhersage der echokardiographischen DD ist bisher noch nicht geklärt. Ziel dieses Beitrags ist es, einen elektrokardiographischen diastolischen Index (EDI) zur Vorhersage der TTE DD mit hoher Sensitivität und Spezifität aufzuzeigen.
Materialien und Methoden
In dieser retrospektiven Untersuchung wurde der DD-Prädiktionswert von EDI [aVL R‑Amplitude × (V1S-Amplitude + V5R-Amplitude)/D1 P‑Amplitude] an 204 konsekutiven erwachsenen Patienten ohne bekannte koronare Herzkrankheit getestet. Die Patienten wurden entsprechend ihrem EDI in Terzile eingeteilt, beginnend mit dem niedrigsten. Die Leistung des EDI wurde auch mit den Untereinheiten von dessen Formel durch eine Analyse der Receiver-operating-characteristic(ROC)-Kurve verglichen.
Ergebnisse
Nach Bereinigung konfundierender Baseline-Variablen war der EDI im 3. Terzil mit der 24,2-fachen Hazard-Ratio von DD assoziiert (Odds-Ratio: 25,2, 95 % Konfidenzintervall [KI] 11,2–51,1; p < 0,001). Die Spearman-Korrelationsanalyse ergab eine moderate Korrelation zwischen E/e′ und EDI. Eine ROC-Analyse zeigte, dass der optimale Cut-off-Wert des EDI zur Vorhersage der DD bei 8,53 mV mit 70 % Sensitivität und 70 % Spezifität lag („area under the curve“: 0,78; 95 % KI 0,71–0,84; p < 0,001).
Schlussfolgerung
Der elektrokardiographische diastolische Index (EDI), der eine kostengünstige, praktikable und einfach anzuwendende Formel darstellt, scheint eine beträchtliche Rolle bei der Vorhersage der diastolischen Dysfunktion (DD) bei erwachsenen Patienten zu spielen.



Similar content being viewed by others
References
Nagueh SF, Smiseth OA, Appleton CP et al (2016) Recommendations for the Evaluation of Left Ventricular Diastolic Function by Echocardiography: An Update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr 29:277–314
Sanchis L, Andrea R, Falces C, Poyatos S, Vidal B, Sitges M (2018) Differential clinical implications of current recommendations for the evaluation of left ventricular diastolic function by echocardiography. J Am Soc Echocardiogr 3:1203–1208
Toida T, Toida R, Yamashita R et al (2019) Grading of left ventricular diastolic dysfunction with preserved systolic function by the 2016 American Society of Echocardiography/European Association of cardiovascular imaging recommendations contributes to predicting cardiovascular events in hemodialysis patients. Cardiorenal Med 9:190–200
de Lemos JA, McGuire DK, Drazner MH (2003) B‑type natriuretic peptide in cardiovascular disease. Lancet 362:316–322
Dokainish H (2007) Combining tissue Doppler echocardiography and B‑type natriuretic peptide in the evaluation of left ventricular filling pressures: review of the literature and clinical recommendations. Can J Cardiol 23:983–989
Krepp JM, Lin F, Min JK, Devereux RB, Okin PM (2014) Relationship of electrocardiographic left ventricular hypertrophy to the presence of diastolic dysfunction. Ann Noninvasive Electrocardiol 19:552–560
Tan ES, Chan SP, Xu CF et al (2019) Cornell product is an ECG marker of heart failure with preserved ejection fraction. Heart Asia 11:e11108
Park JK, Park J, Uhm JS, Joung B, Lee MH, Pak HN (2016) Low P‑wave amplitude (〈0.1 mV) in lead I is associated with displaced inter-atrial conduction and clinical recurrence of paroxysmal atrial fibrillation after radiofrequency catheter ablation. Europace 18:384–391
Schiller NB, Shah PM, Crawford M, DeMaria A, Devereux R, Feigenbaum H, Gutgesell H, Reichek N, Sahn D, Schnittger I (1989) Recommendations for quantitation of the left ventricle by two dimensional echocardiography. American Society of Echocardiography Committee on Standards, Subcommittee on Quantitation of Two-Dimensional Echocardiograms. J Am Soc Echocardiogr 2:358–367
Andrade J, Khairy P, Dobrev D, Nattel S (2014) The clinical profile and pathophysiology of atrial fibrillation: relationships among clinical features, epidemiology, and mechanisms. Circ Res 114:1453–1468
Vogel MW, Slusser JP, Hodge DO, Chen HH (2012) The natural history of preclinical diastolic dysfunction: a population-based study. Circ Heart Fail 5:144–151
Jarasunas J, Aidietis A, Aidietiene S (2018) Left atrial strain—an early marker of left ventricular diastolic dysfunction in patients with hypertension and paroxysmal atrial fibrillation. Cardiovasc Ultrasound 16:29
Alexander B, Haseeb S, van Rooy H et al (2017) Reduced P‑wave voltage in lead I is associated with development of atrial fibrillation in patients with coronary artery disease. J Atr Fibrillation 10:1657
Sokolow M, Lyon TP (1949) The ventricular complex in left ventricular hypertrophy as obtained by unipolar precordial and limb leads. Am Heart J 37:161–186
Casale PN, Devereux RB, Alonso DR, Campo E, Kligfield P (1987) Improved sex-specific criteria of left ventricular hypertrophy for clinical and computer interpretation of electrocardiograms: validation with autopsy findings. Circulation 75:565–572
Nagueh SF, Appleton CP, Gillebert TC et al (2009) Recommendations for the evaluation of left ventricular diastolic function by echocardiography. J Am Soc Echocardiogr 22:107–133
Huurman R, Boiten HJ, Valkema R, van Domburg RT, Schinkel AF (2015) Eight-year prognostic value of QRS duration in patients with known or suspected coronary artery disease referred for myocardial perfusion imaging. Am J Cardiol 116:1329–1333
Karahan Z, Yaylak B, Uğurlu M, Kaya İ, Uçaman B, Öztürk Ö (2015) QRS duration: a novel marker of microvascular reperfusion as assessed by myocardial blush grade in ST elevation myocardial infarction patients undergoing a primary percutaneous intervention. Coron Artery Dis 26:583–586
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
M.İ. Hayıroğlu, T. Çınar, V. Çiçek, S. Asal, Ş. Kılıç, N. Keser, M. Uzun and A.L. Orhan declare that they have no competing interests.
This article does not contain any studies with human participants or animals performed by any of the authors.
Rights and permissions
About this article
Cite this article
Hayıroğlu, M.İ., Çınar, T., Çiçek, V. et al. A simple formula to predict echocardiographic diastolic dysfunction—electrocardiographic diastolic index. Herz 46 (Suppl 2), 159–165 (2021). https://doi.org/10.1007/s00059-020-04972-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00059-020-04972-6